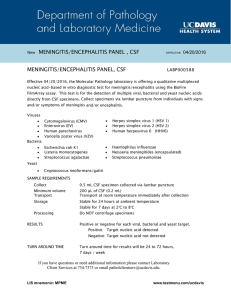
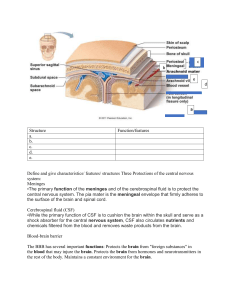
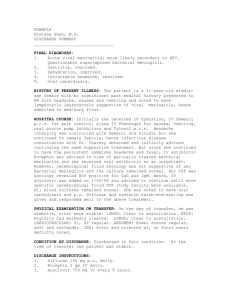
Meningitis Meningitis ▫ Acute infection of the meninges ▫ Viral or bacterial ▫ Almost any bacteria entering the body can cause meningitis Pathophysiology ▫ Invasion may occur at choroid plexus or directly thru an opening in the dura ▫ Organisms colonize in the CSF, leading to inflammation of the meninges that contains it. ▫ Exudate forms, meninges then become thickened and adhesions form leading to hydrocephalus ▫ Arteries supplying the subarachnoid space maybe inflamed, leading to rupture or thrombosis of these vessels ▫ Severe cases, lead to cerebral edema and Iicp, vasculitis and cerebral infarction Manifestations ▫ Classical sign Nuchal rigidity Brudzinski’s sign Kernig’s sign photophobia ▫ Other s/sx ▫ Headache ▫ Fever ▫ Tachycardia ▫ Nausea vs vomiting Medical management ▫ Diagnosed by lumbar puncture ▫ Medications ▫ Respiratory isolation ▫ Cool, dark quit room ▫ Maintain hydration ▫ Prevent injury ▫ Diagnostic evaluation ▫ Complete blood count (CBC) with differential ▫ Detect an elevated leukocyte count in bacterial and viral meningitis ▫ Lumbar puncture ▫ Elevated CSF pressure ▫ Cloudy or milky white CSF ▫ High protein level ▫ Positive gram stain and culture that usually identifies the infecting organism unless it’s a virus ▫ Depressed CSF glucose concentration ▫ CSF evaluation for pressure, leukocytes, protein, glucose ▫ MRI/CT scan ▫ With and without contrast rules out cerebral hematoma, hemorrhage or tumor ▫ Ct scan with contrast to detect abscesses ▫ Low CD4 counts indicate immunosuppression in HIV positive patients and other patients with immunosuppressive disorders ▫ Latex agglutination may be positive for antigens in meningitis ▫ Chest X-rays ▫ May reveal pneumonitis or lung abscess, tubercular lesions, or granulomas secondary to fungal infection ▫ Laboratory diagnosis of bacterial meningitis ▫ Lumbar puncture ▫ Should be performed in all cases whenever the diagnosis of meningitis is known or suspected on the basis of clinical signs ▫ Contraindications ▫ Presence of significant cardio-pulmonary compromise and shock ▫ Signs of increased Icp ▫ Suspected case of space occupying lesion ▫ Infection in the area that the spinal needl will traverse to obtain CSF ▫ Hematologic problems ▫ CSF findings in bacterial meningitis ▫ CSF pressure-usually elevated ▫ CSF cells count and chemistry ▫ Leukocytosis- >1000/Cumm %PMN-90% ▫ Glucose <40mg/dl ▫ CSF blood to glucose ratio <0.4 ▫ Protein 50-500mg/dl ▫ Stained smears of CSF ▫ Gram stain + for bacteria ▫ AFB smear – ▫ India ink – ▫ CSF culture ▫ a negative culture does rule out meningitis Treatment ▫ Antibiotics ▫ Adjunct therapy ENCEPHALITIS Encephalitis ▫ Inflammatory process of CNS with altered function of brain and spinal cord ▫ Variety of causative organisms- viral most frequent ▫ Vector reservoir: mosquitoes and ticks ▫ Two forms ▫ Primary: occurs when a virus invades and replicates within the brain ▫ Postinfectious (parainfectious) ▫ Brain inflammation that develops in combination with other viral illness or following administrations of vaccines such as measles, mumps and rubella due to hypersensitivity reaction that leads to demyelination of nerves Clinical manifestations ▫ ▫ Onset sudden or gradual ▫ Malaise ▫ Fever ▫ Headache/dizzines s ▫ Stiff neck ▫ Nausea/vomiting ▫ Ataxia ▫ Speech difficulties Severe encephalitis ▫ High fever ▫ Disorientation/stu por/coma ▫ Seizures/spasticty ▫ Ocular palsies ▫ Paralysis ▫ IICp ▫ Diagnostic evaluation ▫ CSF analysis ▫ EEG ▫ MRI ▫ PET ▫ Medical management ▫ Prescribed diureticsmannitol(decrease edema) ▫ Antibioticsacyclovir (for herpes encephalitis Nursing diagnosis ▫ Risk for ineffective airway clearance r/t unresponsiveness and inability to clear secretions ▫ Ineffective airway clearance ▫ Altered thought process r/t increased in ICP Nursing intervention ▫ Maintain a patent airway ▫ Assess pupil size and reaction, LOC, strength and motion of the extremities, response to noxious stimuli ▫ Endotracheal intubation, oxygen theray and mechanical ventilation ▫ Ongoing neurological assessment ▫ Document changes in the pt’s condition and initiates proper care immediately ▫ Turn, cough and deep breath every 2 hours ▫ Maintain airway, breathing and circulation ▫ Maintain an open airway with suctioning as needed ▫ Limit the effects of immobility such as skin care, ROM, turning and positioning schedule ▫ Reorient patient to time, place and person as needed ▫ ] BRAIN ABSCESS Brain abscess ▫ CNS abscesses ▫ Focal pyogenic infections of the CNS ▫ Exert their effects mainly by ▫ Direct involvement & destruction of the brain o spinal cord ▫ Compression of parenchyma ▫ Elevation of intracranial pressure ▫ Interfering with blood and or CSF flow ▫ Include: ▫ brain abscess ▫ Subdural empyema ▫ Intracranial epidural abscess ▫ Spinal epidural abscess ▫ Spinal cord abscess Pathophysiology ▫ Begins as localized cerebritis (1-2wks) ▫ Evolves into a collection of pus surrounded by a wellvascularized capsule (3-4wks) ▫ Lesion evolution: ▫ Days 1-3: “early cerebritis stage” ▫ Days 4-9: “late cerebritis stage” ▫ Days 10-14: “early capsule stage” ▫ > day 14: late capsule stage” Etiologies ▫ Direct spread from contiguous foci (40-50%) ▫ Hematogenous (25-35%) ▫ Penetrating trauma /surgery(10%) ▫ Cryptogenic (15-20%) ▫ Direct spread ▫ Occurs by: ▫ Direct extension through infected bone ▫ Spread through emissary veins, diploic veins, local lymphatics ▫ The contiguous foci include ▫ Otitis media/mastoiditis ▫ Sinusitis ▫ Dental infection (<10%), typically with molar infections ▫ meningitis ▫ Hematogenous spread (from remote foci) ▫ Sources: ▫ Empyema, lung abscess, bronchiectasis, endocarditis, wound infections, etc… ▫ May be facilitated by cyanotic HD, AVM ▫ Results in brain abscess at middle cerebral artery distribution ▫ Often multiple Clinical manifestations ▫ Non-specific symptoms ▫ Mainly due to the presence of a space occupying lesion ▫ N/V, lethargy, focal neuro signs, seizures ▫ Signs/symptoms influenced by ▫ Location, size, virulence of organism, presence of underlying condition ▫ headache ▫ often dull, poorly localized, non-specific abrupt, extremely severe headache ▫ Sudden worsening headache with rupture of brain abscess into ventricle (often fatal) ▫ Location & clinical features ▫ Frontal lobe: headache, drowsiness, inattention, hemiparesis, motor speech disorder ▫ Temporal lobe: ipsilateral headache, aphasia, visual field defect ▫ Parietal lobe: headache, visual field defects, endocrine disturbances ▫ Cerebellum: nystagmus, ataxia, vomiting, dysmetria ▫ Diagnosis ▫ High index of suspicion ▫ Contrast CT or MRI ▫ Drainage/biopsy Treatment ▫ Combined medical & surgical ▫ Aspiration or excision ▫ Empirical antibiotics