Working with Urinary and Fecal Incontinence and Pelvic Organ
advertisement

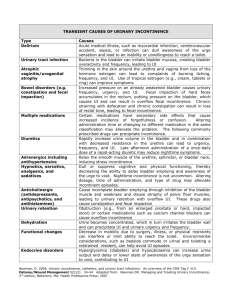
Presented by: Barbara Wiggin, PhD, ANP-BC CCA, specializing in UI, FI, FSH, UDS, POP www.cca-center.com Fall 2015 The bladder is composed of bands of interlaced smooth muscle (detrusor). The innervation of the body of the bladder is different from that of the bladder neck. The body is rich in beta adrenergic receptors. These receptors are stimulated by the sympathetic component of the autonomic nervous system (ANS). Beta stimulation, via fibers of the hypogastric nerve, suppress contraction of the detrusor. Conversely, parasympathetic stimulation, by fibers in the pelvic nerve, cause the detrusor to contract. Sympathetic stimulation is predominant during bladder filling, and theparasympathetic causes emptying. Two sphincters control the bladder outlet. The internal sphincter is composed of smooth muscle like the detrusor and extends into the bladder neck. Like the detrusor, the internal sphincter is controlled by the ANS and is normally closed. The primary receptors in the bladder neck are alphaadrenergic. Sympathetic stimulation of these alpha receptors, via fibers in the hypogastric nerve, contributes to urinary continence. The external sphincter is histologically different from the detrusor and internal sphincter. It is striated muscle. Like skeletal muscle, it's under voluntary control. It receives its innervation from the pudendal nerve, arising from the ventral horns of the sacral cord. During micturition, supraspinal centers block stimulation by the hypogastric and pudendal nerves. This relaxes the internal and external sphincters and removes the sympathetic inhibition of theparasympathetic receptors. The result is unobstructed passage of urine when the detrusor contracts. The ureters pass between the layers of the detrusor and enter the bladder through the trigone. The ureters propel urine into the bladder. The bladder passively expands to accept urine. As the bladder expands and intravesicular pressure increases, the ureters are compressed between the layers of muscle, creating a valve mechanism. This valve mechanism limits the backflow of urine. The normal adult bladder can hold about 500 cc of urine. After emptying, the bladder may still retain about 50 cc residual volume. At about 150 cc of volume, stretch receptors in the detrusor begin signaling the CNS via afferent nerves; at 400 cc we are "seeking" an appropriate toilet Summary: Normally, we are able to control where and when we void. This is largely because the cerebrum is able to suppress the sacral micturition reflex. If the sacral reflex is unrestrained, parasympathetic stimulation via the pelvic nerve causes detrusor contraction. Detrusor contraction is suppressed by alpha and beta sympathetic stimulation via the hypogastric nerve. In response to afferent stimulation, the cerebrum becomes aware of the need to void. If it is appropriate, the cerebrum relaxes the external sphincter, blocks sympathetic inhibition, the bladder contracts and urine is expelled Urinary System: Normal Anatomy & Physiology. http://www.rnceus.com/uro/norm2.htm Health history Continence history Uroflow Bladder Diary Medication evaluation Bowel status Urine Analysis Environmental & mobility assessment Urodynamic study Neurological disease Back Problems Obstetrical Gynecological Diabetes Acute Chronic D delirium I infection (UTI) A atrophic urethritis, vag. P pharmaceuticals P psychological (depression) E excess output: CHF, hyperglycemia R restricted mobility S stool impaction SUI & ISD Overactive bladder: with and without incontinence, IC Mixed Overflow & Retention Functional Reflex Oxybutynin: IR, ER, patch Tolterodine: IR, ER: less constipation than oxybutynin, dry mouth Trospium: lower constipation Solifenacin: lowest constipation (more selective for M3 receptors) Darifenacin: less mental confusion, fewer cardiac side effects (more selective for M3 receptors) Mirabegron(b3 adrenergic agonist) SE:palpitation, urinary retention, dry mouth, HTN, cold symptoms Glaucoma (usually just narrow angle) Hx of Constipation GI hypo motility Hx of Urinary retention Diminished mentation Hx of tachycardia onabotulinum toxinA : blocks action of acetylcholine and paralyses bladder muscle, lasts for several months Urgent PC: percutaneous tibial nerve stimulation (PTNS), mild impulses from the stimulator travel through the needle electrode, along your leg and to the nerves in your pelvis that control bladder function Electrical Stimulation Extracorporeal Magnetic Innervation (Neotonus Chair) InterStimMedtronic Bladder Control Therapy (Sacral Neuromodulation, delivered by the InterStim® System) has been FDA-approved since 1997 for urge incontinence and since 1999 for urinary retention and significant symptoms of urgency-frequency. Medtronic Bladder Control Therapy is not intended for patients with a urinary blockage. Behavioral Pelvic Muscle Rehab (written, verbal, biofeedback) Supportive pessaries Intraurethral Device FemSoft Electrical Stimulation Neotonus Chair Surgery Estrogen Fluid Management Prevention of Constipation Elevation of LE DC fluids 2-3 hours before HS Take a deep breath and lean forward when voiding Timed toileting Suppression techniques: “Quick Flicks” Monitor bladder irritants Use of Absorbent pads for Urinary Incontinence 10 second sustained contraction of pelvic floor muscle followed by 10 second relaxation of the pfm done 10 times twice a day. Use of biofeedback effective if unable to do pfme PFMT with Biofeedback is most effective non surgical modality for treatment of SUI Sling (use of cadaveric tissues, synthetic mesh, animal or donor tissue) Colpopexy mesh Urethral Bulking (Collagen) Injection of bulking materials around the urethra to increase outlet resistance InterStim Therapy Stimulation of sacral nerve for treatment of overactive bladder or retention. Neurostimulator supplying constant mild electrical pulses Electrode system placed at L/R 3rd sacral foramen Sacral nerves most common distal autonomic and somatic nerve supply to the pelvic floor and lower urinary and gastrointestinal tract Evaluate Bowel Status Formed or not Timing Physical exam of rectum Current problem Treatment Biofeedback Fiber Scheduled evacuation Fluid Exercise Indications: prolapse, desire not to have surgery, diagnostic tool for surgical relief, prediction of surgical outcome, Correcting stress incontinence, uterine retrodisplacement, preterm cervical dilation Pessary Wear and Care Intercourse Removal/Cleaning When to get a new one Refitting Tips Menses Gelhorn: Use a short stem if long stem bothers the patient New Visit Health history/sexual activity Focused physical Pessary fitting Teach patient how to care for pessary Follow up in 2 weeks and then in 1-2 months If patient managing care of pessary q 6 months If patient not managing pessary F/U Check U/A, uroflow, PVR Go over patient is managing pessary Evaluate if pessary is supporting prolapse Stand to evaluate Evaluate skin integrity Manage problems Schedule at appropriate interval Contraindication Pelvic infections Lacerations or ulcers Non-compliance Wide introitus, short vaginal vault Properly Fitted Pessary Patient is unaware of the pessary No pain or discomfort Symptoms are relieved Move and toilet pt at least every 2-3 hours Clean soiled area with water and/or cleanser Use a skin barrier (A&D ointment) Notify appropriate staff if skin is breaking down Change pads when soiled Good hydration Good nutrition Adequate fluid intake (6-8 8 oz glasses of non-caffeinated fluids) Monitor urine color and odor Monitor pt for confusion, elevated temp, not feeling well Adequate hydration Dabbing when wiping Pt. checked to ensure he/she is emptying completely Void q 2-3 hours Take a deep breath/lean forward to empty Taking enough time to void Using water to cleanse vulva Unavoidable if has indwelling catheter, CIC decreases UTIs Consider UTI if pt has increased confusion, odorous urine, changed bladder pattern Sex: F Age: 92 c/o: frequency, nocturia, ui Health Hx: arthritis, glaucoma, hypertension (not a problem now), osteoporosis Current medications: None Previous treatment: anticholinergics Focused physical exam: pale vag. tissue, little recruitment of pfm, U/A neg UDS: normal capacity, poor compliance, SUI at low pressure (56 cm H20), empties well, increased pfm tone with voiding Plan of Care: fluid management, elevation of legs, stress technique, biofeedback assisted pfme Results of Treatment: often does not wear pads, continues to do pfme, discussed collagen implants. Sex: F Age: 77 c/o: overactive bladder Health Hx: depression/anxiety, arthritis, hysterectomy, HTN Current medications: lansoprazole, estrogen, valsartan, nabumetone, escitalopram, tolterodine Previous treatment: tolterodine Focused physical exam: pale vag. tissue, reddened vulva, sl recruitment of pfm, atrophic introitus, U/A neg UDS: delayed 1st sensation, normal capacity, SUI at low pressure (75 cm H20), empties well, emg activity during void, after contraction Plan of Care: Dc’d tolterodine, discussed collagen implant, or sling, stress technique, urge technique, biofeedback assisted pfme Results of Treatment: pt. feel she is much improved, continues to do pfme, does not want referral to urologist. Doughty, D. B. Urinary and fecal incontinence (3rd ed.) (pp. 21-54). St. Louis, MO: Mosby/Elsevier. Dr. Rose’s peripheral brain. (2012, October24). Neurogenic bladder:Bladder dysfunction and urinary incontinence. http://faculty.washington.edu/momus/PB/tableofc.htm Effective Health Care Program (2012,April) Non-surgical treatments for urinary incontinence, A review of the research for women. Agency for Healthcare, Research and Quality. Pub No. 11(12)EHCO74-A Gray, M.L. (2006). rdPhysiology of voiding. In Doughty, D. B. Urinary and fecal incontinence (3 ed.) (pp. 21-54). St. Louis, MO: Mosby/Elsevier. Kershen, R.T., Appell, R.A. (2003). Voiding dysfunction after anti-incontinence surgery in women. Issues in Incontinence, Spring/Summer, 1,9-11. Krissovich, M. (2006). Pathology and management rd of the overactive bladder. In Doughty, D. B. Urinary and fecal incontinence (3 ed.) (pp. 109-165). St. Louis, MO: Mosby/Elsevier. Mayo Clinic. (1998-2007). Overactive bladder. http://www.mayoclinic.com/print/overactivebladder/DS00827/DSECTION=all&METHO... Medtronic. What Is Medtronic Bladder Control Therapy? http://www.medtronic.com/patients/overactive-bladder/about-therapy/what-isit/index.htm National guidelines and clinical evidence only modestly influence prescribing of antihypertensive agents. (2007, January). Research Activities, 317, 15. Newman, D.K. (2007, March). Dawning of a dry day: Fresh perspectives in managing overactive bladder. Paper presented at the Annual Symposium of the Society of Urologic Nurses and Associates, Colorado Springs, CO. Newman, D.K. (2006, October). Pharmacologic Management of OAB-You make the call. Paper presented the Annual Meeting of the Society of Urologic Nurses and Associates, Kansas City, MO. Sand, P.K., Dmochowski, R. (2002). Analysis of the standards of terminology of lower urinary tract dysfunction: Report from the standardisation sub-committee of the International Continence Society. Neurology and Urodynamics, 21, 167-78. NIH. (2007). Urologic disease cost Americans $11 billion a year. http://www.nih.gov/news/pr/may2007/niddk-01.htm. Serels, S.R., Appell, R.A. (2002, 2001). Bladder control problems. Newton, PA: Handbooks in Health Care Co. Staskin, D. (2004). Lower urinary tract dysfunction in the female. In A.P. Bourcier, E.J. McGuire, & P. Abrams (Eds.), Pelvic floor disorders (pp. 43-56). Philadelphia, PA: Elsevier Saunders. Urinary Incontinence in Adults Guideline Update Panel. (1996). Urinary incontinence in adults: Acute and chronic management. Clinical Practice Guideline, No. 2, 1996 Update. Rockville, MD: U.S. Department of Health and Human Services. Public Health Service, Agency for Health Care Policy and Research (AHCPR Publication No.96-0682). Urinary System: Normal Anatomy & Physiology. http://www.rnceus.com/uro/norm2.htm Uroplasty. Urgent ® PC Neuromodulation System. https://www.uroplasty.com/healthcare