Pharmacology - Pemberton Counseling

Pharmacology
Overview
Major Types
Antidepressants
Mood Stabilizers
Anti Anxiety
ADHD
Anti psychotics
Antidepressants
Major Groups
Atypicals – unique properties
SSRI – most popular
SNRI – more effective/side effects
NRI - new
Cyclic – react with multiple sites
MAOI – high risk of hypertensive reaction
Antidepressants cont’
Page 176 – Choice of antidepressant
Special Considerations - 177
Side effects
Start low
Nausea – take with meal
Insomnia – take in morning
Anxiety – reduce caffeine
Sedation – take at night
Sexual – other medication
Dry mouth – gum, water
Am Psych Assoc
Mood Stabilizers
the initiation of either lithium plus an antipsychotic or valproate plus an antipsychotic
[I]. For less ill patients, monotherapy with lithium, valproate , or an antipsychotic such as olanzapine may be sufficient [I]. Short-term adjunctive treatment with a benzodiazepine may also be helpful [II]. For mixed episodes, valproate may be preferred over lithium [II]. Atypical antipsychotics are preferred over typical antipsychotics because of their more benign side effect profile [I], with most of the evidence supporting the use of olanzapine or risperidone [II]. Alternatives include carbamazepine or oxcarbazepine in lieu of lithium or valproate [II]. Antidepressants should be tapered and discontinued if possible [I]. If psychosocial therapy approaches are used, they should be combined with pharmacotherapy [I].
For patients who, despite receiving maintenance medication treatment, experience a manic or mixed episode (i.e., a “breakthrough” episode), the first-line intervention should be to optimize the medication dose [I]. Introduction or resumption of an antipsychotic is sometimes necessary [II]. Severely ill or agitated patients may also require short-term adjunctive treatment with a benzodiazepine [I].
When first-line medication treatment at optimal doses fails to control symptoms, recommended treatment options include addition of another first-line medication
[I]. Alternative treatment options include adding carbamazepine or oxcarbazepine in lieu of an additional first- line medication [II], adding an antipsychotic if not already prescribed [I], or changing from one antipsychotic to another [III]. Clozapine may be particularly effective in the treatment of refractory illness [II]. ECT may also be considered for patients with severe or treatment-resistant mania or if preferred by the patient in consultation with the psychiatrist [I]. In addition, ECT is a potential treatment for patients experiencing mixed episodes or for patients experiencing severe mania during pregnancy [II].
Manic or mixed episodes with psychotic features usually require treatment with an antipsychotic medication [II].
Mood Stabilizers cont’
Choices
Lithium
Monitor
Side effects
Anticonvulsants – Tegretol/Depakote
Different side effects for each
New – Lamictal/Topamax – more research
Atypical Antipsychotics
Frequently used, more research needed
Antianxiety Medications
Barbiturates
Benzodiazepines
Differences in pharmacodynamics
Half-lives
Where metabolized
Atypical Benzo’s
Ambien vs Sonata – sleep aids
Buspirone
Not shown to be addictive
Antianxiety Medications cont’
Antihistamines
Not addictive – can build tolerance
Beta blockers
Used as hypertensives
Interact with many other drugs
Assist in peripheral symptoms of anxiety
Antianxiety Medications cont’
Other notes
Withdrawal
Worse with short half lives
Anxiety can return
Difficult to end treatment
Dependence
Types according to Dr. Amen
Type 1: Classic ADD
Restlessness, hyperactivity, constant motion, troubles sitting still, talkative,
.
impulsive behavior, lack of thinking ahead
Type 2: Inattentive ADD
Short attention span (especially about routine matters), distractibility, disorganization, procrastination, poor follow-through/task completion.
Types con’t
Type 3: Overfocused ADD
Worrying, holds grudges, stuck on thoughts, stuck on behaviors, addictive behaviors, oppositional/argumentative.
Type 4: Limbic ADD
Sad, moody, irritable, negative thoughts, low motivation, sleep/appetite problems, social isolation, finds little pleasure.
Types con’t
Type 5: Temporal Lobe ADD
Inattentive/spacey/confused, emotional instability, memory problems, periodic intense anxiety, periodic outbursts of aggressive behavior seemingly triggered by small events or intense angry criticisms directed at himself for failures and frustrations, overly sensitive to criticism and slights by others, frequent headaches and/or stomachaches, learning difficulties, and serious misperceptions/distortions of people and situations.
Types con’t
Type 6: Ring of Fire ADD
A ring of overactivity in the brain scan image which surrounds most of the brain is the source of the name for this type of
ADD. too many thoughts, very hyper behavior, very hyper verbal expressiveness, a hypersensitivity to light, sound, taste, or touch.
Amen’s interventions
Type 1: Classic ADD
Stimulant medication (Ritalin, Adderall, etc.), a diet with more protein and less carbohydrates, intense aerobic exercise.
Type 2: Inattentive ADD
Stimulant medication, perhaps stimulating antidepressants (Welbutrin, for example), a diet with more protein and less carbohydrates, intense
Amen’s interventions
Type 3: Overfocused ADD
An antidepressant that has a dual focus on two brain transmitters (seratonin and dopamine) (Effexor, for example), and/or an antidepressant that enhances seratonin
(Prozac, Zoloft, Paxil, or others, for example). A stimulant medication may need to be added. A diet with less protein and increased complex carbohydrates will help, along with intense aerobic exercise.
Amen’s interventions
Type 4: Limbic ADD
An antidepressant that is also stimulating (Effexor or Welbutrin, for example), with a stimulant medication could be added; a balanced diet, and intense exercise.
Amen’s interventions
Type 5: Temporal Lobe ADD
Anticonvulsant medication (Neurontin,
Depakote for example), a stimulant could be added; a diet with more protein and less simple carbohydrates.
Type 6: Ring of Fire ADD
Anticonvulsant medication (Neurontin,
Depakote for example, a stimulant medication could be added; sometimes some of the newer, different anti-psychotic medications may help (Risperdal, or
Zyprexa); a diet with more protein and less simple carbohydrates.
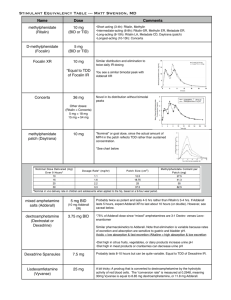
Types of Medications
Methylphenidate
Dextroamphetamine
Atomoxetene
Dexmethylphenidate
Antidepressants
SSRI’s
Tricyclics
Basic Elements of
Methylphenidate
Known as: Ritalin, Ritalin SR, Ritalin LA,
Concerta, Metadate ER, Metadate CD,
Focalin
Pharmacology: It is a CNS stimulant, which is chemically related to amphetamine
Preparations – 5, 10, 20 mg tabs; sustained release 20 mg tabs; LA 20, 30, and 40 mg capsules. The SR tablet should be swallowed and not crushed or chewed.
Concerta comes in 18 and 36 mg extended release tablets. Metadate CD 20 mg capsules; Metadate ER 10 – and 20 – mg tabs. Focalin 2.5, - 5-, 10 - mg tabs.
Methylphenidate, cont’d
Half-Life – 3-4 hours; 6-8 hours for sustained release
It’s a schedule II controlled substance, requiring a triplicate prescription
Pre-Drug Work-Up
Blood pressure and general cardiac status baseline and periodic blood counts and liver function tests
Weight and growth should be monitored in children
Methylphenidate, cont’d
Adverse Drug Reactions
Nervousness and insomnia; can be reduced by decreasing dose.
Cardiovascular – Hypertension, tachycardia, and arrhythmias.
CNS – Dizziness, euphoria, tremor, headache, precipitation of tics and Tourette’s syndrome, and rarely psychosis.
GI – Decreased appetite, weight loss.
Case reports of elevated liver enzymes and liver failure.
Hematological –Leukopenia and anemia have been reported
Growth Inhibition
Basic Elements of
Dextroamphetamine
Known as: Adderall, Adderall XR
Pharmacology:causes the release of norepinepherine from neurons. At higher doses, it will also cause dopamine and serotonin release
Preparations – Adderall 5-, 7.5-, 10-,
12.5-, 15-, 20-, 30-mg tablets; Adderall
XR 5-, 10-, 15-, 20-, 25-, 30-mg capsules.
Dextroamphetamine, cont’d
Half-Life – 10-25 hours
It’s a schedule II controlled substance, requiring a triplicate prescription
Pre-Drug Work-Up
Blood pressure and general cardiac status should be evaluated prior to initiating dextroamphetamine.
Can precipitate tics
Contraindicated in in patients with hypertension, hyperthyroidism, cardiac disease or glaucoma. It is not recommended for psychotic patients ot patients with a history of substance abuse.
Weight and growth should be monitored in all
Dextroamphetamine, cont’d
Adverse Drug Reactions
Side effects – most common side effects are psychomotor agitation, insomnia, loss of appetite, and dry mouth. Tolerance to loss of appetite tends to develop. Effect on sleep can be reduced by making sure no drug is given after
12 pm.
Cardiovascular – Palpitations, tachycardia, increased blood pressure.
CNS – Dizziness, euphoria, tremor, precipitation of tics, Tourette’s syndrome, and rarely, psychosis.
GI – Anorexia and weight loss, diarrhea,
Basic Elements of
Atomoxetene
Known as: Strattera
Pharmacology:works via presynaptic norepinepherine transporter inhibition
Preparations – 10, 18, 25, 40, and 60 mg capsules .
Atomoxetene, cont’d
Half-Life – approximately 4 hours
Not a schedule II controlled substance
Clinical Guidelines –
Dividing the dose may reduce some side effects
Dose reductions are necessary in presence of moderate hepatic insufficiency
Atomoxetine should not be used within 2 weeks of discontinuation of a MAO inhibitor.
Atomoxetine should be avoided inpatients with narrow angle glaucoma and, it should be used with caution in patients with tachycardia, hypertension, or cardiovascular disease.
It can be discontinued without taper.
Pregnancy C category.
Atomoxetene, cont’d
Adverse Drug Reactions
Cardiovascular – increased blood pressure and heart rate (similar to those seen with conventional psychostimulant).
BI – Anorexia, weight loss, nausea, abdominal pain.
Miscellaneous – Fatigue, dry mouth, constipation, urinary hesitancy and erectile dysfunction.
Basic Elements of
Dexmethylphenidate
Known as: Focalin, Focalin XR
Pharmacology:causes the release of dopamine from neurons. Is an isomer of Ritalin.
Preparations – Focalin 2.5, 5 ,10-mg tablets; Focalin XR 5-, 10-, 20-mg capsules.
Dexmethylphenidate, cont’d
Half-Life – 2.2 hours
It’s a schedule II controlled substance, requiring a triplicate prescription
Pre-Drug Work-Up
Blood pressure and general cardiac status should be evaluated prior to initiating
Dexmethylphenidate.
Can precipitate tics
Contraindicated in in patients with hypertension, hyperthyroidism, cardiac disease or glaucoma. It is not recommended for psychotic patients or patients with a history of substance abuse.
Weight and growth should be monitored in all
Dexmethylphenidate, cont’d
Adverse Drug Reactions
Side effects – most common side effects are psychomotor agitation, insomnia, loss of appetite, and dry mouth. Tolerance to loss of appetite tends to develop. Effect on sleep can be reduced by making sure no drug is given after
12 pm.
Cardiovascular – Palpitations, tachycardia, increased blood pressure.
CNS – Dizziness, euphoria, tremor, precipitation of tics, Tourette’s syndrome, and rarely, psychosis.
GI – Anorexia and weight loss, diarrhea,
Release Characteristics
Concerta Metadate
CD
Ritalin LA
30% 50% Immediate
Release
22%
Delayed
Release
78% 70% 50%
Technolog y
Oros Eurand SODAS
Other Medications
Dexadrine
Cylert
Since marketing in 1975, 13 cases of acute hepatic failure have been reported to the FDA.
11 resulted in death or transplant.
Attenade
Paxil
Wellbutrin
Zoloft
Trileptal
Celexa/Lexapro
Effexor
When to use, when to change
Side effects
Past history
Substance abuse
Efficacy
Onset time
Stimulant first line, Strattera second
Follow MD
Closing Thoughts
Stimulants still first line defense
Look at choice of drug based upon time of release
Be aware of study sponsor
Addictive nature
Subscribe to Medscape
Tools/Resources
ADD/ADHD Behavior-Change
Resource Kit
Teenagers with ADD: A Parents’ Guide www.myadhd.com
www.adhdhelp.com
www.amenclinic.com
ADDitude Magazine
References
American Academy of Pediatrics. Diagnosis and evaluation of the child with attentiondeficit/hyperactivity disorder. Pediatrics.
2000;105:1158-1170.
American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. DSM-IV-TR.
In: Disorders Usually First Diagnosed in Infancy, Childhood, or Adolescence: Diagnostic Criteria for
Attention-Deficit/Hyperactivity Disorder.
Washington, DC: American Psychiatric Association; 1994:92-
93.
National Institute of Mental Health. National Institutes of Health. Attention deficit hyperactivity disorder.
Available at: http://www.nimh.nih.gov/publicat/helpchild.cfm. Accessed April 19, 2002.
U.S. Department of Health and Human Services. Mental Health: A Report of the Surgeon General.
Available at: http://www.surgeongeneral.gov/library/mentalhealth/chapter3/sec4.html. Accessed April
19, 2002.
Dulcan M. Practice parameters for the assessment and treatment of children, adolescents, and adults with attention-deficit/hyperactivity disorder. J Am Acad Child Adolesc Psychiatry.
1997;369(suppl):855-
1215.
American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. DSM-IV-TR.
In: Disorders Usually First Diagnosed in Infancy, Childhood, or Adolescence: Diagnostic Criteria for
Attention-Deficit/Hyperactivity Disorder.
Washington, DC: American Psychiatric Association; 1994:92-
93.
American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. DSM-IV-TR.
In: Disorders Usually First Diagnosed in Infancy, Childhood, or Adolescence: Diagnostic Criteria for
Attention-Deficit/Hyperactivity Disorder.
Washington, DC: American Psychiatric Association; 1994:92-
93.
National Institute of Mental Health. National Institutes of Health. Attention deficit hyperactivity disorder —questions and answers. Available at: http://www.nimh.nih.gov/publicat/adhdqa.cfm.
Accessed April 19, 2002.
National Institute of Mental Health. National Institutes of Health. Attention deficit hyperactivity disorder
—questions and answers. Available at: http://www.nimh.nih.gov/publicat/adhdqa.cfm.
Accessed April 19, 2002.
American Psychiatric Association: Diagnostic and Statistical Manual of Mental Disorders, Fourth
Edition, Text Revision. Washington, DC, American Psychiatric Association, 2000.
Fauman, M. A. (2002). Study Guide to DSM-IV-TR. Washington, DC: American Psychiatric
Publishing, Inc.
www.pembertoncounseling.com