DATE OF ADMISSION: DATE OF DISCHARGE: ADMISSION
advertisement
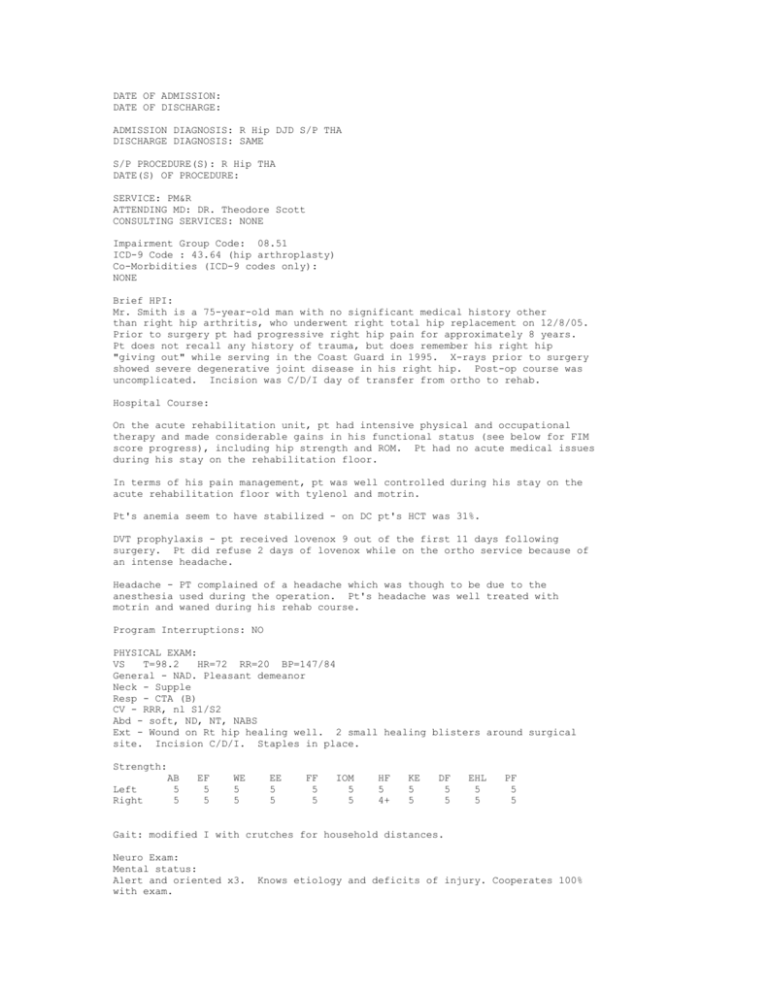
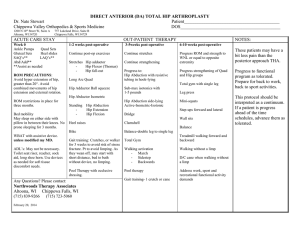
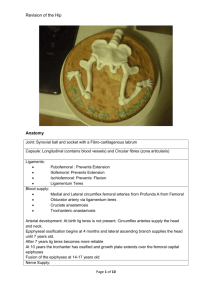
DATE OF ADMISSION: DATE OF DISCHARGE: ADMISSION DIAGNOSIS: R Hip DJD S/P THA DISCHARGE DIAGNOSIS: SAME S/P PROCEDURE(S): R Hip THA DATE(S) OF PROCEDURE: SERVICE: PM&R ATTENDING MD: DR. Theodore Scott CONSULTING SERVICES: NONE Impairment Group Code: 08.51 ICD-9 Code : 43.64 (hip arthroplasty) Co-Morbidities (ICD-9 codes only): NONE Brief HPI: Mr. Smith is a 75-year-old man with no significant medical history other than right hip arthritis, who underwent right total hip replacement on 12/8/05. Prior to surgery pt had progressive right hip pain for approximately 8 years. Pt does not recall any history of trauma, but does remember his right hip "giving out" while serving in the Coast Guard in 1995. X-rays prior to surgery showed severe degenerative joint disease in his right hip. Post-op course was uncomplicated. Incision was C/D/I day of transfer from ortho to rehab. Hospital Course: On the acute rehabilitation unit, pt had intensive physical and occupational therapy and made considerable gains in his functional status (see below for FIM score progress), including hip strength and ROM. Pt had no acute medical issues during his stay on the rehabilitation floor. In terms of his pain management, pt was well controlled during his stay on the acute rehabilitation floor with tylenol and motrin. Pt's anemia seem to have stabilized - on DC pt's HCT was 31%. DVT prophylaxis - pt received lovenox 9 out of the first 11 days following surgery. Pt did refuse 2 days of lovenox while on the ortho service because of an intense headache. Headache - PT complained of a headache which was though to be due to the anesthesia used during the operation. Pt's headache was well treated with motrin and waned during his rehab course. Program Interruptions: NO PHYSICAL EXAM: VS T=98.2 HR=72 RR=20 BP=147/84 General - NAD. Pleasant demeanor Neck - Supple Resp - CTA (B) CV - RRR, nl S1/S2 Abd - soft, ND, NT, NABS Ext - Wound on Rt hip healing well. 2 small healing blisters around surgical site. Incision C/D/I. Staples in place. Strength: AB Left 5 Right 5 EF 5 5 WE 5 5 EE 5 5 FF 5 5 IOM 5 5 HF 5 4+ KE 5 5 DF 5 5 EHL 5 5 PF 5 5 Gait: modified I with crutches for household distances. Neuro Exam: Mental status: Alert and oriented x3. with exam. Knows etiology and deficits of injury. Cooperates 100% Fluent speech and comprehension Functional Progress: FUNCTIONAL STATUS AT DISCHARGE: SELF CARE: Admission Eating 7 Grooming 6 Bathing 2 Dressing UB 7 Dressing LB 2 Toileting 6 Sphincter Control Bladder 7 Bowel 6 Transfers: bed,chair,w/c 5 Toilet 5 Tub 5 Locomotion: Walk 5 Wheelchair 6 Stairs 5 Communication: Comprehension 7 Expression 7 Social Cognition Social interaction 7 Problem solving 7 Memory 7 Discharge 7 6 6 7 6 6 7 7 6 6 6 6 6 7 7 7 7 7 Key/Grading scale: (FIM Levels) No Helper: 7 = Ind = completely independent 6 = Mod (I) = modified independent (uses device or required extra time) Helper - Modified dependence 5 = Sup = supervision only (no physical assist) 4 = Min = minimal assist (1-25% assist) 3 = Mod = moderate assist (26-50% assist) Helper - Complete Dependence 2 = Max = maximal assist (51-75% assist) 1 = Dependent = total assist (76-100% assist) ADL CGA V/C WFL = = = = Activities of Daily Living Contact Guard Assist Verbal Cues Within Functional Limits (Not Limiting Functional Activities) ALLERGIES: NKDA DC Medications FeSO4 325mg po tid Vitamin C 25mg po qday PRN Motrin, Tylenol D/C Activity: WBAT D/C Diet: Regular D/C Precautions: Fall D/C Education: PT has been taught a home program to continue working on gait training and stretching/strengthening of LE muscles. Patient voiced understanding. Also advised pt to eat a healthy diet low in salt and fat as well as refrain from EtOH and nicotine for continued general health. D/C Follow-up Orthopedics - pt has been scheduled for f/u with ortho in Honolulu on 12/22 @ 10:30am. Pt will have his staples removed in HI at that appointment. PT - pt will see have outpatient PT 1x week for strength, mobility, ambulation, and ROM for the next four weeks in HI. PT will be notified about this first appointment. PCP - Pt should schedule to have an appointment with his PCP within 2-3 weeks from time of discharge. Pt's PCP is Dr. James Woods. We will attempt to fax this DC summary to his office. This DC summary as well as the assessment and plan were discussed with and agreed upon by the patient as well as Dr. Scott, the attending physician.