Discharge Summary 4
advertisement
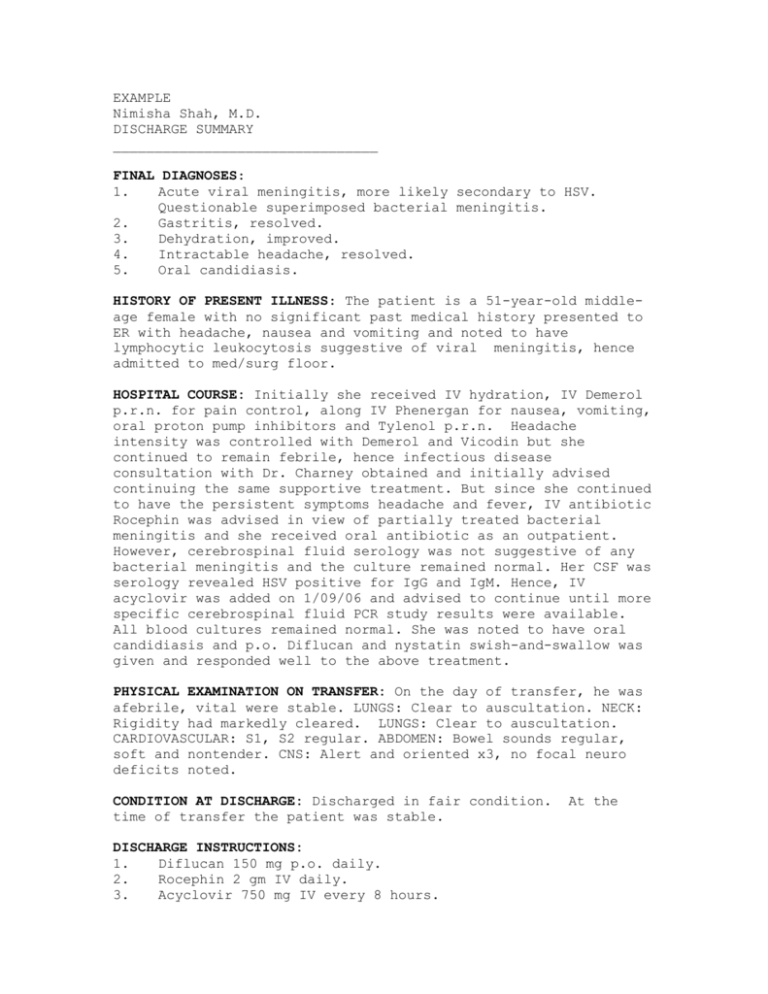
EXAMPLE Nimisha Shah, M.D. DISCHARGE SUMMARY ________________________________ FINAL DIAGNOSES: 1. Acute viral meningitis, more likely secondary to HSV. Questionable superimposed bacterial meningitis. 2. Gastritis, resolved. 3. Dehydration, improved. 4. Intractable headache, resolved. 5. Oral candidiasis. HISTORY OF PRESENT ILLNESS: The patient is a 51-year-old middleage female with no significant past medical history presented to ER with headache, nausea and vomiting and noted to have lymphocytic leukocytosis suggestive of viral meningitis, hence admitted to med/surg floor. HOSPITAL COURSE: Initially she received IV hydration, IV Demerol p.r.n. for pain control, along IV Phenergan for nausea, vomiting, oral proton pump inhibitors and Tylenol p.r.n. Headache intensity was controlled with Demerol and Vicodin but she continued to remain febrile, hence infectious disease consultation with Dr. Charney obtained and initially advised continuing the same supportive treatment. But since she continued to have the persistent symptoms headache and fever, IV antibiotic Rocephin was advised in view of partially treated bacterial meningitis and she received oral antibiotic as an outpatient. However, cerebrospinal fluid serology was not suggestive of any bacterial meningitis and the culture remained normal. Her CSF was serology revealed HSV positive for IgG and IgM. Hence, IV acyclovir was added on 1/09/06 and advised to continue until more specific cerebrospinal fluid PCR study results were available. All blood cultures remained normal. She was noted to have oral candidiasis and p.o. Diflucan and nystatin swish-and-swallow was given and responded well to the above treatment. PHYSICAL EXAMINATION ON TRANSFER: On the day of transfer, he was afebrile, vital were stable. LUNGS: Clear to auscultation. NECK: Rigidity had markedly cleared. LUNGS: Clear to auscultation. CARDIOVASCULAR: S1, S2 regular. ABDOMEN: Bowel sounds regular, soft and nontender. CNS: Alert and oriented x3, no focal neuro deficits noted. CONDITION AT DISCHARGE: Discharged in fair condition. time of transfer the patient was stable. DISCHARGE INSTRUCTIONS: 1. Diflucan 150 mg p.o. daily. 2. Rocephin 2 gm IV daily. 3. Acyclovir 750 mg IV every 8 hours. At the 4. 5. 6. 7. 8. 9. 10. Tylenol p.r.n. Phenergan 12.5 mg IV every 6 as needed. Protonix 50 mg one p.o. daily. Vicodin 7.5 SR 100 p.o. every 4 as needed for headache. CBC, Chem-7 twice a week. Will follow up with cerebrospinal fluid PCR study and inform Dr. Charney. Will request continued followup.