External Auditory Canal Foreign Body
advertisement
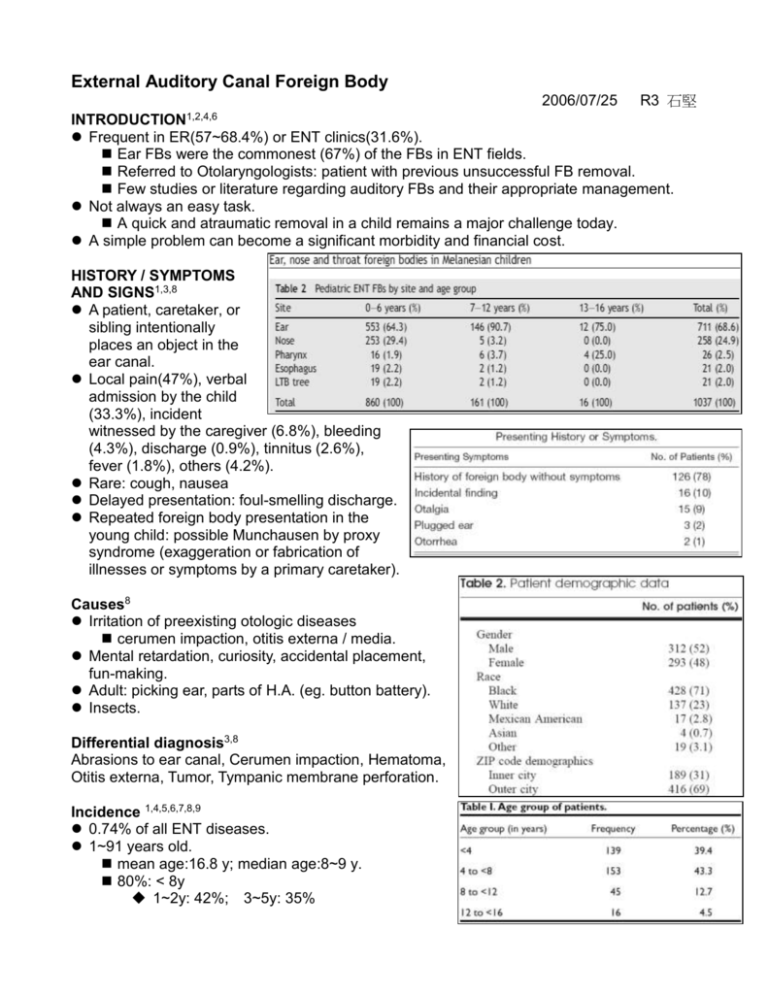
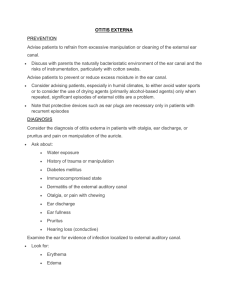
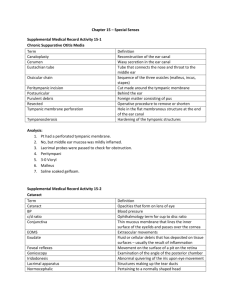
External Auditory Canal Foreign Body 2006/07/25 R3 石堅 INTRODUCTION1,2,4,6 Frequent in ER(57~68.4%) or ENT clinics(31.6%). Ear FBs were the commonest (67%) of the FBs in ENT fields. Referred to Otolaryngologists: patient with previous unsuccessful FB removal. Few studies or literature regarding auditory FBs and their appropriate management. Not always an easy task. A quick and atraumatic removal in a child remains a major challenge today. A simple problem can become a significant morbidity and financial cost. HISTORY / SYMPTOMS AND SIGNS1,3,8 A patient, caretaker, or sibling intentionally places an object in the ear canal. Local pain(47%), verbal admission by the child (33.3%), incident witnessed by the caregiver (6.8%), bleeding (4.3%), discharge (0.9%), tinnitus (2.6%), fever (1.8%), others (4.2%). Rare: cough, nausea Delayed presentation: foul-smelling discharge. Repeated foreign body presentation in the young child: possible Munchausen by proxy syndrome (exaggeration or fabrication of illnesses or symptoms by a primary caretaker). Causes8 Irritation of preexisting otologic diseases cerumen impaction, otitis externa / media. Mental retardation, curiosity, accidental placement, fun-making. Adult: picking ear, parts of H.A. (eg. button battery). Insects. Differential diagnosis3,8 Abrasions to ear canal, Cerumen impaction, Hematoma, Otitis externa, Tumor, Tympanic membrane perforation. Incidence 1,4,5,6,7,8,9 0.74% of all ENT diseases. 1~91 years old. mean age:16.8 y; median age:8~9 y. 80%: < 8y 1~2y: 42%; 3~5y: 35% highest incidence: 0~6y Male:female ≒ 1:1 (Japan = 3:2; Singapore = 2:1) Right:Left ≒ 1:1 (Bilateral: 0.8%) Peaking: during July ~ August, organic FBs. Treated within 24hr: 46~92%; 15% within 3days, 8% >1week. Incidentally finding: 5%. Previous attempts: 46~48%. Organic : inorganic = 4:6 Suburb > downtown Types of FBs1,2,6 Overall (1~91y) Pediatric patient FB type of the patients Remove FB under direct vision. Firm, round FBs were removed more successfully under otomicroscope. Location Lateral 1/3 v.s. medial 2/3 of the EAC. EAC narrows at the junction of cartilaginous and osseous portions. Potentially painful and traumatic: the skin overlying the periosteum is exquisitely tender, highly vascular, and not much affected by topical anesthetics. MANAGEMENT6,8,9 Experience and skills of the Otolaryngologists. Seen on directed vision (90.6%) The type, shape, size of FB, condition of the EAC and visibility of the TM. Head mirror with a strong light source, otoscope, ear speculum. Instrumentation: tip suctions, alligator forceps, Hartman forceps, ear curette, wire loops, right-angle ball hooks. Stabilize the patient's head, fix your hand against it, holding the instrument loosely to reduce the risk of injury should the patient move suddenly. Alligator forceps will push a large, hard foreign body farther into the ear. One drop of cyanoacrylate (Super Glue) to adhere to a smooth, clean, dry foreign body. Touch it to the foreign body, hold for ten seconds, then pull. Live insects: Quite painful, significant amount of physical and emotional distress. Initial priority: to kill or immobilize the insect. mineral oil: more effective than lidocaine for immobilizing cockroaches. Subsequent microscope examination: to be sure no insect anatomic parts left remaining barbed appendages delayed EAC inflammation. Aural irrigation Nonimpacted, relatively small FBs. The integrity of the tympanic membrane must be established by pneumatoscopy before irrigating. Warm solution at body temperature. Irrigation syringe, standard syringe and scalp vein needle catheter cut short. Hygroscopic objects: vegetables, beans, food matter. Swell with subsequent greater EAC impaction on contact with moisture. Indications for otomicroscope. Failure to remove foreign body on initial attempt(s). (46~48%) Existent injury to the external auditory canal or tympanic membrane. Round solid subjects. (78%) Object wedged in the medial external auditory canal or up against tympanic membrane. Glass or other sharp-edged foreign body. Special circumstances such as insects, putty, and disc batteries. Uncooperative patient Restrained: child seated in an adult’s lap in the exam chair with the child’s arms and torso held securely by the adult. An additional staff member immobilize the child’s head. Only one or two chances before the child loses his patience and becomes uncooperative. Sedation (19.7%): Ketamine, Dormicum (Midazolam). General anesthesia for Operative Extraction: 30~6% (88% <7y) Mask inhalation without intubation. Indications for otomicroscope in younger children. End-aural incision. (India) After removal: thorough examination of the EAC and tympanic membrane. Opposite ear and nostrils should be examined. Not uncommon for multiple foreign bodies in the same child. Uncomplicated, atraumatic foreign body removal: require no further follow-up care. COMPLICATIONS6,8,9 Not related to age and gender. Factors: (i) irregular shape of the FB, namely, stone, (ii) duration of lodgments as longer stay (>24hr) in EAC leads to otitis externa, (iii) degree of cooperation of the child during removal, (iv) experience of the surgeon. Failure of FB removal(22.2%), laceration(5.1%), perforated tympanic membrane(1~6%) Other complications(4.3%): bleeding, hematoma, edema, traumatic otitis externa. Injury to tympanic membrane or ossicles: audiogram. Prolonged FBs: otitis media / externa. Treated with antibiotic or steroid otic drops and given water precautions until healing. BUTTON BATTERY INJURY8,10 Dry cell, mercury cell and alkaline. Electrolyte: sodium hydroxide or potassium hydroxide. Smooth and shiny appearance makes them quite attractive and noticeable to children. Size: 7.9~23mm diameters, 1~10 g in weight. In 97% of cases, the size of the battery is less than 15mm. 44.6% were intended for use in a hearing aid. 32.8% were removed from the child’s own hearing aid. Majority in the 0~5y (61~71%); peak incidence between 1~2y; 57% are male. children of that age range are more able to obtain and remove the batteries from those products that contain them. 5~12y: 5.4% Presenting to ER: 3~24h. Symptoms: no signs or symptoms. non-specific signs: pain, cough, vomiting, irritability, fever and tachycardia. More specific s/s: EAC ulceration, foul or dark otorrhea, mimicking malignant otitis externa. Mechanisms of injury: liquefactive necrosis extending into deep tissues. Electrolyte leakage marked ulceration within 2 h of placement. necrosis of the inner muscularis layer after 1~2 h. progressing to full thickness necrosis from 2~4 h. Alkali produced de novo 2H2O + 2e− → 2OH− + H+ Hydrogen ions accumulates at the anode more substantial damage. A mercury cell: 1ml of 13% sodium hydroxide after 48 h of mucosa contact. Mercury toxicity Theoretical risk Only 2 two case reports: no systemic s/s of mercury toxicity, treated with oral chelators. Lethal dose of mercuric salts: 0.5~1.0g Mercury button batteries: 0.9~21g of mercuric oxide, poorly absorbed reduced to elemental mercury, virtually non-toxic. Pressure necrosis Theoretical risk, no evidence or case reports. Should never be irrigated before removal. After removal, the canal should be irrigated to remove alkalai residue. Complications: tympanic membrane perforation, EAC stenosis. Reference: 1. Thompson SK, Wein RO, Dutcher PO. External auditory canal foreign body removal: management practices and outcomes. Laryngoscope. 2003 Nov;113(11):1912-5. 2. Schulze SL, Kerschner J, Beste D. Pediatric external auditory canal foreign bodies: a review of 698 cases. Otolaryngol Head Neck Surg. 2002 Jul;127(1):73-8. 3. Robin Mantooth. Foreign Bodies, Ear. http://www.emedicine.com/emerg/topic185.htm 4. Wada I, Kase Y, Iinuma T. Statistical study on the case of aural foreign bodies. Nippon Jibiinkoka Gakkai Kaiho. 2003 Jun;106(6):678-84. 5. Balbani AP, Sanchez TG, Butugan O, Kii MA, Angelico FV Jr, Ikino CM, D'Antonio WE. Ear and nose foreign body removal in children. Int J Pediatr Otorhinolaryngol. 1998 Nov 15;46(1-2):37-42. 6. Endican S, Garap JP, Dubey SP. Ear, nose and throat foreign bodies in Melanesian children: An analysis of 1037 cases. Int J Pediatr Otorhinolaryngol. 2006 May 15. 7. Ng KC, Sim TP. Otorhinolaryngeal foreign bodies in children presenting to the emergency department. Singapore Med J. 2005 Apr;46(4):172-8. 8. Ansley JF, Cunningham MJ. Treatment of aural foreign bodies in children. Pediatrics. 1998 Apr;101(4 Pt 1):638-41. 9. Mishra A, Shukla GK, Bhatia N. Aural foreign bodies. Indian J Pediatr. 2000 Apr;67(4):267-9. 10. Lin VY, Daniel SJ, Papsin BC. Button batteries in the ear, nose and upper aerodigestive tract. Int J Pediatr Otorhinolaryngol. 2004 Apr;68(4):473-9.