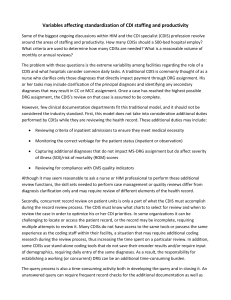
Productivity and staffing example
advertisement

Productivity and staffing example Determining an adequate number of staff and ensuring acceptable levels of productivity for a CDI department can be overwhelming. There are many variables to consider, including staff experience, the type of record system in the facility, and how much data each CDI specialist (CDIS) is required to track and enter during chart reviews. Productivity is also affected when CDI staff is additionally responsible for quality initiatives, case management duties, validation of pre–bill drop records, or formal physician education, among other duties. Although most organizations would prefer to have a simple formula for calculating CDI staffing ratios (e.g., hire X number of CDISs per X number of discharges per year), there is currently too much variation within the industry to allow for a one-size-fits-all approach. As such, ACDIS recommends that each organization develop its own determination of staffing and productivity levels based on its own unique attributes and the mission of its CDI department (see related document “variables affecting standardization of CDI staffing and productivity”). One basic way to determine staffing needs within an organization is to base it on the number of hours each CDIS works per year divided by the time it takes to perform an average review based on the results of a time study. When using this method, you must calculate and deduct non-review time (i.e., establishment of the work list, physician training, development of educational materials, etc.). Following is an example of how a CDI department at a fictional hospital (Hospital A) determines its staffing needs and productivity expectations. Productivity: Identify and omit time spent on activities other than initial or follow-up reviews, including query follow-up. Hospital A requires its CDISs to spend two hours at the end of each day for DRG and coding reconciliation. It also allots a half-hour lunch break and two 15-minute breaks, leaving five hours of daily review time per CDIS. Determine how many weeks per year your CDISs work. Employees at Hospital A are given two weeks’ vacation, 10 paid holidays, and five sick days, reducing the work year to 47 weeks. Multiply the hours of reviews each day by the number of days in a workweek by the number of workweeks per year. For Hospital A, this works out to 5 hours x 5 days x 47 weeks, meaning each CDIS spends approximately 1175 hours performing chart review per year. Once you determine your baseline of how many hours are spent annually completing reviews, count how many patients are reviewed by each CDIS and determine how long it takes to perform an average chart review. Track each floor separately by number of reviews, number of new reviews, and number of queries. This allows for an equal distribution of assignments and a more realistic average, since certain types of patient charts will require more queries and detailed reviews than others. At Hospital A, CDISs review an average of 20 patients in five hours, so each review takes approximately 15 minutes. (Note: Reviewers are assumed only to review charts for principal diagnosis and secondary diagnoses, and do not perform other duties such as case management, observation, etc.) Staffing: To determine your staffing needs, determine how many reviewable patients were admitted last fiscal year in the insurances reviewed by your department. (Note: You may wish to carve out obstetrics, neonates, rehab, or psych; or review DRG payers only; etc.) For example, if ABC Insurance had 153 patients admitted to Hospital A, and it takes 15 minutes to review each of those charts (as calculated above), then the total number of hours for review would be 32.51. Add up the total number of hours and divide this number by the total number of CDI work hours. This result is the number of FTEs you need to staff your program. For example, at Hospital A, there are three insurers reimbursed via DRGs, and 5,000 hours of review time are required to cover all three. Based on 1,175 hours of annual review time per CDS, approximately four fulltime FTE CDSs are needed. Use of time studies You can also use a time study to determine how much time it takes for an average CDIS to complete a review. A time study is a method used to understand how much time it takes an employee to complete each of his or her daily tasks. A time study can be complex, or it can be simply a log where the employee keeps track of how much time is spent on each discrete job function. For a CDIS, a typical day would include identifying which reviews must be completed for the day. Some organizations may have a tool that automatically creates work lists for the CDI staff, while other organizations may rely on a manual process. Note that the CDIS will require access to all new admissions, all discharges, the status of open queries, and the status of current open reviews (i.e., subsequent reviews) in order to determine his or her daily work list. There are many variables that influence CDI productivity (see document “Variables impacting standardization of CDI staffing and productivity”). An initial review in which the working DRG is established requires a CDIS to review the history and physical as well as any applicable historical patient information, emergency room records, transfer records, and the treatment plan. Depending on the experience and resources available to the CDIS, performing an initial review and establishing a working DRG can take 15–30 minutes or longer. Note that locating and reviewing the record takes time, as does inputting the findings into an encoder. When elements are missing from the medical record or an interaction with the medical staff is required, this can lengthen the time needed to complete the initial review. The type of health record used (electronic, paper, or hybrid) can also influence productivity. The amount of time needed to complete a follow-up review will also vary depending on the resources and experience of the CDIS. Organizations where an encoder is integrated into the CDI documentation tool will be more productive than those where the CDIS must reenter his or her diagnoses into the encoder each review. Although the working DRG is already established and most CDI are knowledgeable about what diagnoses are CCs or MCCs, in order to evaluate the severity of illness (SOI) and risk of mortality (ROM) values of a case one must enter all applicable diagnoses, as the number of diagnoses and their relationship to each other impacts SOI and ROM. (A robust grouper embedded in the CDI module can minimize or eliminate some of these tasks.) There is also much more documentation to review during a follow-up review than an initial review. However, subsequent reviews may take less time. Proficiency in conducting reviews varies with experience. Also consider that organizations where CDISs rotate through service lines may be less productive than those in which CDISs specialize in one or two services—specialized CDISs will likely be more productive due to their familiarity with the codes and DRGs, as well as their relationships with the medical staff. Lastly, queries can be a time-consuming activity for CDISs depending on the resources available at the organization. Organizations that rely on a paper query process require the CDIS to review the medical record on a daily basis to check for query responses. If the query is not part of the medical record, the CDIS must review all new documentation to see whether the query was addressed. Depending on the involvement of the medical staff, it can be a time-consuming process to issue a query as well as to obtain input from the physician. Once you have completed a time study to determine the average length of time it takes the staff to complete basic CDI responsibilities, you can use this information to determine staffing and productivity.



![CDI+Impact+on+RAC[1]](http://s2.studylib.net/store/data/005600152_1-87991b5e70e02cff6dbbfebd48f7ff80-300x300.png)