Chapter 20 - FacultyWeb
advertisement
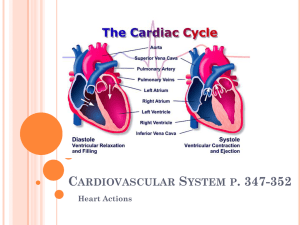
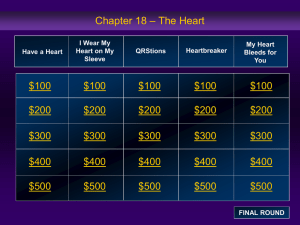
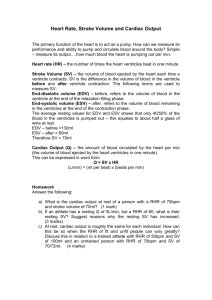
The region between the two pleural cavities that contains the heart and great vessels is called the ______? 1. 2. 3. 4. Mediastinum Visceral pericardium Parietal pericardium Pericardial cavity Which layer of pericardium touches the heart? 1. 2. 3. 4. Parietal pericardium Pericardial sac Fibrous pericardium Visceral pericardium Which of the following is true of cardiac muscle tissue? 1. Cardiac muscle cells are larger than skeletal muscle cells. 2. Cardiac muscle is not striated. 3. Cardiac muscle cells have intercalated discs. 4. Cardiac muscle cells are multinucleate. Which blood vessels bring blood back into the right atrium from systemic circulation? 1. Foramen ovale, pulmonary trunk, and ductus arteriosus 2. Superior and inferior venae cavae 3. Superior and inferior venae cavae and coronary sinus 4. Aorta, pulmonary trunk, and pulmonary veins How is eversion of the AV valves and backflow of blood into the atria prevented? 1. 2. 3. 4. Pressure of blood pushing against the valves Contraction of the ventricles Closure of the semilunar valves Tightening of chordae tendineae and contraction of papillary muscles Doris was born with a malformed pulmonary valve. How will that affect her circulation? 1. 2. 3. 4. Blood will flow more efficiently into her pulmonary trunk. Blood will regurgitate into her right atrium. Blood will flow back into her right ventricle. Deoxygenated blood will continuously pass around her systemic circuit. Why is the left ventricle more muscular than the right ventricle? 1. Because it pumps a larger volume of blood. 2. Because it contracts with force sufficient to push blood through the systemic circuit. 3. Because the papillary muscles are stronger. 4. Both 1 and 2 are correct Rick had a heart attack because of blockage of his right coronary artery. Which regions of his heart will be damaged by the blockage? 1. 2. 3. 4. SA node and AV node Interventricular septum and left atrium Portions of both ventricles 1 and 3 are correct. Why is resting HR somewhat slower than the 80– 100 bpm set by the SA node? 1. The AV node slows the heart to an average between its own rate and that of the SA node. 2. Parasympathetic innervation slows the HR. 3. The AV node takes over causing the HR to be 40–60 bpm. 4. None of these is correct. What is the importance of the 100 msec delay at the AV node? 1. Atria must contract before the ventricles. 2. AV valves must have time to close. 3. Contraction of papillary muscles must begin before ventricular contraction. 4. Tachycardia results if the delay is absent. On an ECG reading, what does the P Wave indicate? 1. 2. 3. 4. Ventricular contraction An abnormal heart condition Atrial depolarization Atrial diastole What factor could cause an increase in the size of the QRS complex of an electrocardiogram recording? 1. 2. 3. 4. An increase in heart rate A decrease in blood volume A decrease in blood pressure An increase in heart size What condition contributes to a reduction in the size of the T Wave? 1. 2. 3. 4. Long-term high fat intake Damage to the conducting pathway Damage to the AV node Coronary ischemia Why is there no wave corresponding to atrial repolarization on an ECG reading? 1. It is masked by the QRS complex. 2. Atrial repolarization produces no electrical effect at all. 3. It is masked by the P Wave. 4. None of these is correct. What event is taking place during the Q-T interval? 1. A single cycle of the cardiac cycle 2. An action potential 3. A single cycle of atrial depolarization and repolarization 4. A single cycle of ventricular depolarization and repolarization What is happening during ventricular systole of the cardiac cycle? 1. 2. 3. 4. Rising atrial pressures push blood into the ventricles. All heart valves are closed and ventricles are relaxing. Both ventricular contraction and atrial diastole take place. Pressure in ventricles drops, which forces the semilunar valves closed. When during the cardiac cycle do ventricles contain their maximal amount of blood? What is this quantity called? 1. 2. 3. 4. At the end of ventricular systole/ESV At the end of atrial systole/EDV At the end of ventricular diastole/EDV 2 and 3 are correct. How is Cardiac Output (CO) calculated? 1. 2. 3. 4. CO ml/min = (EDV–ESV) x SV CO ml/min = HR bpm x SV ml/beat CO ml/min = ESV/EDV 1 and 2 are correct Benjamin has an EDV of 120 ml, an ESV of 45 ml, which gives him an SV of 75 ml. What is his ejection fraction? 1. 2. 3. 4. 45% 75% 37.5% 60% What is the most important factor in considering cardiac function over time? 1. 2. 3. 4. Cardiac output Heart rate Stroke volume End systolic volume Where is the ANS headquarters for cardiovascular control? 1. 2. 3. 4. Cardiac plexus SA and AV nodes Medulla oblongata Cervical and upper thoracic ganglia How does damage to the cardioinhibitory center of the medulla affect heart rate? Why? 1. 2. 3. 4. Heart rate increases/sympathetic dominance Heart rate decreases/parasympathetic dominance Heart rate remains unchanged/autonomic tone makes delicate adjustments Heart rate increases/only the SA node will be controlling heart rate What is the effect on heart rate of NE binding to beta-1 receptors? 1. 2. 3. 4. Increases rate of depolarization Decreases heart rate Increases heart rate 1 and 3 are correct Which of the following affect(s) the rate of venous return? 1. 2. 3. 4. Cardiac output Stroke volume Heart rate All of the above are correct Frank has just run a marathon and his heart is beating extremely rapidly. What happens to the length of diastole and filling time? 1. Both increase 2. Both decrease 3. Length of diastole increases/filling time decreases 4. Length of diastole decreases/filling time increases Why is ESV lower when you are actively exercising? 1. 2. 3. 4. SV decreases and filling time increases. EDV is very low and ventricular muscle is stretched very little. EDV increases and ventricular muscle produces more forceful contractions ejecting more blood. Parasympathetic stimulation causes it.