Rheumatology
advertisement

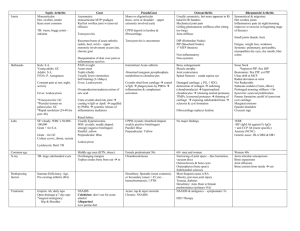
Or me to go back Rheumatology Dan Cushman 2007 Note: Hit me to advance to the next slide Joints What type of Articular (hyaline) cartilage are cartilage bones covered by? What’s special It secretes about the synovial synovial fluid! membrane? Which parts of the joint Cartilage are not & covered intraarticular by the fibrocartilage synovial membrane (2)? How long does it take for the It never fully articular cartilage regenerates to fully regenerate? Synovial Fluid Is there a high or a What types of Synovial low proteinCan cells secrete What It provides is the point Low protein fibroblasts be contentarthrocenteses in synovial hyaluronic acid? viscosityacid? Yep, if you’re good of hyaluronic performed on fluid (SF)? at it patients with coagulopathies? What’s the main A vasovagal risk of Immuneepisode What are arthrocentesis? the main surveillance, three purposes of supply nutrients, SF? remove wastes It is happens digestedtoby What the enzymesacid hyaluronic content during a Why Real menbranes is the decreased Because it lacks a pathological process? synovial cry when viscosity don’t true basement membrane you bump your not a membrane real membrane? knee Culture! What else should When is it “NonWhatWBC would <= fat you test for?inflammatory?” globules2000 suggest? Synovial Fluid Cloudy Yellow Red Low >> 20,000 = Periph blood None Oh yeah None Septic >20,000 >50,000 Normal Cloudy Yellow Cloudy Yellow None • RBC <200 per uL • WBC High • Viscosity Clear Yellow • Color A fracture Inflamm Bloody Gouty Acute Phase Reactants What causes them What are the main toInflammatory increase in the ESR and CRP states two tests? blood? Which They’re disease not are APRsspecific specific for? Plasma proteins What created arebythey? the liver Fever, neuroendocrine What can they effects, cause? behavioral changes, etc. Cytokines What molecules (IL-6, IL1, TNF-α, cause the IFN-β, TGF-β, increase? etc.) C-Reactive Protein What is the main Bind to (presumed) phosphocholine? C-Reactive Protein function of CRP? C-Reactive Protein Run Is CRP considered Because it could Why would youpart of the innate be a way to want to bind to or Innate humoral recognize foreign phosphocholine? pathogens immune system? To recognize the phospholipid Activates the Why else? constituents of When complement bound, damaged cells what system does and/or CRP Is it rapid Rapid or slow? bind to do? phagocytic cells Erythrocyte Sedimentation Rate What molecule largely is Fibrinogen responsible for the ESR? Which changes moreThe quickly CRP– the ESR or the CRP? Is it a direct or indirect measure of theIndirect acute phase protein concentrations? How can the red By their shape, cells affect the size, and number ESR? Rheumatoid Factor Yes – it’s a known Is it marker; even related RF+ to patients rheumatoid have more arthritis? aggressive RA Which isotype is most commonly IgM identified by testing? An auto-antibody to the What’s Fc portion RF? of IgG What is its role in the immunopathology Unknown of rheumatoid arthritis? CCP Antibodies It’sWhich seen inisthe early important… stages of why? RA Antibodies to Cyclic What’re Citrullinated those? Peptide It’s seen almost Which is exclusively in RA important… why? patients AWhat’s form of citrulline? arginine At what level is someone Serum urate considered to above 6.8mg/dL have hyperuricemia? What type of nucleic acid can Purines lead to increased uric acid levels? What Inflammatory would the (>2000) WBC count – usually be in between in the synovial 20,000 Is there andfluid? 100,000 inflammation Yep present? Gout Which Adenosine onesand are purines guanine again? Which The joint first is most metatarsal commonly phalangeal affected? (MTP) What Negatively would the crystals birefringent look like? What type of crystals Monosodium deposit into urate tissues in gout? Xanthine Oxidase What is the final enzyme in purine degradation? Dietary purines Tissue nucleic acids Endogenous purine synthesis Urate Overproduction Underexcretion Proximal tubules The Hyperuricemia Cascade Where does most of the urate reabsorption occur in the kidney? Hyperuricemia Silent tissue deposition Gout Renal manifestations Associated cardiovascular events and mortality Gout Which Too high; is a obesity worse – a is BMI a comorbid that is too highcondition or too low? >3 attacks/year, tophaceous gout, Who should get urate What shape are allopurinol? Needle-shaped nephropathy, the urate crystals? More males or urate > 12 mg/dL Males females? What three Lose weight, eat lifestyle less modifications meat/seafood, should be NSAIDs, canlow-dose be done drink less alcoholWhich What type recommended? prophylactically? oralofcolchicine alcohol Beeris the Which three drugs Cyclosporines, lowdoseincrease aspirin, and worst? can the diuretics risk? Gout Where is gout present? You can be sure that this guy is gout-free, though. Where is the pig who ate roast beef? That is a direct contradiction, because roast beef should cause gout (increased purine intake). What are Asymptomatic intervals between “intercritical acute flares segments” Gout Where do Joints monosodium and soft How Decreased can diuretics urate crystals tissues tend to What food should cause excretion gout? What’s the most accumulate? is lead LeadHow bekidneys avoided if you Alcohol lapseUnderexcretion of common general of Meat. decreased associated urate with don’t want to I mean, mechanism judgement urate for How can alcohol excretion gout? have gout? underexcretion of promiscuity contracting gout? cause gout? STGurate (sexually No, there is hidden transmitted gout) Are intercritical damage that can What are two occur duringsafe? those Increased ATP sgements mechanisms that periods Who told I did. you so? LowerHow pH, lower ↓ solubility, joint/soft could tissue degradation How can could cause temperature tissue disturbances, underperfusion increased precipitation of decreased reabsorption of water exacerbate adenosinegout? crystals occur (3)? solubility? supersaturation increased urate Pseudogout – six causes 1. 2. 3. 4. 5. 6. Hemochromatosis Hyperparathyroidism Hypophosphatemia/-magnesemia Familial Hypocalciuria/-emia Aging Thyroid Disease Calcium oxalate, What other types calcium are possible? hydroxyapatite Pseudogout Inflammation What type of Yep present? birefringence Positive do crystals have? Whatthe is chronic NSAIDs, Calcium Pseudo-What type of polyarticular Colchicine, Pyrophosphate rheumatoid What’s the arthritisDihydrate alsocrystals? steroids, (CPPD) treatment arthritis (4)? called? underlying disease Is the ROM of It’s painful treatment preserved? Where does it most Wristcommonly and knee Is the Negative, synovial butcell What is the WBC occur? culture there can usually be a count >2000 in the concurrent positive or synovial fluid? negative? infection Osteomyelitis What are two Trauma contamination; other routes of contiguous infection? spread What are the most What is commonly common Staph aureus bacteria and apparent before Bacteremia Strep involved pyogenes in acute osteomyelitis? What is the most osteomyelitis? common Hematologic route of infection? Why should children be They harbor treated differently different bacteria with osteomyelitis? Osteomyelitis IV antibiotics, surgical How is it treated? What is the debridement & Where do children Whatstabilization are two Bone definitive biopsy & Long most bones often of the diagnostic diseases that can culture test for Pott’s disease, TB present extremities with cause spinal ostemyelitis? osteomyelitis? osteomyelitis? Where do adults most commonly The vertebrae present with osteomyelitis? Fever, chills, Back pain, spine What symptoms malaise, How do localized they tenderness, loware present? pain, present? erythema, grade fever warmth, edema Where do adults usually get The knee infectious arthritis? Infectious Arthritis Rapid – it’s a Rapid medical or slow? emergency! Previous damage, prosthetics, IV drug What are the main use, 4 risk factors? immunocompromised patients Most common Hematogenous route of infection? How It long canuntil be the joint permanent regains its function? damage! Damage can occur How fast? within a few hours The Where knee;dobut kids the hip usually is more get Yes, but most common infectious than inCan it be chronic? commonly acute arthritis? adults Contiguous, How else can direct it inoculation spread? Infectious Arthritis Are the symptoms localized Both or systemic? What is the most common Gonococcal cause of arthritis arthritis in sexually active adults? What are the three most Knee, wrist, hand common sites affected? Is it considered autoimmune Both or infectious? What Staph areaureus, the main Strep three pyogenes, bacteria H. responsible? influenzae What would the WBC > 10,000; fluid Is it more commonsynovial >80% polys Women in men or women? show? Skeletal What homeostasis, are the three mineral main functions homeostasis, ofphysis bone? Is the hematopoiesis metabolically Active Bone YesCan – without bone Is the physis regenerate scars itself? stronger or Weaker weaker than When can a regular bone? active or inactive? fracture Neoplasm, be a result endocrinopathy of another inherent process? Infection, What complications compartment can When does bone occur syndrome, with a In which part of calcification In utero The bone physis does fracture thrombosis (3)? the begin? growth occur? Bone Comminuted 1 2 3 2 Simple Open Growing Bone 3 4 1 5 2 6 7 8 9 Fractures – identify location Type I Type II Type III Type IV Type V The tissue is Then…? calcified What Precise are the reapproximation physician’s two of goals the fracture of the & primary rigid stage of immobilization bone healing? Inflammation & Then…? angiogenesis Bone What happens Hematoma first in secondary forms fracture healing? Deposition What is of thenew boneprimary across the physiology fracture byof bone osteoblasts healing? Blood vessels invade A primitive scar is Then…? Then…? formation of formed scar normal bone! Bone healing – Steps Early Fracture Inflammation Repair Remodelling Bone Healing – Three Processes 1. Inflammatory 2. Reparative 3. Remodelling When does each stage occur? Bone Healing – Six Stages 1. 2. 3. 4. 5. 6. Hematoma Inflammatory Formation of granulation tissue Soft callus formation Hard callus formation Remodelling Hours – days Begins < 48 hours 2-12 days 1 week – months 1 week – months Several months Ewing sarcoma DIAPHYSIS Name the tumor! Chondrosarcoma Chondroma Osteochondroma METAPHYSIS EPIPHYSEAL PLATE EPIPHYSIS Osteosarcoma Giant cell tumor What Myeloma, are the lymphoma, three most common metastatic bone carcinoma tumors? Bone Tumors What’s the capital of theLome country of Togo? What’s the most common Osteosarcoma type of sarcoma? Malignant neoplasm What is aof mesenchymal sarcoma? tissue What do the lesions Multiple of multiple lytic myeloma lesionslook like? Bone Tumors Tumor Origin Osteo(-sarcoma, …) Bone ? Chondro(-sarcoma, …) Cartilage ? Chordoma Notochord ? Ewing sarcoma Unknown ? Giant Cell Fibroma Bone ? ? Osteosarcoma 10-20 Age? BodyKnee location? Bone Metaphysis location? LevelHigh-grade of malignancy? Sunburst, Codman Radiologic findings? Triangle Produces? Osteoid Osteoma Age? 60 ? Skull Body andlocation? facial bones Level ofBenign malignancy? Osteoid Osteoma ? Body Longlocation? bones Bone Cortex, location? <2cm Aspirin Treatment at night Osteoblastoma BodySpine location? >2cm in Size? diameter Chondrosarcoma ? 50-70 Age? Pelvis, proximal femur, Body location? shoulder, ribs LevelLow-grade of malignancy? Dedifferentiation Notable finding? Chondroma 30-50 Age? Hands/feet, humerus, Body location? femur ? Level ofBenign malignancy? X-rays Radiologic mustimportance? be reviewed ? Osteochondroma 10-30 Age? Femur, humerus, tibia, Body location? fibula Bone Metaphysis location? Benign (may convert to Level of malignancy? malignant) MRI shows medullary Radiologic importance? connection Ewing sarcoma ? 10-20 Age? LongBody bones, location? ribs, pelvis Metaphysis Bone location? or diaphysis Level Highly of malignancy? aggressive Notable CD99 finding? stain Chordoma ? 27-80 Age? Sacrum, Body clivus, location? vertebrae Notochord Origin? Level Slow-growing of malignancy? Giant Cell Tumor ? 25-40 Age? Body Distal location? femur Bone Epiphysis location? Level ofBenign malignancy? Easily confused with Notable finding? tendon sheath tumor Tumor Age Bones affected Location on bone Malignancy Special points Osteosarcoma 10-20 Knee Metaphysis High Sunburst, Codman Triangle, osteoid Osteochondroma 10-30 Tibia, fibula, humerus Metaphysis Ben. Medullary connection Ewing Sarcoma 10-20 Long bones, ribs, pelvis Dia./meta. High CD99 stain Giant Cell Tumor 25-40 Femur Epiphysis Ben. Chondroma 30-50 Hands, feet, arms, legs Cortex, surface Ben. Osteoma 60 Skull Chondrosarcoma 50-70 Pelvis, ribs, femur Cortex Low Dedifferentiation Osteoid Osteoma Long bone Cortex Ben. <2cm Osteoblastoma Spine Ben. >2cm Chordoma Sacrum, vertebrae Low Ben. Joint Hypermobility Age,Joint gender, hypermobility family depends background, on which ethnic fourbackground factors? Why are AfricanA failed war on Americans much By the drugs unfairly How is joint likely to be extensibility of the more our mobility limited, segregates jailed for joint joint capsule, society generally hypermobility? ligaments, and speaking? tendons Name three Skin striae, lax extraarticular upper eyelids, features involved weakness of pelvic in hypermobility floorIs it determined by syndrome.genetics Bothor the environment? Is the genetic trait Polygenic, of mono- or course polygenic? Ehlers Danlos Syndrome Does musculoskeletal pain present Early early or late in the syndrome? What is the main Theskeletal X-rays are abnormality normal on XWhich joints are ray? Shoulder, patella, particularly TMJ susceptible? What’s the most Hypermobility Is this chronic or A heterogenous prevalent form of Chronic, of Bruising, course scarring,type acute?What other group of heritable four EDS? What is EDS? tissue fragility, connective tissue presentations can What generally How can EDS skin Joint sublaxations occur? Pes planus (flat disorders happens withhyperextensibility this present in the & dislocations foot) type of EDS? lower extremities? Vascular EDS What’s the most common cause of Arterial rupture sudden death for vascular EDS? Where can The adipose face and limbs, deposition particularly be limited? What’s the genetic Autosomal inheritance in this dominant disorder? Arterial, What internal intestinal, damage and uterine can fragility/rupture occur? What facial characteristics Large eyes, thin can nose, be seen lobeless in this ears type of EDS? Marfan Syndrome What is the Fibrillin-1 mutation? Dilation of the aorta, involving …due to? the sinuses of Valsalva What cardiac Aortic symptom can be regurgitation associated? What’s the genetic What is the most Autosomal inheritance in this severe associated dominant Aortic dissection disorder? cardiovascular complication? Which is longer for Marfan patients – Arm span arm span or body height? What is another Ectopia associated lentis It’s a major symptom? What does fibrillin protein building do? block Arthritis Osteoarthritis Is local inflammation It can be present? Is joint effusion It can be present? More common in Women men or women? Are systemic What’s the most No Osteoarthritis! form of Radiographic effects present? prevalent arthritis? Why findings shouldn’t are far the hands more common be X-rayed in the for screening? hands than symptoms Osteoarthritis It gets worse When is pain the throughout the worst? What is the day Very pattern irregular of What happens to cartilage loss? metabolic It’s increased activity in the joint? Is chondrocyte Can joint proliferation instability Sure be What happens to It’s increased increased or present? What is the level the It’sjoint decreased space in of stiffness Low in the What can happen decreased? an X-ray? Subchondral cysts morning? below the and/or sclerosis cartilage? What happens to It’s proteoglycan decreased concentration? Osteoarthritis Deep groin pain Radiographic How can hip OA Typically, should What’s the radiating into evidence appears present? the pain be problem with this? medial thigh Yes late in the disease recreated with How MTPdoes joints diabetic with What is the gold passive motion? neuropathy excessive standard Radiograph for usually destruction present seen on diagnosis? inX-ray? X-ray Is OA associated Previous trauma, with Short-term short- or NM What disease are three (e.g. long-term stiffness (<1 stiffness hr) secondary diabetes), causes How good are ESR Which five joints (>What Pain or < 1are relief, hour)? the metabolic of OA? MCP, wrist, elbow, and Not CRP useful as disorders are typically not exercise three main regiment, points ankle, or shoulder markers for OA? involved? patient of treatment? education Osteoarthritis Risk Factors • • • • • • • H ereditary A ge Metabolic disorders S ex (female) N euromuscular disease O besity T rauma Osteoarthritis – Joints Involved Neck Hip Spine PIP, DIP, CMC Knee 1st MTP Spondyloarthropathies Which parts of the Can it be Vertebrae & Yup 1.is Ankylosing spondylitis body are generally What are the 5 peripheral too? If it’s peripheral, Usually 2. Reactive arthritis sacroiliac joints affected? it symmetric or3. IBD-associated arthritis spondyloasymmetric 4. Psoriatic arthritis What age group is asymmetric? 5. arthropathies? Undifferentiated No, Is nor HLA-B27 does it Genetically, what generally Younger rulescreening in or rule out HLA-B27 Is it genetic or is the main cause? affected? recommended? a disease environmentally Both ANA+ Negative or ANA-? determined? Are these Inflammatory or conditions more WhatInflammatory doesnonMales What is common the main in males Probably a inflammatory? spondylosis The vertebrae refer What does RF+ Negative or RF-? environmental Fusion/crooked or females? bacterial infection to? ankylosis mean? cause? Ankylosing Spondylitis Are big joints or “Ankylosing spondylitis” small joints isDid Catherine Crawford’s you know…? affected Big joints more Age? <40 favorite medical term? When is the pain often At night Which Vertebrae joints&are the worst? peripherally? Movement, affected? sacroiliac NSAIDs, What’s Anti-TNF, the What test is used osteoporosis treatment? toSchober’s monitor spinal test prophylaxis mobility? Is the pain better Acute or More men or Progressive or worse Worsewith Men progressive onset? women? rest? Extraarticular AS • • • • • • • • A ortic insufficiency N eurological symptoms K idneys: amyloidosis S pinal fracture, stenosis P ulmonary fibrosis O cular: anterior uveitis N ephropathy (IgA) D iscitis Reactive Arthritis Symmetrical or Asymmetric asymmetric? When are women Approximately likely to get WhatEnteric two types or ofmost overreactive per month 1-3When weeksdoes afterit an infection urogenital usually once arthritis? infection appear? (chlamydia) cause RA? NSAIDs – it’s Treatment? usually self-limited Conjunctivitis, arthritis, Triad? non-GC urethritis Mono-, oligo-, or Oligoarticular polyarticular? What type of bacteria is usually None; it’s sterile found in the synovial fluid? How can RA be differentiated AS is bilateral from SA in sacroiliac arthritis? Psoriatic Arthritis Inflammatory or Inflammatory noninflammatory? Erosive bone What can be seen disease in DIP radiographically? joints What is the severe Arthritis mutilans form of PA called? Chronic Chronic or acute? Which comes first – skin Skindisease diseaseor joint disease? What Theage under-50 group is affected? crew Anti-TNF Treatment? agents IBD-Associated Arthritis What Erythema about from nodosum Crohn’s? How do you treat Steroids those? Which causes deformity – the Axial form (fusion peripheral or axial & disability) form of the disease? can show on What’s Treat the the main What Pyoderma the skin from underlying treatment? disease gangrenosum ulcerative colitis? Should X-rays be No – they areBilateral sciatica, saddle Watchful How is mechanical waiting + used for anesthesia, Onlybowel/bladder 1 out of 2500 more often I incontinence don’t believe you Cauda EquinaLBP treated? mechanical back patients under When is acute LBPexercise misleading – give me a to muscles, syndrome, Does carryvariable a 60yo Injury What does painhas pattern, pain?itBruits, an a medical statistic abdominal mass abdominal aortic Good goodprognosis or poor “mechanical” ligaments, refer unexpected X-ray bones, emergency (3 aneurysm, prognosis? disks to? conditions)? neurologic deficit Yes! Those who Fifth-most Should remain activity activebe How common a common reason despite advised acute during pain complaint is it? for how an office visit How long until For long acute have pain less future phase? 90% resolve most cases have 2-3 should days rest at most be chronic pain within 8 weeks resolved? advised? Which type of exercises should How much acute What’s the main Mechanical be performed Both back – pain <5% turns type of LBP? strength or chronic? endurance? Lower Back Pain Low Back Pain – Red Flags What am I? Low back Lowpain back pain • Fever, weight loss • Intractable pain—no improvement in 4 to 6 weeks • Nocturnal pain or increasing pain severity • Morning back stiffness with pain onset before age 40 • Neurologic deficits What is the main What is the main Resuming activity presenting goal for acute Sudden back pain. What Pain at are night, the main local as soon as symptom of an compression Duh. symptoms tenderness, of a possible acute compression fractures? elevated spinalESR,Hormone Epidural LegWhat pain/tingling is thefracture? How is it weight lossreplacement What’s the severe corticosteroids, malignancy? with presentation less of or a managed? therapy, treatment thiazides, of pain exercise, surgery Non-improving herniated no back disk? osteoporosis? Ca/Vit D, Fever, rigors, focal What are the pain, increasing bisphosphonates Surgery tends to What tenderness are thewith main symptoms of Why not do lower neurological have no better muscle symptoms spasm; of spinal stenosis? surgery? symptoms pain reliefAnd don’t forget spinal needle infections? tracks Yeah! the exercise! present What labs should How is a herniated When is surgery What surgical Symptomatic What Neurologicbe deficits Mildcan anemia, be seen taken for the disk treated? indicated? option exists for Vertebroplasty in elevated the labsESR of initial Hb,evaluation ESR, Ca compression spinal and/or infections? CRP of osteoporosis fractures? (3)? Back pain Low Back Pain Tolerance, What are the four Ignorance, consequences of Activation-death, Ag encounter with Activationlymphocytes? proliferation What’s Defectsthe in Immunology apoptosis relationship may between lead to autoimmunity autoimmuneand The What periphery about B& apoptosis? conditions What type of bonecells? marrow They How encounter do B cells autoimmune Repetitive becomehigh anergic in condition ITPinvolvesWhat stimulation, is AICD? concentrations the peripheralof platelets as acausing apoptosis lymphoid antigens tissue? target? Where does “anergy” Tolerance fall into What two general What two types of those four? Co-stimulator are What type of Ag +signals cells are largely Where The periphery does T-cell & autoimmune (e.g. required B7/CD28) for Treg and Tsuppressor anemia responsible for tolerance the thymus occur? Hemolytic activation? condition involves cells peripheral T-cell RBC’s as a target? tolerance? Immunopathogenic Mechanisms Condition Immunological disease type SLE II, III, IV ITP II Hemolytic anemia II RA III & IV Type I Diabetes Mellitus IV Cryoglobulinemia III Goodpasture’s II Explain SLE’s type •Malar rash Anti-snRNP T cells IV •Discoid involvement rash SLE Which immune mechanisms (type II, III, & IV I-IV) are involved in SLE? •Photosensitivity •Oral ulcers Azathioprine, Four symptoms What are•Arthritis the main methotrexate, •Serositis from Howthe is SLE SLE drugs used in the cyclo•Renal disorder Classification diagnosed? What’s Overall the treatment? What test isdisorder phosphamide •Neurologic Criteria Nothing like that suppression general focus of the of pathognomonic •Hematologic disorder exists treatment disease for SLE? for SLE? •Immunologic disorder What are the main •ANA Explain SLE’s type Arthralgia two initial (53%), Explain SLE’s type IC nephritis Anti-RBC III involvement presentations Rash (19%) of II involvement SLE? Rheumatoid Arthritis They’re the minority of Inflammatory or What are type B Prevalence 0.5-1% of in the the synoviocytes & Inflammatory nonsynoviocytes? population US? can damage the inflammatory? joint 1:3 (more M:F? women) What are the main RA patients are at concerns for RA a higher risk to Increased risk of Lymphoma patients with contract which stroke & MI respect to sudden type of cancer? death? Mono-, oligo-, or Polyarticular polyarticular? Local orBoth systemic? Age 25-50 of onset? Rheumatoid Arthritis What are the Cervical Does RA cause Swan-neck, How can the spine three main hand subluxation (C1 on Which two general bone Erosion erosion or Boutonniere, MCP be affected? Where do deformities from C2) Joint radiographic narrowing, formation? subuxation rheumatoid HLA-DR4 (which RA? Olecranon process findings erosion are most Which HLA nodules usually stands for type HLA-is Serpositive RA prominent in RA? associated with appear? Develops with What’s splenomegaly Felty’s Is there a RA? Rheumatoid 4)* necrotic correlation Central & *Not syndrome? really What is in a zone with sharp between YupRA titer rheumatoid granulocytopenia border of and disease nodule? What are the What’s the most With which palisading cells Is exercise good severity?DMARDs, NSAIDS, Of course main pharm important aspect treatment isthree early for RA? stiffness Morning Stiffness – a little biologics (antiEarly intervention Any of them treatments of successful >or1ahour lot? intervention most TNF) for RA? treatment of RA? effective? RA – Extraarticular Manifestions • P ulmonary • H ematologic • Ocular • N eurologic • V asculitis Interstitial fibrosis, pulmonary nodules, pleuritis Anemia, thrombocytosis Scleritis, episcleritis Entrapment syndromes, peripheral nephropathy Subcu nodules, leukocytoclastic vasculitis Psoriatic Arthritis What’s the relationship Does PsA affect How 3-5% common of the is between No relationship PsA and men or M=F women population psoriasis? the severity of the more? What other psoriasis? component Tendonsof – the What is the worst Pencil-in-cup What does the joint What are the Arthritis mutilans > joint enthesitis can be How many ofcase of PsA?Using handsradiology show? three main erosions 5-39% have Standing > inflamed? those activities affected psoriatic arthritis? Sleeping What type of byoccurs PsA? first Which edematous NSAIDs, Symmetric or – arthritis Dactylitis What is the A- Usually structural Age 30-50 of onset? pattern occurs in asymmetric? corticosteroids, symptoms or treatment? damage the fingers? DMARDs, Biologics structural damage? Psoriatic Arthritis – 5 subgroups • • • • • Spondylitis Polyarticular, symmetric Oligoarticular, asymmetric Mutilans DIP synovitis Vasculitis Disease? Disease? Disease? Disease? Intima, internal elastic lamina, media, adventitia Aorta + major branches “Medium?” “Large?” Which half of the Blindness, body The is lower most What are the main headache, jaw extremities affected by complications of How is temporal pain, neurological vasculitis? temporal arteritis? Possibly because arteritis Biopsy disturbances Why do differenteach size has a diagnosed? sized vessels have Due to the skipdifferent antigen What is the What is a common different diseases? Mostly unknown lesion nature, concentration a causative agent? mistake made in single biopsy may temporal arteritis result in a false biopsy? The temporal is affected and negative What What age group is by ophthalmic giant cell Middle-age and usually affected by arteritis? arteries What size of elderly Systemic, with What lab test is temporal arteritis? Are vasculites vessels does localized useful ESR >in50 the Smaller systemic or rheumatoid symptoms (e.g. diagnosis? localized? arthritis affect? ischemia) Vasculitis Polyarthralgia Rheumatica Pain/stiffness in What are the main neck, shoulder, & clinical symptoms? pelvic girdles When is the After rest (it’s hard stiffness usually to get out of bed) the worst? Are the peripheral Usually symptoms bilateral and symmetric symmetric or asymmetric? What disease can Temporal arteritis be associated with (GCA) PR? Fibromyalgia What is the cause Unknown of fibromyalgia? What 30-50 age group? Is the onset slow It can be either or fast? Which lab test Are symptoms helpsNone diagnose constant Varyingor fibromyalgia? varying? FMWhat patients is the have anrelationship abnormalitytoin deep sleep? sleep What kind of pain Diffuse, amplified is felt? Which organbased disease IBD is it associated with? How 5% many of all people Chronic, does Americans it affect? widespread What are pain the + cardinal tender points features? on exam Joint surgeries Which result in What is the gold more Who should get a Cemented total Cemented Who is more likely Younger, more standard in hip radiolucencies –nerve is noncemented hip What hip–prosthesis How Debridement, do you treat to get Younger; osteolysis it’s active prostheses? cemented or non? replacement? The mostsciatic commonly nerve a drainage, superficial related youngertoor activity older What are the DM, affected? antibiotics infection? patients? three main risk Immunosuppressi What causes the factors for on, prior surgery Soft-tissue majoritylaxity of infection? What treatments Are they likely to Two-stage type of dislocations? Antigoagulation, Most do not recur Which are suggested recur? reconstruction antibiotics post-op? (92% works success) best? What’s the main Observation, What’s the main How do you treat bacteria Staph. aureus involved The What is the it’sradiolucency Are they usually problem Osteolysis with non-unless that? in infection? outcome of the cement, defined progressing anterior Posterior or cemented? post-op by? posterior? Bursitis & Tendonitis The abductor Which part of the What is affected hand is involved in pollicis longus and The palmar fascia Obstruction at A1 with de Quervain’s Dupuytren’s pulley What in is involved proximal extensor pollicis tenosynovitis? Contracture? brevis tendons in portion triggeroffinger? flexor Where tendon do sheath most ganglion Dorsal wrist cysts What test helps occur? Finkelstein’s test diagnose this? What can be a A compressive complication of a neuropathy Inflammation of Which age group ganglion cyst? Is proliferative Which sheathisisaffected with theWhat synovium is Many Older males Chronic tenosynovitis? surrounding a tenosynovitis affected? Dupuytren’s tendon chronic or acute? Contracture? What is the main Leg cause length of a trochanteric discrepancy bursitis? Which fingers are Bursitis & Tendonitis What is affected with The median carpal tunnel nerve Manual pressure McMurthry’s sign? syndrome? innervated The first by 3 ½the of median nerve Which three Are the symptoms median nerve? They’re worse at rheumatoid or better Scleroderma, RA, worsenight conditions can during the day? and gout lead to olecranon What are the main Which muscleWhat is does Cubital bursitis? The extensor carpi tunnel Ulnarsyndrome nerve Swelling clinicaland affected by lateral radialis brevis affect? presentations numbness of What test epicondylitis? involves How can you carpal tunnel? percussion at the Flexion of the What about Point tenderness What’s Phalen’s Pronator teres or differentiate it Tinel’s wrist that signtrochanterichands at the wrist medial in the test? flexor carpi radialis recreates the from for one minute epicondylitis? bursa osteoarthritis? paresthesia?