System, policy and environmental change
advertisement

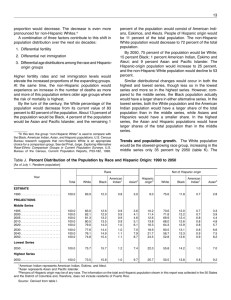
System, policy and environmental change: Evidence, Gaps and Implications Presented by: Laura K. Brennan, PhD, MPH Overview Projects Brief Description 1. Social determinants of health (2003-2010) Funding: Centers for Disease Control & Prevention Process: Forum, Presentation, Application Products: Workbook, Training, Train-the-trainer 2. Evaluation of Active Living by Design (2006-2010) Funding: Robert Wood Johnson Foundation Process: Interviews/Site visits Products: Journal Supplement, Case Reports 3. Review of environment & policy interventions for childhood obesity prevention (2008-2011) Funding: Robert Wood Johnson Foundation Process: Advisors, Resource review Products: Intervention strategy summaries, Gaps 4. Evaluation of Healthy Kids, Healthy Communities (2009-2014) Funding: Robert Wood Johnson Foundation Process: Technical assistance, Interviews/Site visits Products: Articles, Policy Briefs, Resources, Tools 5. System dynamics modeling to inform overweight and obesityrelevant policy (2009-2011) Funding: National Institutes of Health Process: Group model building Products: System dynamics models Our Team Julie Claus, Chief Operating Officer Sarah Castro, Project Director Peter Holtgrave, Project Director Tammy Behlmann, Project Manager Laura Runnels, Project Manager Courtney Jones, Project Coordinator Allison Kemner, Project Coordinator Daedra Lohr, Financial Coordinator Many part-time staff and interns Our Local Collaborators Elizabeth Baker, Saint Louis University Cheryl Kelly, Saint Louis University Ross Brownson, Washington University Cheryl Carnoske, Washington University Debra Haire-Joshu, Washington University Christine Hoehner, Washington University Peter Hovmand, Washington University Timothy Hower, Washington University Our National Advisors Policy/Practice Partners RWJF, NIH & CDC Rachel Ballard-Barbash Jamie Bussell William Dietz Terry Huang Laura Kettel-Khan Laura Leviton Elizabeth Majestic Robin McKinnon Shawna Mercer Marilyn Metzler Meredith Reynolds Tracy Orleans Thomas Schmid Celeste Torio Pattie Tucker Researcher Partners Karen Glanz Frank Chaloupka Lawrence Green Shiriki Kumanyika Marc Manley Barbara Riley James Sallis Eduardo Sanchez Loel Solomon Janice Sommers Mary Story Antronette Yancey Don Bishop Elaine Borton Leah Ersoylu Steve Farrar Harold Goldstein Dean Grandin James Krieger Jacqueline Martinez Malisa McCreedy Leslie Mikkelsen Joyal Mulheron Maya Rockeymoore Marion Standish Sarah Strunk Ian Thomas Mildred Thompson Social Determinants of Health: Learning from Doing Ottawa Charter International Conference on Health Promotion in 1986 Health promotion approach: – – – – – Building healthy public policy Creating supportive environments Strengthening community actions Developing personal skills Reorienting health services Ottawa Charter “Health promotion is the process of enabling people to increase control over, and to improve, their health. To reach a state of complete physical, mental and social well-being, an individual or group must be able to identify and to realize aspirations, to satisfy needs, and to change or cope with the environment... People cannot achieve their fullest health potential unless they are able to take control of those things which determine their health. At the heart of this process is [communities taking] ownership and control of their own endeavors and destinies.” Ottawa Charter for Health Promotion (1986) Common Language Community Health disparities Health inequities Health equity Social determinants of health (SDOH) Community A group of people with a shared identity, including: living in a particular geographic area; having some level of social interaction; sharing a sense of belonging; or having common political or social responsibilities References: Eng, Parker (1994), Fellin (1995), Hunter (1975), Israel, et al (1994), MacQueen, et al (2001), McKnight (1992) Distribution of U.S. Population by Race/Ethnicity, 2007 Native Hawaiians/Pacific Islanders 0% Asian 4% American Indian/ Alaska Native 1% (2.3 million) (0.4 million) Two or more races 1% (13.1 million) (4.2 million) African American 12% (37.0 million) Hispanic 15% (45.5 million) White 66% (199.1 million) Total = 301.6 million NOTES: Data do not include residents of Puerto Rico, American Samoa, Guam, the U.S. Virgin Islands, or the Northern Mariana Islands. Totals may not add to 100% due to rounding. All racial groups and individuals reporting “two or more races” non-Hispanic. SOURCE: Kaiser Family Foundation, based on Table 3: Annual Estimates of the Population by Sex, Race and Hispanic Origin for the United States: April 1, 2000 to July 1, 2007 (NC-EST2007-03). Population Division, U.S. Census Bureau. Share of Population that is a Racial/Ethnic Minority by State, 2005-2006 Less than 14% (11 states) 14% to 21% (13 states) 22% to 36% (14 states) More than 37% (13 states) SOURCE: Urban Institute and Kaiser Commission on Medicaid and the Uninsured analysis of March 2006 and March 2005 Current Population Survey. Distribution of U.S. Population by Race/Ethnicity, 2000 and 2050 50.1% White, Non-Hispanic 69.4% Hispanic African American 24.4% 12.6% 3.8% 2.5% 12.7% 2000 Total = 282.1 million Asian Other 14.6% 8.0% 5.3% 2050 Total = 419.9 million NOTES: Data do not include residents of Puerto Rico, Guam, the U.S. Virgin Islands, or the Northern Marina Islands. “Other” category includes American Indian/Alaska Native, Native Hawaiian or Other Pacific Islander, and individuals reporting “Two or more races.” African-American, Asian, and Other categories jointly double-count 1% (2000) and 2% (2050) of the population that is of these races and Hispanic; thus, totals may not add to 100%. SOURCE: Kaiser Family Foundation, based on http://www.census.gov/population/www/projections/popproj.html, U.S. Census Bureau, 2004, US Interim Projections by Age, Sex, Race, and Hispanic Origin. Health Disparities Differences in the incidence and prevalence of health conditions and health status between groups, based on: Race/ethnicity Socioeconomic status Sexual orientation Gender Disability status Geographic location Combination of these Reference: Braveman P. (2006)1 Cancer Screening Rates by Race/Ethnicity*, 2003 70.4% 65.1% 70.0% 58.2% Breast Cancer (Mammography) White, NonHispanic Hispanic 80.2% 74.6% 82.6% 67.8% Cervical Cancer (Pap Test) Colon and Rectum Cancer (Fecal Occult Blood Test) 22.7% 15.4% 22.3% 18.3% AfricanAmerican, NonHispanic Asian NOTES: * Data for American Indians/Alaska Natives and Native Hawaiians/Pacific Islanders do not meet the criteria for statistical reliability, data quality or confidentiality. Age-adjusted percentages of women 40 and older who reported a mammography within the past 2 years, women 18 and older who reported a pap test within the past 3 years, and adults 50 and older (male and female) who reported a fecal occult blood test within the past 2 years. SOURCE: Kaiser Family Foundation, based on the National Healthcare Disparities Report, 2005, available at: http://www.ahrq.gov/qual/nhdr05/index.html, using data from the Centers for Disease Control and Prevention, National Center for Health Statistics, National Health Interview Survey. Health Inequities Systematic and unjust distribution of social, economic, and environmental conditions needed for health Access to healthcare Employment Education Access to resources (e.g., grocery stores, car seats) Income Housing Transportation Positive social status Freedom from discrimination Reference: Whitehead M. et al7 Health Insurance Status, by Race/Ethnicity: Children, 2007 Private (Employer and Individual) 8% 21% 13% 20% 12% 19%* 19% 43% 8% 34% NSD 68% 36% Uninsured 45% 73% Total Child Population 2007 Medicaid and Other Public 43% 58% 31%* White Hispanic African American Asian/ Pacific Islander American Indian/ Alaska Native Two or More Races 44.7 million 16.5 million 11.6 million 3.3 million 0.5 million 2.1 million NOTES: “NSD” = Not sufficient data; “Other Public” includes Medicare and military-related coverage. All racial groups non-Hispanic. * = Estimate has a large 95% confidence interval of +/- 5.0 - 7.9 percentage points. SOURCE: Urban Institute and Kaiser Commission on Medicaid and the Uninsured analysis of the March 2008 Current Population Survey. Percent Uninsured, Ages 55-64, by Race/Ethnicity, 2006 33% 23.0% 18.7% 16.5% 12.7% 9.5% White, Non-Hispanic Hispanic African American, Asian/ American Indian/ Non-Hispanic Pacific Islander Alaska Native DATA: March 2007 Current Population Survey SOURCE: Kaiser Commission on Medicaid and the Uninsured estimates. Two or More Races No Doctor Visit in Past Year for Nonelderly Adults by Race/Ethnicity and Insurance Status, 2005-2006 Insured Uninsured 53% 48% 40% 39% 45% 31% 21% 14% White, NonHispanic 20% 13% Hispanic African American 14% 13% American Indian/Alaska Native Asian and NHPI SOURCE: Kaiser Family Foundation and Urban Institute analysis of the National Health Interview Survey, 2005 and 2006, two-year pooled data. Two or More Races No Usual Source of Care for Nonelderly Adults by Race/Ethnicity and Insurance Status, 2005-2006 Insured Uninsured 62% 45% 48% 45% 41% 35% 9% White, NonHispanic 13% Hispanic 8% African American 7% 11% American Asian and NHPI Indian/Alaska Native SOURCE: Kaiser Family Foundation and Urban Institute analysis of National Health Interview Survey, 2005 and 2006, twoyear pooled data. 11% Two or More Races Life Expectancy at Age 25 for U.S. Black and White Men with Similar Income Levels* 60 50 52.9 50.2 50.2 47.4 45.0 41.6 40 White Men 30 Black Men 20 10 0 $25,000 or more $10,000-$24,999 $10,000 or less * 1980s income levels SOURCE: NLMS: Lin et al 2003 and Nancy E. Adler, Health Disparities: Measurement, Mechanisms, and Meaning presentation, NIH Infant Mortality Rates for Mothers Age 20+, by Race/Ethnicity and Education, 2001-2003 Infant deaths per 1,000 live births: Less than High School 15.1 10.7 9.2 5.0 5.2 African American, Non-Hispanic American Indian/Alaska Native 13.4 High School 9.2 White, Non-Hispanic 6.5 5.6 5.3 11.5 College + 7.0 4.2 3.9 4.6 Asian/Pacific Islander Hispanic SOURCE: Kaiser Family Foundation, based on Health, United States, 2006, Table 20, using data from the National Center for Health Statistics, National Vital Statistics System, National Linked Birth/Infant Death Data. Health Equity The opportunity for everyone to attain his or her full health potential No one is disadvantaged from achieving this potential because of his or her social position or other socially determined circumstance Distinct from health equality Reference: Whitehead M. et al7 Social Determinants Life-enhancing resources, such as food supply, housing, economic and social relationships, transportation, education and health care, whose distribution across populations effectively determines length and quality of life. Reference: James S. (2002)6 Diseases and Behaviors Tobacco Use Poor Nutrition Physical Activity Physician Visits Arthritis/Lupus ✓ ✓ ✓ Asthma ✓ ✓ ✓ Breast Cancer ✓ ✓ ✓ Colorectal Cancer ✓ ✓ ✓ COPD (Lung Disease) ✓ Diabetes ✓ ✓ ✓ ✓ Heart Disease and Stroke ✓ ✓ ✓ ✓ ✓ Hepatitis B ✓ Immunizations (for adults) ✓ Infant Health Problems ✓ Injury from falls ✓ ✓ ✓ ✓ ✓ Lung Cancer ✓ ✓ ✓ Oral Health ✓ ✓ ✓ Pneumonia and Influenza ✓ ✓ SDOH and Health Pathways from social determinants to health Active Living by Design National program, The Robert Wood Johnson Foundation Purpose: To establish innovative approaches to increase physical activity through community design, public policy, and communications strategies ALbD Community Action (or “5P”) Model: – Preparation – Promotion – Programs – Policy Influence – Physical Projects www.activelivingbydesign.org ALbD Products ALbD Best Practices special issue (available: http://www.activelivingbydesign.org/AJPM) ALbD Evaluation special issue (under development) – Active Living Research evaluation (2 communities) – Progress reporting – Concept mapping – “5P” strategies and integration of approaches Other reports/products: – Cross-site report – Community partnership summaries Healthy Kids, Healthy Communities National program, The Robert Wood Johnson Foundation Purpose: To implement healthy eating and active living policy- and environmental-change initiatives that can support healthier communities for children and families across the United States HKHC places special emphasis on reaching children who are at highest risk for obesity on the basis of race/ethnicity, income and/or geographic location www.healthykidshealthycommunities.org Healthy Kids, Healthy Communities (50 Grantees) HKHC Leading Site Communities Seattle/King County, WA Portland/Multnomah County, OR Houghton, MI Benton County, OR Rochester, NY Milwaukee, WI Buffalo, NY Somerville, MA Kingston, NY Flint, MI Kane County, IL Omaha, NE Oakland, CA Watsonville/Parajo Valley, CA Denver, CO Hamilton County, OH Washington, DC Charleston, WV Columbia, MO Baldwin Park, CA Rancho Cucamonga, CA Cuba, NM San Felipe Pueblo, NM Boone/Newton Counties, AR Louisville, KY Knoxville, TN Chattanooga, TN Desoto/Marshall/ Tate Counties, MS Phoenix, AZ Nash/Edgecombe Counties, NC Moore/Montgomery Counties, NC Greenville, SC Jefferson County, AL Spartanburg, SC Milledgeville, GA Grant County, NM Jackson, MS El Paso, TX San Antonio, TX Philadelphia,PA Chicago, IL Kansas City, MO Central Valley, CA Fitchburg, MA Houston, TX New Orleans, LA Cook County, GA Duval County, FL Lake Worth/Greenacres/ Palm Springs, FL Caguas, PR Healthy Kids, Healthy Communities Assessment & Evaluation Assessment Planning & Implementation Evaluation • Identify assets, needs & previous or complementary work (inform planning and implementation) • Identify goals/objectives & prioritize efforts (use assessment findings) • Measure new or modified systems, policies & environments (what changed) • Measure current systems, policies & environments (baseline evaluation) • Track activities, impacts, outcomes, strengths & challenges (determine evaluation priorities) • Contextualize the changes through analysis of processes, strengths & challenges (what worked) Why Evaluate? To determine the effectiveness of local policy, environment, and systems approaches to prevent or reduce childhood obesity Short-, intermediate- & long-term impacts and outcomes related to health behaviors and obesity Reliable & valid quantitative tools & measures Study design and execution to ensure confidence in the findings from the evaluation To identify the approaches with the greatest impact, relevance, feasibility and sustainability What works, where it works, when it works, how it works & why it works (or why not) Multi-method quantitative & qualitative measures Local representation and participation to ensure confidence in the findings from the evaluation To inform local decision-making, document successes & obtain more funding Track intended/unintended results, practical considerations (resources, costs), assets & challenges Simple, quick measures serving multiple purposes (advocacy, marketing, cost/benefit) Findings translate to the interests of local audiences (decision-makers, business owners) THESE ARE NOT MUTUALLY EXCLUSIVE… Evidence Goals 1) To bridge research/evaluation and policy/practice efforts associated with environment and policy nutrition and physical activity intervention strategies for childhood obesity prevention. 2) To accelerate the translation of replicable, evidencebased environment and policy interventions that will lead to leveling and eventually reducing rates of childhood obesity, especially in lower income and racial/ethnic populations. Evidence Levels How do we define levels of evidence in order to bridge the gap between research/evaluation and policy/practice efforts? Evidence Review How do we create a complementary process to identify, collect and review a range of different evidence resources from research/evaluation and policy/practice efforts? Review Cycle INPUT Identification and collection of resources (inclusion/exclusion criteria) Remove Building the Evidence for Environment & Policy Change OUTPUT Implementation guides EFFECTIVE (1st TIER) STRATEGIES OUTPUT Systematic review Evidence gaps EFFECTIVE (2nd TIER) STRATEGIES PROMISING STRATEGIES OUTPUT Evaluation, feasibility & impact studies OUTPUT Pilot studies EMERGING STRATEGIES Inventory & Abstraction Articles Inventoried – Approx. 850 to be considered for effective (1st & 2nd tier) – Approx. 350 to be considered for promising and emerging – 227 federal bills Articles Abstracted – 44 from effective (1st tier) reviews – Approx. 390 effective (2nd tier) or promising • 128 Nutrition • 259 Physical Activity Intervention Strategy Summary Summary & synthesis of findings for each intervention strategy Includes: – Strategy overview (e.g., description, evidence rating) – Evidence summary (e.g., key ingredients, research/evaluation gaps, policy/practice implications) – Evidence tables for each study EFFECTIVE Applying the Evidence Typology Design/ Execution/Effectiveness Reach/Adoption/Implementation/Maintenance Experimental, quasi- Potential to directly or indirectly reach experimental, prospective crosssectional or natural experimental study design children and families; racial/ethnic and lower income populations High quality study execution (sampling/recruitment, statistical power, measures of exposure, internal validity) Effectiveness of intervention at changing obesity, physical activity or nutrition outcomes; demonstrating policy, environmental or economic impact Description of resources needed; anticipated support and opposition influencing adoption Use of theory or logic model; implementation fidelity or quality assurance assessment; sufficient description of intervention for replication Description of practicability for ongoing funding and support; plans for enforcement and maintenance PROMISING Applying the Evidence Typology Design/ Execution/Effectiveness Reach/Adoption/Implementation/Maintenance Quantitative or qualitative study Potential to directly or indirectly reach design children and families; racial/ethnic and lower income populations High quality study execution (sampling/recruitment, statistical power, measures of exposure, internal validity) Plausible effectiveness of intervention at changing obesity, physical activity or nutrition outcomes; demonstrating policy, environmental or economic impact Description of resources needed; anticipated support and opposition influencing adoption Use of theory or logic model; implementation fidelity or quality assurance assessment; sufficient description of intervention for replication Description of practicability for ongoing funding and support; plans for enforcement and maintenance EMERGING Applying the Evidence Typology Design/ Execution/Effectiveness Reach/Adoption/Implementation/Maintenance Potential to directly or indirectly reach Plausible effectiveness of intervention at changing obesity, physical activity or nutrition outcomes; demonstrating policy, environmental or economic impact children and families; racial/ethnic and lower income populations Description of resources needed; anticipated support and opposition influencing adoption Use of theory or logic model; implementation fidelity or quality assurance assessment; sufficient description of intervention for replication Description of practicability for ongoing funding and support; plans for enforcement and maintenance Intervention Strategy Summaries Healthy Eating School food & beverage policies School wellness policies National school lunch & breakfast program Provision of free or subscription F&V at school Provision of free drinking water at school Menu Labeling Childcare food & beverage policies Food pricing (schools & community) Neighborhood availability of restaurants Neighborhood availability of food stores Neighborhood availability of food stores & restaurants School & Community Gardens Government Nutrition Assistance Programs TOTAL number of Interventions to-date= 128 Active Living School physical activity policies School physical activity environments Childcare physical activity policies Safe Routes to School Neighborhood availability of parks, playgrounds, trails and recreation centers Neighborhood safety Point of decision prompts for physical activity Community design Street design Transportation policies Screen time TOTAL number of interventions to-date= 259 Inputs Inputs & Outputs Systematic Reviews Outputs Research & Evaluation Findings PeerReviewed Studies Evaluation Reports Community Demonstration Projects Strategic Partners & Systematic Methods RESOURCE INVENTORY ABSTRACTION Transtria LLC/Washington University Institute for Public Health Pilot or Case Studies Strategic Partners & Systematic Methods Gaps in Existing Evidence Policy & Environment Changes Other Key Ingredients Local Context Policy Briefs Standards of Practice Tools, Guides & Models Build connections to related efforts Task Force on Community Preventive Services CDC/RWJF Measurement (COCOMO) CDC/RWJF Early Assessment Initiative Centers for Disease Control and Prevention Center of Excellence for Training and Research Translation University of North Carolina, Chapel Hill Food and Nutrition Board Institute of Medicine Active Living Research National Institutes of Health Healthy Eating Research Healthy Kids, Healthy Communities Review of Environment & Policy Interventions Leadership for Healthy Communities Center for Childhood Obesity Prevention Communities Creating Healthy Environments Salud America! Physical Activity Policy Research Network State Health Depts Bridging the Gap The Robert Wood Johnson Foundation Discussion Activity County Health Rankings (115 Missouri Counties Ranked) Health Outcomes (Morbidity & Mortality) County Outcomes Morbidity Mortality St. Louis City 106 106 107 St. Louis County 18 32 11 St. Charles County 2 6 1 Robert Wood Johnson Foundation & University of Wisconsin Population Health Institute Discussion Activity County Health Rankings (115 Missouri Counties Ranked) Health Factors (Behaviors, Clinical Care, Social and Economic, and Environmental) County Factors Behavior Clinical Social & Economic Environment 115 113 4 115 115 St. Louis County 6 3 2 15 114 St. Charles County 1 1 5 2 111 St. Louis City Robert Wood Johnson Foundation & University of Wisconsin Population Health Institute Community Who does your community include? Who does it not include? Does your community have definite geographic boundaries? Are there social or cultural ties that link your community members to one another? Does your community have multiple communities within it? How would you describe these communities? What are other characteristics of your community? Health Equity o What are the health concerns of individuals in your community (e.g., asthma, diabetes)? o What are the conditions that affect your whole community (e.g., air pollution, high concentration of fast food restaurants)? o Are the health concerns and conditions affecting health differently for various groups in your community? Social Determinants of Health How are resources (e.g., food, housing, local businesses, transportation, health care services) distributed within your community? How do resources in your community compare to those in surrounding communities? How can social determinants impact health behaviors? Laura K. Brennan, PhD, MPH President and CEO laura@transtria.com