Learning-and-teaching-motor-skills
advertisement

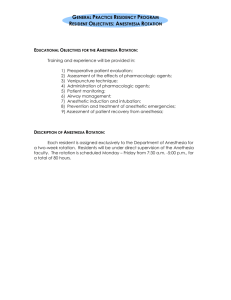
REVIEW ARTICLE Learning and Teaching Motor Skills in Regional Anesthesia A Different Perspective Reuben J. Slater, BSc (Hon), BMed, FANZCA,* Damian J. Castanelli, MBBS, MClin Ed, FANZCA,†‡ and Michael J. Barrington, PhD, MBBS, FANZCA*§ Abstract: Existing literature on learning in regional anesthesia broadly covers the rate of skill acquisition and the structure of educational programs. A complementary body of literature spanning psychology to medical education can be found describing skill acquisition in other fields. Concepts described in this literature have direct application to the teaching of regional anesthesia. This review introduces a selection of these complementary educational concepts, applying them to ultrasound-guided regional anesthesia skills education. Key educational concepts presented in this article can be divided into 3 sections, namely, how residents acquire manual skills, how tutors teach, and type of feedback. (Reg Anesth Pain Med 2014;39: 230–239) A regional anesthesia training program should produce confident anesthesiologists capable of safe, independent practice. Tutors and residents alike are challenged by the complexity of the skills that must be acquired with limited time and clinical exposure. This review discusses motor skills learning, a subset of the skills required for ultrasound-guided regional anesthesia (UGRA). An overview of evidence for teaching UGRA has recently been published.1 Regional anesthesia educational literature describes curricula,2 the use of simulation, and supervised practice to teach regional anesthesia.3 Documenting the volume of practice before residents are judged as competent is prevalent.4–7 How motor skills are learned and taught attracts less attention, yet the education literature effectively describes these concepts. The development of expertise has been studied in many domains,8 providing a knowledge base for planning teaching. For example, students acquire motor skills at variable rates and pass through distinct behavioral stages. Therefore, it is important to implement individual teaching strategies, such as preparatory teaching, task setting, assessment, and feedback. This review aims to summarize relevant educational theory and apply it to the teaching of UGRA. Studies of Learning in Regional Anesthesia Learning studies in neuraxial anesthesia have predominantly investigated procedural volumes required before residents From the *Department of Anaesthesia and Pain Medicine, St Vincent’s Hospital, Fitzroy; †Department of Anaesthesia and Perioperative Medicine, Monash Medical Centre; ‡Department of Anaesthesia and Perioperative Medicine, Monash University; and §Melbourne Medical School, Faculty of Medicine, Dentistry and Health Sciences, University of Melbourne, Melbourne, Victoria, Australia. Accepted for publication February 6, 2014. Address correspondence to: Reuben J. Slater, BSc (Hon), BMed, FANZCA, Department of Anaesthesia and Pain Medicine, St Vincent’s Hospital, Fitzroy, Victoria 3065, Australia (e‐mail: ben.slater2@svhm.org.au). The authors declare no conflict of interest. Copyright © 2014 by American Society of Regional Anesthesia and Pain Medicine ISSN: 1098-7339 DOI: 10.1097/AAP.0000000000000072 230 achieved competency. Studies by Kopacz et al,5 Konrad et al,9 and Kestin6 introduced learning curves and the use of cumulative summation analysis to skills acquisition. These studies defined competency differently, leading to variable results. Rosenblatt and Fishkind10 documented that, after 15 attempts, 87.5% of residents were able to place an interscalene brachial plexus block without intervention. A survey of senior anesthesia residents’ experience with nerve blocks confirmed that their exposure was insufficient for confident practice.11 Studies demonstrate that the experience required for a minimal level of competence may exceed opportunities available for many residents.11 Ultrasound-guided regional anesthesia involves complex motor skills and a broad knowledge base. Novices find key skills, such as optimizing sonographic images and recognizing sonographic anatomy, challenging. Despite this, Orebaugh et al12 demonstrated that residents performed UGRA more efficiently than nerve stimulator-guided techniques with a success rate of 97% using UGRA. As residents became more experienced, procedural time decreased as their ability to efficiently identify neural structures improved. Several studies examine how long-axis needle-imaging skills are acquired. Using a turkey breast/olive model, Sites et al13 measured a significant improvement in resident performance during 6 trials when feedback was given after each trial. de Oliveira Filho et al14 used a meat phantom and applied a discovery learning model, believing it represented how most individuals learn. Individuals varied in their rate of skill acquisition, with 30% of participants attaining proficiency. A mathematical model suggested that to achieve a 95% success for long-axis needleimaging skills or placing the needle tip next to a target, 37 or 109 attempts would be required, respectively. Barrington et al15 used a cadaver training model of in-plane sciatic nerve blockade. Resident performance was assessed evaluating long-axis needle visualization and probe steadiness. Residents performed 30 simulated blocks with feedback after each attempt. Consistent with de Oliveira Filho et al, residents varied significantly in their rate of skill acquisition; however, their results suggested that competency in needle placement would be achieved in 28 trials. These differing results with different teaching paradigms (discovery-learning vs feedback) indicate the potential value that feedback can have on acquiring skills. More broadly, this implies that teaching strategies can optimize motor skill learning and tutors should consider incorporating these into training programs. Equipment for UGRA is constantly changing; visualizing needles has become easier as hardware, software, and the needles themselves improve. With technological advances, some of the previously mentioned studies may be obsolete. Teachers and residents must remain abreast of the latest advances and adjust their skill sets appropriately. The studies mentioned in this section have been summarized in Table 1. How Are Motor Skills Learned? Educational literature describes the development of motor skills across many domains; principles are generic rather Regional Anesthesia and Pain Medicine • Volume 39, Number 3, May-June 2014 Copyright © 2014 American Society of Regional Anesthesia and Pain Medicine. Unauthorized reproduction of this article is prohibited. Regional Anesthesia and Pain Medicine • Volume 39, Number 3, May-June 2014 Motor Skills in Regional Anesthesia TABLE 1. A Summary of the Papers Mentioned in “Studies of Learning in Regional Anesthesia” Author Kopacz et al Procedure(s) 5 Konrad et al9 Kestin6 Rosenblatt and Fishkind10 Orebaugh et al12 Spinal, epidural, intubation Subjects 7 first-year residents Methodology Objective measures of success used for a range of procedures over 6 months of training Measured success or failure of a range of procedures over a year Spinal, epidural, 11 first-year residents brachial plexus block, intubation, arterial line insertion Obstetric epidural, Junior residents in a CUSUM analysis charting spinal, central venous department over a year success or failure of catheter and arterial 4 techniques line Insertion Interscalene block, All first- and second-year Reporting of experience during nerve stimulator residents in a department an 8-mo period, utilising level over 8 months of supervision and success Interscalene 222 consecutive blocks by Total block time, imaging time, block, UGRA practitioners with a range and time for needle insertion of experience measured for each block Outcome 45 and 60 attempts at spinal and epidural anesthesia, respectively, were required to achieve a 90% success rate Epidural anesthesia was the most difficult procedure to perform. CUSUM is a useful technique to monitor training of practical procedures. Number of blocks required to reach proficiency was greater than previously thought. 97.3% success rate. Time to perform block and acquire image decreased over 4 wk. Time to insert needle did not change Residents can rapidly improve performance using a simulated task. Failure to visualize needle most common error. 37 to 109 attempts were required to achieve proficiency, significant variation between subjects. Sites et al13 Simulated UGRA 10 residents between first and third year Simulated tasks, videotaped and assessed for speed and accuracy de Oliveira Filho et al14 Simulated UGRA (bovine phantom) 30 anesthesiologists or residents who had no experience with ultrasound Discovery learning paradigm. 25 consecutive trials of needle insertion and then needle insertion to a target. Analysis using CUSUM and Bush and Mosteller’s learning model Feedback offered after each Significant variation in trial. Procedures video-taped proficiency, 28 simulated and scored blind. CUSUM and blocks to become proficient. Bush and Mosteller’s learning model used for analysis. 15 residents who had Barrington et al15 Simulated UGRA (cadaver, sciatic Nn) performed < 5 UGRA procedures CUSUM indicates cumulative sum control chart analysis; UGRA, ultrasound guided regional anesthesia. than specific and provide insight into teaching motor skills in UGRA. The Power Law of Learning Performance improves with practice and is described by a robust relationship16 valid across domains including sport, chess, and music.8 Initial practice leads to a rapid development. As practice continues, the improvement demonstrated for a quantum of practice decreases so learning curves display a logarithmic shape, explaining “The power law of learning.” Improving performance can be demonstrated after thousands of hours of practice. Crossman17 documented individual improvement in cigar rolling after 10 years of practice and 100,000,000 cigars. Learning curves have been published for a wide range of anesthesia procedures, including arterial line insertion, intubation, brachial plexus, and neuraxial blockade.5,9 Behavioral Stages of Motor Learning Ultrasound-guided regional anesthesia skills are associated with clinical decisions, patient care, and working in a team. Cognitive load theory describes how information can overload our cognitive capacity. The theoretical cognitive space that is © 2014 American Society of Regional Anesthesia and Pain Medicine used to attend to sensory information and solve problems is labeled attentional capacity.51 Schema18 are organized patterns of thought or behavior used to minimize cognitive load. When examining motor skills, they can be considered “motor programs.” Motor skills learning can be conceptualized as the creation of schema. Schema theory states that prepackaged sequences of actions are stored in procedural memory and the desired outcome is represented and stored in recognition memory. When the schema is executed, the result is compared with the desired outcome; learning occurs through adjustment of both recall and recognition memory. Dreyfuss,19 Rassmussen,20 Fitts and Posner,21 and Anderson16 have described learner behaviors as they acquire new motor skills. Learners typically pass through stages that are not discrete but characterize approximate points in the “qualitative evolution of a skill.”16 These models are summarized in Table 2. In this review, the work of Fitts and Posner21 later adapted by Anderson,16 is emphasized because this model has behavioral correlates in both learning anesthesia and cognitive neuroscience (Table 3). The Early (or Cognitive) Stage Residents need a concept of a new motor skill. This concept may be based on didactic instruction, observation, or previous 231 Copyright © 2014 American Society of Regional Anesthesia and Pain Medicine. Unauthorized reproduction of this article is prohibited. Regional Anesthesia and Pain Medicine • Volume 39, Number 3, May-June 2014 Slater et al TABLE 2. Four Models Describing Stages of Motor Skill Acquisition Author and References Stages Summary Adams L. (describing Noel Burch, 1970 Gordon Training International19) 1. 2. 3. 4. 1. 2. 3. 4. 5. 1. 2. 3. Widely quoted in management courses and education courses. Does not appear in the peer-reviewed literature with regularity. Dreyfuss,48 1980 Rasmussen (for more detail, refer to review by Long52 or Rasmussen’s original description.29) Fitts and Posner21/Anderson16 Unconsciously unskilled Consciously unskilled Consciously skilled Unconsciously skilled Novice Competence Proficiency Expertise Mastery Skill based Rule based Knowledge based 1. Early (cognitive) 2. Intermediate (associative) 3. Final (autonomous) experience. In the cognitive stage, attempts at the skill are problem-solving exercises creating movements that match their concept of the skill. Problem solving may fully occupy their In Dreyfuss’ model, a novice rigidly follows rules. As he progresses through the stages, he starts to use rules in context. Finally, new rules are intuitively developed and enacted. Devised to describe situations in which rapid decisions have to be made. First, skills are attained; then as knowledge is increased, the learner gains the ability to use these skills appropriately. Finally, the learner develops a required solution from broad-based knowledge. The model described by Fitts and Posner and later Anderson is described in detail in Table 3 and also in the text of this review. attentional capacity, a limited cognitive space. In the early behavioral stage, residents seem indecisive and error prone with a complete focus on the task and lack of situational awareness.16 TABLE 3. Description of a Resident Performing Brachial Plexus Block and Corresponding Behavioral and Neuropsychological Correlates of the Motor Skill Stages Described by Fitts and Posner and Later by Anderson Stage Early (cognitive) Intermediate (associative) Final (autonomous) 232 Behaviors50 Description In this stage, a resident attempting an axillary brachial plexus block struggles to set up the environment, his biomechanics are poor, and he checks and rechecks landmarks. All movements lack conviction. The resident does not know whether to look at patient or ultrasound screen. Despite this indecision he is completely focused on the task at hand and unaware of what is occurring in the procedure room. He does not interact with the care team or patient. When attempting long-axis needle placement, the needle is poorly visualized, the resident makes seemingly random movements and often the needle and probe are moved simultaneously to improve the view. In this stage, there is more structure to the resident’s performance. The resident is more likely to position herself correctly and optimize the ultrasound image. The resident’s movements are more concise and seem planned. When performing long-axis needle placement, she may hold the probe steady with relatively good control and interact with the patient and other members of the care team while performing the block. If the task becomes challenging or the environment becomes more stressful, the resident reverts to a problem-solving mode, and her behavior reflects the cognitive stage. The resident now performs the block with ease. Movements are precise, efficient, and inspire confidence. The resident can comfort the patient and interact with the care team while performing the block. He is not disrupted by unexpected events, and if the block becomes complex, he has developed strategies to deal with problems encountered. Neuroimaging16 • Inaccurate • Inconsistent • Inefficient • Slow, halting • Timid • Rigid • Many errors • Lateral prefrontal area (general planning) • More relaxed • More consistent • More efficient • More adaptable • More confident • Fewer errors • Supplemental motor area (guidance of action) • Posterior parietal cortex (motor planning) • Hippocampus (retrieval of memory) • Automatic • Consistent • Accurate • Adaptable • Fluid • Recognizes errors © 2014 American Society of Regional Anesthesia and Pain Medicine Copyright © 2014 American Society of Regional Anesthesia and Pain Medicine. Unauthorized reproduction of this article is prohibited. Regional Anesthesia and Pain Medicine • Volume 39, Number 3, May-June 2014 Residents in this stage may have an internal monologue, reminding themselves of the required sequence of events or mistakes they have previously made.22 During the cognitive stage, motor behaviors that lead to success are reinforced and those that lead to failure are extinguished. Eventually, a solution to the motor problem is generated in the form of a schema. The neurologic correlate of this stage is neural activity concentrated in the prefrontal and parietal regions. As motor skills improve, this activity decreases, whereas activity in the supplemental motor area and hippocampus increases.16,23 The Intermediate (or Associative) Stage The resident in the associative stage has developed a schema, which has 2 consequences. First, the resident’s movements become more fluid and definite; they seem relaxed and make fewer mistakes. Second, their use of attentional capacity has decreased so that they can effectively interact with their environment, which allows their situational awareness and nontechnical skills to improve. At this stage, a resident might be confronted with more challenging cases and opportunities for independent practice.9 These scenarios place pressure on the resident’s nascent motor plan, and they may revert to a problem-solving approach exhibiting cognitive stage behaviors. The Final (or Autonomous) Stage The resident in this stage has automatic, accurate, fluid, and consistent movements. Residents easily recognize mistakes, adapt to unexpected situations, and make errors infrequently; little cognitive input is required to perform the task, leaving attentional capacity available to concentrate on other issues. In anesthesia, this may be reflected by a superior ability to communicate with and monitor the patient and interact with other members of the care team. Expert Performance Ericsson has written extensively about expert performance, how expertise is defined and how individuals achieve it. Expertise is characterized by superior and reproducible performance across many domains. Experts in chess win more often and expert musicians play more complex pieces making fewer mistakes. Expert medical practitioners consistently perform at a higher level than their peers.8 However, success alone may not be the best metric to define expertise. For example, the high success rate reported by Orebaugh et al24 potentially reflects how closely residents were supervised rather than their learning or expertise. In surgical studies, time and error metrics distinguish novices from experts but more complex metrics are required to distinguish between advanced beginners and experts.25 Advanced metrics include measures of kinematics, such as the imperial hospital surgical assessment tool,26 or the ability to multitask while performing a skill. Smith et al27 suggest expertise goes beyond technical proficiency and is determined by maximizing patient comfort, anticipating problems, communicating well, and recognizing the limits of safe practice. These attributes are consistent with the autonomous stage and directing attentional capacity to nontechnical skills.28 Application of Educational Expertise to Teaching UGRA Skills At the end of anesthesia training, residents should be not only capable of high procedural success rates under supervision © 2014 American Society of Regional Anesthesia and Pain Medicine Motor Skills in Regional Anesthesia but also proficient, safe, and confident in independent practice, capable of self-assessment, and managing their ongoing professional development. To do this, we need to do more than provide experience. How can we teach procedures more effectively? Specific teaching strategies based on what we know of how motor skills develop may improve learning. Preparatory Teaching A learner performing a motor skill for the first time must have a concept of the desired outcome; their goal is to craft a series of movements into a schema to fit this outcome. This concept can be informed by didactic teaching, reading references, watching videos, or observing clinical practice. Surgical residents have successfully learned knot tying using a computer-aided video package.29 Learning by observing may be an underused resource in medical skills education.30 Observing senior colleagues in everyday practice may have a powerful influence on residents’ practice.31 Even when an anesthesiologist is not actively teaching, observant residents may be learning by example, so that, as “exemplars of performance,” what we do may be more important than what we teach.31 Task Deconstruction Experts perform procedures automatically; hence, a motor task may be “easier done than said.”32 In contrast, novices require discrete steps and explicit direction. Cognitive task analysis tools break down complex skills into individual processes and decisions to facilitate teaching.33 In anesthesia, task analysis tools have been used to examine the individual tasks involved in procedures including axillary brachial plexus blockade34 and central line insertion.35,36 Simulated Practice Individual tasks and processes can be practiced in a laboratory environment. Practicing individual components of motor skills is known as part-task training37 or fractionization.46 Adding steps of a motor program together sequentially until eventually the whole task is performed is described as segmentation.38 Tasks and processes may be sequential or occur in parallel. Motor skills occurring in parallel are not suitable for fractionation. Integral to long-axis needle visualization is the specific interaction between the ultrasound transducer and needle which cannot be replicated unless the components are practiced together.38 Temporal separation of simulated training sessions is important. A resident undertaking a task 10 times in 1 session (massed practice) may not learn as much compared with attending 5 sessions with 2 trials each (blocked practice). The benefit of blocked practice is related to the requirement for the “motor problem” to be partially resolved.39 However, enhanced learning in the massed practice setting can be achieved by teaching a number of skills in a random order, thus disrupting the resident’s flow and challenging them on each task.40,41 A “pre-trained novice”49 can be created by maximizing procedural learning in simulated environments, with the learner developing some automaticity and spare attentional capacity before their clinical practice commences. Supervised Practice A teacher should choose the appropriate level of performance for a resident, by assessing the prior knowledge and level of proficiency.21 Options for varying the difficulty of skill 233 Copyright © 2014 American Society of Regional Anesthesia and Pain Medicine. Unauthorized reproduction of this article is prohibited. Regional Anesthesia and Pain Medicine • Volume 39, Number 3, May-June 2014 Slater et al FIGURE 1. Learning and teaching concepts presented in this article, related to the learning stages described by Fitts and Posner.21 performance include practicing only part of the procedure, varying the support provided, or allowing the resident to perform only straightforward cases. According to Vygotsky, tasks can be conceptualized as within a resident’s independent capability, beyond their capability, or within their zone of proximal development (ZPD), where TABLE 4. A Summary of Concepts Derived From Education Literature With Relevance to Teaching in Regional Anesthesia Description Power law of learning 17 Deliberate practice8 Attentional capacity50 Application Performance improves with practice. Initially performance improves rapidly, however, with ongoing practice, performance improvements decrease. Practice continues to have small benefits even in very experienced practitioners. Teacher assesses performance, identifies problems, and targets practice to eliminate problems. A cognitive space with limited capacity used to focus on a specific aspect of the environment. Stages of motor skill learning 21 Three behavioral stages, which can be identified as a resident acquires a motor skill. Expertise8 Performing at a level that is consistently superior to your peer group. Systematic Training and Assessment of Technical Skills (STATS framework)32 A systematic training and assessment tool for motor skills comprising (1) knowledge based learning, (2) task deconstruction, (3) training in laboratory environment, (4) transfer of skills to the clinical environment, and (5) obtaining privileges for independent practice. Resident’s performance will improve rapidly with practice. After ongoing practice, the rate of improvement in performance is less; however, quality practice will always lead to some performance improvement. Practice does not necessarily lead to performance improvement, high-quality practice is required. Residents attempting a skill for the first time will focus their attention on the skill. As attentional capacity is limited, he will have a limited ability to focus on other areas of the clinical environment. The behaviors exhibited by a resident can be used to assess her level of motor skill learning. Training can then be set appropriately. Performing at the highest level. Practitioners who are experts are likely to have had thousands of hours of experience and have engaged in deliberate practice. A way of structuring a training program for aspects of a curriculum that require motor skills. Can be used granting privileges for independent practice. Continued next page 234 © 2014 American Society of Regional Anesthesia and Pain Medicine Copyright © 2014 American Society of Regional Anesthesia and Pain Medicine. Unauthorized reproduction of this article is prohibited. Regional Anesthesia and Pain Medicine • Volume 39, Number 3, May-June 2014 Motor Skills in Regional Anesthesia TABLE 4. (Continued) Description 33,36 Cognitive Task Analysis A method of breaking down a motor skill that has become automated into sections that can be taught effectively. Self-directed learning45 Residents who can independently set appropriate academic goals and design strategies to achieve their academic goals. Learning and performance51 Performance of a motor skill is a measure of immediate aptitude. If a learning session leads to a sustained improvement in performance when the skill is tested after a delay, learning has occurred. A person performing a motor skill while being observed by a resident. Can be live or via digital media. Exemplar of performance45 Zone of Proximal Development (ZPD)42 Scaffolding42 Challenge point43 Fractionation38 Segmentation38 Massed practice39 When a resident performs a task that is difficult enough that they require help from a tutor, it is described as being in the ZPD. Tasks performed in the ZPD promote learning. A term used to describe the support given to a resident, when they are performing a task in the ZPD. There is an optimal level of difficulty for any motor task given to an individual resident. Tasks that are too easy or too difficult do not promote learning. Practicing discrete components of a motor skill. Adding discrete components of a motor skill together after they have been practiced separately. Practicing a motor skill repetitively at a single session. Blocked practice39 Practicing a motor skill at several discrete sessions. Pretrained novice49 A resident who has practiced a skill in a nonclinical environment. When they transfer the skill to the clinical environment they have more attentional capacity. Feedback45 Feedback can be internal, a resident critiquing their own performance or external, a tutor providing information about a resident’s performance. Briefing can be used before a learning interaction to assess a resident’s knowledge and define appropriate goals and limits. Debriefing or delivering feedback can then refer directly to the goals set. Brief/debrief46,47 Application For an exemplar of performance, a skill may be “easier done than said.” Cognitive task analysis provides a method to break down motor skills into steps so steps can be taught individually. Self-directed learners tend to perform better academically. They tend to be internally motivated to learn and practice. This is in comparison to externally motivated residents, who are driven by desire to please or to pass examinations. Improvement in a measurable aspect of a resident’s performance during a teaching session does not necessarily reflect learning. For learning to occur the improvement must persist or be transferrable to other skills. As a qualified anesthesiologist, whenever you perform a manual skill you are acting as a role model to residents who may be watching. What you do is profoundly more important than what you teach. The difficulty of a task should be modulated to be appropriately challenging for the resident. The type of support given to a resident can vary from guidance through stages of a task, to control of clinical environment. Another way of describing the concept of ZPD, tasks administered to residents need to be appropriately challenging to promote resident. A component of a motor task is practiced in isolation. For example, ultrasound scanning to identify neural structures is practiced in a laboratory. Components of a motor skill that have been practiced separately are linked together. Repetitively practicing the same motor skill at a single setting may improve performance, but not lead to learning. Practicing motor skills in discrete blocks requires the motor skill to be resolved at each setting. This may improve learning. Residents who have progressed beyond the first stage of motor skills acquisition in simulated practice, will have more attentional capacity to apply to other aspects of the clinical environment and nontechnical skills. Learning cannot occur without feedback. Feedback should be balanced and limited. Before setting a task, have a discussion that assesses a resident’s knowledge and level of performance. Set a task of the appropriate difficulty. Discuss responsibility for different aspects of the clinical environment and limits at which you will take over the task. This discussion then forms a framework for feedback at end of procedure. Continued next page © 2014 American Society of Regional Anesthesia and Pain Medicine 235 Copyright © 2014 American Society of Regional Anesthesia and Pain Medicine. Unauthorized reproduction of this article is prohibited. Regional Anesthesia and Pain Medicine • Volume 39, Number 3, May-June 2014 Slater et al TABLE 4. (Continued) Description Dialogue of feedback 45 Application Feedback in the form of a discussion may improve the learning experience, by elucidating the resident’s internal feedback processes before giving external feedback. Concurrent feedback45 Feedback delivered during the performance of a skill. Summary feedback45 Feedback performed at the end of a motor skill. they can complete the task only with support.42 Performing tasks in the ZPD allows development of skills. Guadagnoli and Lee43 describe a challenge point framework, suggesting that there is an optimal difficulty that will promote learning. Bjork and Bjork44 describe the concept of “desirable difficulty,” suggesting that a degree of challenge will enhance learning. A task allocated to a resident should be complex enough that they can learn, without being so complex that it is impossible to achieve. In clinical settings, a tutor can assume control of the procedure and environment so as to allow the resident to concentrate on a specific skill. This has been described as “scaffolding.”44 During regional anesthesia, environmental control includes attending to patient comfort, monitoring sedation and physiological parameters, or interacting with members of the care team. As residents become more experienced, they take on more of these responsibilities moving toward independent practice. This process of environmental control should be disclosed to the resident, so they are aware of the process and not lulled into a false sense of security. Systematic Training and Assessment of Technical Skills Framework A framework for the systematic training and assessment of technical skills (STATS) has been developed by Aggarwal et al.32 This provides a template for curriculum development in procedural teaching. The training program in regional anesthesia at the Mayo Clinic described by Smith et al2 demonstrates how the STATS framework can be applied to teaching UGRA. Initiating feedback by asking an open question, “How do you think you performed?” Gives the tutor a concept of the resident’s internal model of the skill and their internal feedback processes. May encourage feedback about the teaching session. May be useful for novices performing procedures with multiple steps, allowing the novice to concentrate on a motor skill without having to concentrate on the overall sequence. In more experienced residents concurrent feedback may inhibit learning. Feedback provided at the end of a procedure. Feedback Feedback is an important tool that allows a resident to close the gap between their current and desired performance during all stages of skill acquisition. A model describing the interaction of the resident and task, developed by Nicol and MacFarlane-Dick,45 provides an opportunity for a deeper understanding of feedback. The model has been modified herein (Fig. 1) to apply to motor skills learning. There are 2 distinct feedback pathways available when a resident undertakes a motor skill (Fig. 1). First, the resident compares their performance to a mental concept of how the skill should be performed (internal feedback). Second, an external source provides information on the resident’s performance (external feedback). Before a resident performs a supervised skill, there should be a discussion about goals to establish agreed expectations. These goals define control of the clinical environment, set limits on skill performance and, importantly, frame postprocedure feedback. This concept mirrors the “briefing/ debriefing” model that is used extensively in the military, emergency services, and aviation.46,47 Feedback may most simply be initiated by asking the resident how they viewed their performance. This allows the tutor not only to assess the resident’s attempt at the skill but also the resident’s desired level of performance.45 External feedback can be used to correct both what was observed during the procedure and also the resident’s internal model. Targeted feedback is critical as the capacity to accept and use feedback is limited. Feedback does more than correct technical points. Poor performance may point to a lack of motivation if the resident FIGURE 2. Illustrating the concept of internal and external feedback loops, modified from Nicol and Macfarlane-Dick.45 236 © 2014 American Society of Regional Anesthesia and Pain Medicine Copyright © 2014 American Society of Regional Anesthesia and Pain Medicine. Unauthorized reproduction of this article is prohibited. Regional Anesthesia and Pain Medicine • Volume 39, Number 3, May-June 2014 Motor Skills in Regional Anesthesia FIGURE 3. This framework draws on the concepts in the review to describe an “ideal” learning scenario. The framework could be used in preclinical environments to create the pretrained novice, or in clinical environments. does not appreciate the value of the skill or of performing it as the tutor requires. Feedback can be used to discuss why the skill is valuable or how the outcome may be improved if it is performed in a given way. A knowledge deficit may be identified in the discussion and the tutor might be able to assist the resident with advice about learning resources. During feedback, a tutor will ideally have made 2 or 3 points that may include constructive criticism, identification of weaknesses, problem solving, and positive reinforcement of the resident’s technique. The dialogue may conclude with feedback of how effective the teaching session has been for the resident. The timing of feedback is important; it should be given as close as possible to the end of skill performance (summary feedback). There is a risk if feedback is delivered constantly throughout performance (concurrent feedback) that the resident will depend on this feedback with inhibition of learning. Concurrent feedback may be required with new skills or to prevent harm to patients. Summary This review highlights the importance of teaching in the acquisition of motor skills, a subset of the total skill base required to practice UGRA. To do this, we have reviewed the literature from the psychology and education domains. Table 4 provides a summary of concepts and Figure 2 relates the concepts to the stages of learning motor skills. Applying lessons from other academic domains allows anesthesiologists to pass on their © 2014 American Society of Regional Anesthesia and Pain Medicine knowledge more effectively, with the goal of producing confident, safe, and knowledgeable residents, capable of independent practice. Residents should prepare themselves before attempting new motor skills, and this should include creating a mental concept of how the skill is performed. Observing senior colleagues is important and even when teachers are not actively teaching they act as role models. Pretrained novices can be created through preclinical training or simulations with clinical benefits. Within the clinical environment, teachers can modulate task difficulty to optimize learning. Structuring learning encounters with briefing and debriefing can be used to establish agreed goals and frame a feedback dialogue restricted to 2 to 3 balanced points. Incorporating teaching strategies, which have been developed to maximize learning of motor skills, into regional anesthesia training programs provides the opportunity to improve the quality and efficiency of learning opportunities. The UGRA training program at the Mayo Clinic2 provides an excellent framework for a UGRA teaching program. To conclude this review, we present an ideal framework for a single teaching session in Figure 3. This session could be in a simulator as part of the training of a pretrained novice or supervised practice in a clinical environment. ACKNOWLEDGMENT The authors thank Assistant Professor Lisa Warren (Department of Anesthesia, Critical Care and Pain Medicine at Massachusetts General Hospital), who made insightful comments on several drafts of this review. 237 Copyright © 2014 American Society of Regional Anesthesia and Pain Medicine. Unauthorized reproduction of this article is prohibited. Regional Anesthesia and Pain Medicine • Volume 39, Number 3, May-June 2014 Slater et al REFERENCES 1. Nix CM, Margarido CB, Awad IT, et al. A scoping review of the evidence for teaching ultrasound-guided regional anesthesia. Reg Anesth Pain Med. 2013;38:471–480. 2. Smith HM, Kopp SL, Jacob AK, Torsher LC, Hebl JR. Designing and implementing a comprehensive learner-centred regional anesthesia curriculum. Reg Anesth Pain Med. 2009;34:88–94. 3. Castanelli DJ. The rise of simulation in technical skills teaching and the implications for training novices in anesthesia. Anaesth Intensive Care. 2009;37:903–910. 4. Regional Anesthesiology and Acute Pain Medicine Fellowship Directors Group. Guidelines for fellowship training in regional anesthesiology and acute pain medicine: second edition, 2010. Reg Anesth Pain Med. 2011;36:282–288. 5. Kopacz DJ, Neal JM, Pollock JE. The regional anesthesia “learning curve.” What is the minimum number of epidural and spinal blocks to reach consistency? Reg Anesth. 1996;21:182–190. 6. Kestin IG. A statistical approach to measuring the competence of anaesthetic trainees at practical procedures. Br J Anaesth. 1995;75:805–809. 7. Naik VN, Devito I, Halpern SH. Cusum analysis is a useful tool to assess resident proficiency at insertion of labour epidurals. Can J Anaesth. 2003;50:694–698. 8. Ericsson KA. Deliberate practice and the acquisition and maintenance of expert performance in medicine and related domains. Acad Med. 2003;79:S70–S81. 9. Konrad C, Schupfer G, Wietlisbach M, Gerber H. Learning skills in anesthesiology: is there a recommended number of cases for anesthetic procedures? Anesth Analg. 1998;86:635–639. 21. Fitts PI, Posner MI. Learning and skilled performance. In: Fitts PI, Posner MI, eds. Human Performance. London: Prentice/Hall, Inc; 1973:8–25. 22. Adams JA. A closed loop theory of motor learning. J Mot Behav. 1971;3:111–149. 23. Luft AR, Buitrago MM. Stages of motor skill learning. Mol Neurobiol. 2005;32:205–216. 24. Orebaugh SL, Williams BA, Kentor ML, Bolland MA, Mosier SK, Nowak TP. Interscalene block using ultrasound guidance: impact of experience on resident performance. Acta Anaesthesiol Scand. 2009;53:1268–1274. 25. Stefanidis D, Scerbo MW, Korndorffer JR Jr, Scott DJ. Redefining simulator proficiency using automaticity theory. Am J Surg. 2007;193:502–506. 26. Chin KJ, Tse C, Chan V, Tan JS, Lupu CM, Hayter M. Hand motion analysis using the imperial college surgical assessment device: validation of a novel and objective performance measure in ultrasound-guided peripheral nerve blockade. Reg Anesth Pain Med. 2011;36:213–219. 27. Smith AF, Pope C, Goodwin D, Mort M. What defines expertise in regional anaesthesia? An observational analysis of practice. Br J Anaesth. 2006;97:401–407. 28. Fletcher GCL, McGeorge P, Flin RH, Glavin RJ, Maran NJ. The role of non-technical skills in anaesthesia: a review of current literature. Br J Anaesth. 2002;88:418–429. 29. Xeroulis GJ, Park J, Moulton CA, Reznick RK, Leblanc V, Dubrowski A. Teaching suturing and knot-tying skills to medical students: a randomized controlled study comparing computer-based video instruction and (concurrent and summary) expert feedback. Surgery. 2007;141:442–429. 10. Rosenblatt MA, Fishkind D. Proficiency in interscalene anesthesia—how many blocks are necessary? J Clin Anesth. 2003;15:285–288. 30. Wulf G, Shea C, Lewthwaite R. Motor skill learning and performance: a review of influential factors. Med Educ. 2010;44:75–84. 11. Chelly JE, Greger J, Gebbhard R, Hagberg CA, Al-Samsam T, Khan A. Training of residents in peripheral nerve blocks during anesthesiology residency. J Clin Anesth. 2002;14:584–588. 31. The Doctor as Teacher—archived policy document. 1999. Available at http://www.gmc-uk.org/education/postgraduate/doctor_as_teacher.asp. Accessed February 29, 2012. 12. Orebaugh SL, Williams BA, Kentor ML. Ultrasound guidance with nerve stimulation reduces the time necessary for resident peripheral nerve blockade. Reg Anesth Pain Med. 2007;32:448–454. 32. Aggarwal R, Grantcharov TP, Darzi A. Framework for systematic training and assessment of technical skills. J Am Coll Surg. 2007;204:697–705. 13. Sites BD, Gallagher JD, Cravero J, Lundberg J, Blike G. The learning curve associated with a simulated ultrasound-guided interventional task by inexperienced anesthesia residents. Reg Anesth Pain Med. 2004;29:544–548. 33. Clark RE, Estes F. Cognitive task analysis. Int J Educ Res. 1996;25:403–417. 14. de Oliveira Filho GR, Helayel PE, da Conceicao DB, Garzel IS, Pavei P, Ceccon MS. Learning curves and mathematical models for interventional ultrasound basic skills. Anesth Analg. 2008;106:568–573. 15. Barrington MJ, Wong DM, Slater B, Ivanusic JJ, Ovens M. Ultrasound-guided regional anesthesia: how much practice do novices require before achieving competency in ultrasound needle visualization using a cadaver model. Reg Anesth Pain Med. 2012;37:334–339. 16. Anderson JR. Skill acquisition. In: Anderson JR, ed. Learning and Memory. 2nd ed. Hoboken, NJ: John Wiley & Sons Inc; 2000. 17. Crossman ERFW. A theory of the acquisition of speed skill. Ergonomics. 1959;2:153–166. 18. Schmidt RA. A schema theory of discrete motor skill learning. Psych Rev. 1975;82:225–260. 19. Adams L. Gordon Training International: Learning a new skill is easier said than done. 2011. Available at: http://www.gordontraining.com/ free-workplace-articles/learning-a-new-skill-is-easier-said-than-done/. Accessed September 5, 2013. 20. Rasmussen J. Skills, rules, knowledge: signals, signs and symbols and other distinctions in human performance models. IEEE Trans Syst Man Cybern B Cybern. 1983;123:257–266. 238 34. O’Sullivan O, Aboulafia A, Iohom G, O’Donnell BD, Shorten GD. Proactive error analysis of ultrasound-guided axillary brachial plexus block performance. Reg Anesth Pain Med. 2011;36:502–507. 35. Sullivan ME, Ortega A, Wasserberg N, Kaufman H, Nyquist J, Clark R. Assessing the teaching of procedural skills: can cognitive task analysis add to our traditional teaching methods? Am J Surg. 2008;195:20–23. 36. Velmahos GC, Toutouzas KG, Sillin LF, et al. Cognitive task analysis for teaching technical skills in an inanimate surgical skills laboratory. Am J Surg. 2004;187:114–119. 37. Wightman DC, Lintern G. Part-task training for tracking and manual control. Hum Factors. 1985;27:267–283. 38. Schmidt RA, Wrisberg CA. Supplementing the learning experience. In: Schmidt RA, Wrisberg CA, eds. Motor Learning and Performance. 4th ed. Champaign, IL: Human Kinetics; 2008:218–253. 39. Moulton CA, Dubrowski A, Macrae H, Graham B, Grober E, Reznick R. Teaching surgical skills: what kind of practice makes perfect?: a randomized, controlled trial. Ann Surg. 2006;244:400–409. 40. Shea JB, Morgan RL. Contextual interference effects on the acquisition, retention, and transfer of a motor skill. J Exp Psychol Learn Mem. 1979;5:179–187. © 2014 American Society of Regional Anesthesia and Pain Medicine Copyright © 2014 American Society of Regional Anesthesia and Pain Medicine. Unauthorized reproduction of this article is prohibited. Regional Anesthesia and Pain Medicine • Volume 39, Number 3, May-June 2014 41. Rendell MA, Masters RS, Farrow D, Morris T. An implicit basis for the retention benefits of random practice. J Mot Behav. 2011;43:1–13. 42. Verenikina I. Scaffolding and learning: its role in nurturing new learners. In: Kell P, Vialle W, Konza D, Vogl G, eds. Learning and the Learner: Exploring Learning for New Times. Wollongong, NSW, Australia: University of Wollongong; 2008:161–180. 43. Guadagnoli MA, Lee TD. Challenge point: a framework for conceptualizing the effects of various practice conditions in motor learning. J Mot Behav. 2004;36:212–224. 44. Bjork EL, Bjork RA. Making things hard on yourself, but in a good way: creating desirable difficulties to enhance learning. In: Gernsbacher MA, Pew, RWHough LM, Pomerantz JR, eds. Psychology and the Real World: Essays Illustrating Fundamental Contributions to Society. New York, NY: Worth Publishers; 2011:56–64. 45. Nicol DJ, Macfarlane-Dick. Formative assessment and self-regulated learning: a model and seven principles of good feedback practice. Stud High Ed. 2006;31:199–218. 46. Roberts NK, Williams RG, Kim MJ, Dunnington GL. The briefing, intraoperative teaching, debriefing model for teaching in the operating room. J Am Coll Surg. 2009;208:299–303. © 2014 American Society of Regional Anesthesia and Pain Medicine Motor Skills in Regional Anesthesia 47. Papaspyros SC, Javangula KC, Adluri RK, O’Regan DJ. Briefing and debriefing in the cardiac operating room. Analysis of impact on theatre team attitude and patient safety. Interact Cardiovasc Thorac Surg. 2010;10:43–47. 48. A five-stage model of the mental activities involved in directed skill acquisition. Berkeley Operations Research Center, 1980. Available at http://www.dtic.mil/dtic/index.html. Accessed September 5, 2013. 49. Gallagher AG, Ritter EM, Champion H, et al. Virtual reality simulation for the operating room: proficiency-based training as a paradigm shift in surgical skills training. Ann Surg. 2005;241:364–372. 50. Schmidt RA, Wrisberg CA. Structuring the learning experience. In: Schmidt RA, Wrisberg CA, eds. Motor Learning and Performance. 4th ed. Champaign, IL: Human Kinetics; 2008:254–280. 51. Schmidt RA, Wrisberg CA. Preparing for the learning experience. In: Schmidt RA, Wrisberg CA, eds. Motor Learning and Performance. 4th ed. Champaign, IL: Human Kinetics; 2008:187–216. 52. Long DM. Competency-based residency training: the next advance in graduate medical education. Acad Med. 2000;75:1178–1183. 239 Copyright © 2014 American Society of Regional Anesthesia and Pain Medicine. Unauthorized reproduction of this article is prohibited.