Erythropoietin and erythropoiesis
advertisement

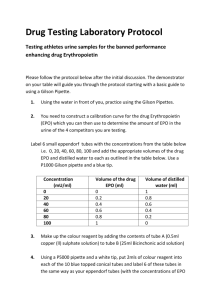
Experimental Hematology 2009;37:1007–1015 Erythropoietin and erythropoiesis Walter Fried Oncology Specialists, Park Ridge, Ill., USA (Received 20 April 2009; revised 20 May 2009; accepted 22 May 2009) Although the concept of a humoral regulator of erythropoiesis was introduced more than 100 years ago, its existence was first firmly established a little more than 50 years ago. This review briefly describes the historical development of information about erythropoietin. It then describes our current understanding of where erythropoietin is produced; the factors that regulate its rate of production; how erythropoietin acts at the cellular level to stimulate erythropoiesis; and its role in the regulation of the rate of erythropoiesis. Finally, it discusses the clinical uses of erythropoietin in the diagnosis and therapy of hematopoietic diseases. Ó 2009 ISEH - Society for Hematology and Stem Cells. Published by Elsevier Inc. In 1882, Dr. Bert and his colleagues [1] took their microscope high into the Mexican mountains and showed, for the first time, that the amount of red blood cells is increased when residing at a high altitude. They postulated that the rate of erythropoiesis is regulated by the oxygen supply to the site of red blood cell (RBC) production. This was the opening salvo in the quest to understand regulation of erythropoiesis. In 1906, when the concept of the humoral transmission of information from one site to a distant one via the bloodstream was new, two French scientists, Carnot and DeFlandre [2], postulated that the effect of hypoxia on erythropoiesis was mediated by a hormone, which they named haemopoietin. To test this hypothesis, they bled rabbits of 10 mL. Then they collected their plasma and injected 10 mL intravenously into normal rabbits. They claimed that this caused an increase in the recipient rabbits’ RBC count. These experiments were then, and are not now, reproducible. However, the possibility of a hormonal control of erythropoiesis was not rejected. In 1952, Drs. Grant and Root [3] reviewed the studies on regulation of erythropoiesis, including experiments that Dr. Grant performed using an oxygen-sensitive electrode that was implanted into the bone marrow of anemic animals. Despite the anemia, the bone marrow oxygen tension remained normal. They, therefore, concluded that the effect of hypoxia on erythropoiesis could not be exerted directly on the marrow. They considered a humoral mechanism to be likely. In 1950, Dr. Kurt Reissman [4] parabiosed rats. Offprint requests to: Walter Fried, M.D., Oncology Specialists, 1700 Luther Lane, Park Ridge, IL 60068; E-mail: fried_walt@hotmail.com He then subjected one parabiont to hypoxia, but showed that both rats became plethoric. He was able to document that only one of the parabionts became hypoxic, and also that there was capillary and small blood vessel communication between the parabionts that permitted transport of humoral factors between them. In 1953, Dr. Alan Erslev [5] provided the first direct and reproducible evidence for a humoral factor in the plasma of anemic rabbits that increased the reticulocyte count of normal rabbits injected with the anemic rabbit plasma. He bled rabbits of about 150 mL blood to reduce their hematocrits to about 20%. Then he collected their plasma and injected normal rabbits with 200 mL anemic rabbit plasma. He documented a significant increase in the reticulocyte counts of the normal recipient rabbits. This was essentially a repeat of the experiments of Carnot and DeFlandre [2], which were performed 50 years previously; however, with induction of much more severe anemia and injection of 20-fold more anemic plasma into the normal recipients. Also key to their success was the use of the reticulocyte count, which was not available to the earlier investigators, to assess erythropoiesis. The year 1953 was also an auspicious one for me. As a 4th-year premed student, I joined a classmate of mine, Louis Plzak, in the laboratory of Dr. Leon O. Jacobson. Dr. Jacobson was the Director of the Hematology Section at the University of Chicago and the Director of the Argonne Cancer Research Hospital (a hospital supported by the Atomic Energy Commission to study the role of radioactive isotopes in medicine). Dr. Jacobson was already a renowned scientist whose studies on shielding spleens of mice to protect their hematopoietic system from radiation 0301-472X/09 $–see front matter. Copyright Ó 2009 ISEH - Society for Hematology and Stem Cells. Published by Elsevier Inc. doi: 10.1016/j.exphem.2009.05.010 1008 W. Fried/ Experimental Hematology 2009;37:1007–1015 damage led to the first evidence of the existence of multipotential hematopoietic stem cells that are capable of regenerating the total hematopoietic system after radiation damage. Despite recognizing that the radioprotective effects of spleen-shielding were due primarily to sparing of hematopoietic stem cells that could travel from the spleen to repopulate sites in the marrow, Dr. Jacobson still had a suspicion that there was a humoral factor released by the shielded spleen that was instrumental in promoting regeneration of hematopoiesis. Therefore, Dr. Jacobson became very interested in the humoral factor that Dr. Erslev had identified. At that time, Louis Plzak and I were studying the uptake of radioactive iron into avian erythrocytes as a way of measuring erythropoiesis. Dr. Jacobson sensed the importance of using radioactive iron uptake into mammalian erythrocytes to develop a practical bioassay for the humoral factor that Dr. Erslev had reported. He asked Louis Plzak and I to work on developing such an assay. He suggested that we use rats as the test animals. In 1955, we [6] reported the development of a practical but still crude assay for detecting erythropoietin (EPO). By injecting 10 mL plasma from anemic rats into normal rats, we were able to demonstrate a significant effect on the rate of uptake of Fe59 into newly formed erythrocytes of the recipients. In the subsequent year, we were able to increase the sensitivity of the assay several fold by using animals that had a plethora of oxygen compared to their needs. The first such model was the hypophysectomized rat [7] that had a markedly reduced metabolic rate and therefore had more RBCs than needed for the first few weeks postoperatively. Next we used transfusion-induced plethoric rats. The concept was that in plethoric rats, EPO production and consequently the serum EPO titer should decrease to subnormal levels and then these animals would become very sensitive to exogenous EPO. In 1962, Dr. DeGowin et al. [8] described the posthypoxic mouse model. Mice were made plethoric in a chamber evacuated to one-half atmosphere. After 2 weeks, they were plethoric and very sensitive to exogenous EPO. Compared to the initial experiments that required 200 mL and then 10 mL anemic plasma, these posthypoxic mice could detect increased EPO titers in as little as 0.5 mL. Also, they could detect EPO in rabbit, rat, mouse, and human plasma. This bioassay became the standard for assaying EPO for 20 years until development of a reliable immunoassay. Using these newly available bioassays, we studied the effect of a variety of factors on erythropoietin production, including cobaltous chloride [9] and androgenic [10] and anabolic steroids. In 1956, we began to investigate the effect of removing various organs from rats on their ability to produce EPO in response to various stimuli. We failed to show any effect on EPO production of removing the various endocrine glands. Then our classmate, Sandy Krantz, suggested that we might consider the kidneys because patients with renal failure were always anemic and some with hypernephromas became plethoric. This called to mind a study by Stohlman et al. [11]. He was called to see a child who had a patent ductus that emptied into the aorta below a coarctation. Consequently, the child was pink above the diaphragm and blue below. Dr. Stohlman aspirated bone marrow from both the sternum and the iliac crest. Both sites had marked erythroid hyperplasia. The implication was that erythropoiesis is regulated by a humoral factor that originates from somewhere below the diaphragm. Our next study was to perform bilateral nephrectomies on one group of rats, ligate the ureters of another group, and perform a laparotomy only on a third group. Only the nephrectomized rats failed to produce a significant amount of EPO in response to anemia, injection of cobaltous chloride, or hypoxia. Results of some of these studies were first reported in 1957 [12] and provided the first direct evidence for the role of the kidney in the production of EPO. In 1977, Drs. Miyake and Goldwasser [13] succeeded in purifying EPO from the urine of patients with aplastic anemia. This led to a logarithmic increase in the rate at which new knowledge was acquired. The clumsy, technicianintensive bioassays were replaced by more-sensitive and more-precise immunoassays. Scientists at Amgen [14], working with antibodies against purified EPO, isolated complementary DNA and were able to transfect this into hamster ovary cells, grown en-masse to produce commercial amounts of EPO for clinical use. EPO is a 30.4-kD glycoprotein with four carbohydrate residues [13]. The latter prevent EPO from being rapidly cleared from the blood by the liver. EPO interacts as ligand for a specific receptor [15] (EPO-R) found predominantly on erythroid precursor cells. EPO-R is not found on multipotential hematopoietic stem cells and is not found on the early burst-forming units-erythroid (earliest committed erythroid precursors that form bursts of subcolonies in culture). Therefore, EPO is not required for cell differentiation. It begins to appear on the later burst-forming unitserythroid and is found in highest concentration on colony-forming units-erythroid (erythroid precursors that are only one or two divisions upstream from the first morphologically recognizable erythroid precursors, the proerythroblasts) [16] and proerythroblasts. These cells are the erythropoietin responsive cells (ERC). EPO-R contains two polypeptide chains on its extracellular component, which become homodimerized after interaction with their ligand [17]. This, in turn, activates the receptor and results in phosphorylation of Jak-2, which is either in close proximity or attached to the intracellular portion of EPO-R. This results in transmission of the signal via the Jak/Stat pathway and possibly also via Ras [18,19]. The signal that is transmitted to the nucleus prevents apoptosis and permits the cell to complete its terminal maturation into a reticulocyte and subsequently into an erythrocyte. EPO also increases the size of the ERC W. Fried/ Experimental Hematology 2009;37:1007–1015 population by stimulating proliferation of these cells. Accordingly, in an intact erythropoietic system, one in which the hematopoietic microenvironment, the multipotential stem cells and the early erythroid precursors (burst-forming units-erythroid) are intact and the nutrients required for terminal maturation are not limited, the rate of erythropoiesis is a function of the number of intact ERC and the amount of circulating EPO. Therefore, one would expect that as the ERC population decreases in numbers and/or function, the dose of EPO required to maintain the rate of erythropoiesis will increase. This has been demonstrated in mice exposed to increasing doses of irradiation [20] and is compatible with what is observed in patients with refractory anemias that are treated with EPO [21]. A corollary of this is that the amount of EPO required to maintain a given rate of erythropoiesis should be less if the ERC are increased. This is likely to be the explanation for the compensated hemolytic state. People with a chronic hemolytic condition, such as hereditary spherocytosis, often maintain an increased rate of erythropoiesis to compensate for their shortened RBC lifespan, with minor or no anemia and no increase in the EPO titer. The primary site of EPO production in adult mammals is the kidney [12]. In experimental animals, the site of EPO production in the kidney is a specialized peritubular cell found mainly in the proximal tubular region [22]. In fetal and neonatal life [23,24], the hepatocyte is the prime source of EPO production and this may continue, to a minor extent, into adult life [23,25]. In rodents, procedures that result in regeneration of hepatocytes increase hepatic EPO production [26]. In humans with end-stage renal failure, the hemoglobin and hematocrit sometimes increase during episodes of hepatitis [27]. EPO gene expression has been demonstrated in various extrarenal sites, including even the hematopoietic tissue of the bone marrow [28,29]. The physiologic significance of these extrarenal sites requires clarification. EPO is also produced by some neoplasms. The most common is the hypernephroma [30] and the next most common is the hepatoma [31]. However, a variety of other neoplasms have also been reported to produce paraneoplastic EPO [32,33]. The paraneoplastic production of EPO frequently results in erythrocytosis without hypoxia and with increased serum EPO levels that persist despite the erythrocytosis. EPO production is primarily regulated by the oxygen supply to a sensor in the kidney relative to its oxygen requirements [34]. Conditions that result in a decrease in oxygen delivery to the renal sensor will stimulate EPO production. This includes residence at high altitude, pulmonary disease that affects the diffusing capacity of the lungs and results in decreased uptake of oxygen, admixture of arterial and venous blood through a right to left shunt, decreased renal blood flow, etc. Conditions that increase oxygen delivery, such as erythrocytosis or breathing a gas mixture that contains an increased oxygen 1009 pressure, will decrease production of EPO. In conditions that decrease the oxygen needs, such as hypothyroidism and hypopituitarism, a normal rate of oxygen delivery represents plethora and causes EPO production and the serum EPO titer to decline. The oxygen sensor probably resides in proximity to the site of EPO production and may consist of a heme-containing protein [35]. The EPO gene is activated by a hypoxia-inducible factor (HIF) [36,37], which attaches to the hypoxia-sensitive region of the EPO gene to activate it. Because commercial EPO assays are not sensitive enough to detect small changes in EPO titer, it is not possible to reliably determine how great a hypoxic stimulus is required to increase EPO production. There is evidence that after phlebotomizing someone without a known erythropoietic defect of 500 mL whole blood, the erythropoietin titer does not increase detectably [38]. This is not surprising because there are so many ways in which our bodies can compensate for a small change in the oxygen-carrying capacity of the blood. Even if the rate of erythropoiesis remains constant and does not increase, the red cell mass will slowly recover (after losing 500 mL blood [240 mL RBCs] about 2 mL less RBCs will become senescent every day for 120 days. Accordingly, 2 mL of the lost 240 mL RBCs will be recovered daily). Although the ratio of oxygen delivery to oxygen requirements is the primary physiologic regulator of EPO production, there are others. Androgenic steroids [10,39,40], anabolic steroids [41], and cobaltous chloride [9] stimulate EPO production by an unknown mechanism. Protein deprivation [34] and inflammatory cytokines, such as interleukin-6 and tumor necrosis factor [42,43], decrease EPO production. This contributes to the anemia of chronic inflammatory disease and the anemia of cancer, as will be discussed later. There is also evidence in experimental animals that an increase in the RBC mass can decrease production of EPO independent of its effect on oxygen delivery [44,45]. Perhaps this effect is related to the resultant increase in whole blood viscosity. The plasma EPO titer at any given severity of anemia is inversely proportional to the effective rate of erythropoiesis. This has been observed under several conditions [46,47]. In rats exposed to hypoxia, plasma EPO titer peaks within 6 to 8 hours, but after 72 hours of exposure, when the RBC mass is not yet detectably increased, it is almost back to the prehypoxic level. In contrast, the rate of erythropoiesis, as measured by Fe59 uptake into newly formed erythrocytes, is increased after 24 hours, peaks after 48 hours of hypoxic exposure, and persists at a maximum level for 7 days (this is compatible with the explanation that less EPO is required to maintain the rate of erythropoiesis if the ERC population is enlarged). Three possible explanations have been proposed. The EPO titer may exert a negative feedback effect on EPO production. This was tested in an animal model and denied 1010 W. Fried/ Experimental Hematology 2009;37:1007–1015 [48]. The increase in ERC results in consumption of EPO [47]. This also was tested and found not to be the case [46,49,50]. Therefore, the most likely possibility is that the effective ERC population somehow exerts a negative feedback on EPO production. The phenomenon of the inverse effect of the ERC population on the plasma EPO titer has been observed in various situations in humans. Following intensive chemotherapy, the serum EPO titer rises before the hemoglobin and the hematocrit falls [51,52]. Treatment of patients with vitamin B-12 deficiency and with iron deficiency results in a fall in serum EPO titer before the hemoglobin and the hematocrit rise [53]. Serum EPO levels of patients with aplastic anemia and with myelodysplastic syndromes are higher than in those with comparable anemias associated with active erythropoiesis [54,55]. However, more direct data on EPO clearance rates in humans are needed before the hypothesis that ERC exert a negative feedback effect on EPO production is proven. It might be of interest to screen the EPO titers of patients who are considered to be hematologically normal for those that might have an EPO titer that is O2 standard deviations beyond the normal for the laboratory. A follow-up of such patients might indicate an occult marrow dyscrasia. Once EPO has interacted with its receptor on the erythroid progenitor cell, that cell can go on to express its terminal maturation program if the conditions required for the synchronous synthesis of hemoglobin and DNA are adequate. As stated earlier, under those conditions, the rate of erythropoiesis is a function of the serum EPO level and the size and integrity of the ERC population. Let us begin with a discussion of the factors that determine the ability of the erythroid precursors to synthesize hemoglobin. Hemoglobin molecules consist of four globin chains, each of which has a heme moiety attached. Defective globin synthesis generally is the result of mutations of the promoter portion that adversely affect one or more of the a- or the b-globin genes to produce a variety of thalassemia. The synthesis of heme occurs in the mitochondria of the erythropoietic precursor cells and is dependent on insertion of iron into preformed protoporphyrin molecules. Defective heme synthesis occurs because of iron deficiency, because iron is not released in sufficient quantity from its storage sites in the reticuloendothelial system as occurs in the anemia of chronic disease, or because there is a defect in either the structure of the mitochondria or in the ferrochetalase enzyme that catalyzes the insertion of iron into protoporphyrin. The resultant accumulation of iron in the mitochondria gives rise to the ringed sideroblasts, which are the diagnostic feature of sideroblastic anemias. To maintain a normal rate of erythropoiesis, the erythron requires an amount of iron that is equal to the amount required to replace the RBCs that become senescent daily. In an average adult 70-kg male, this would amount to about 20 mL RBCs or 20 mg iron. Females require 18 mg. Assuming 1 mg insensible loss daily, about 17 to 19 mg iron should become available from senescent RBCs, which were scavenged by the macrophages that day. If there is no known source of blood loss, only 1 mg iron should be required from food sources daily. Females, during their childbearing years, however, lose approximately 30 mg iron monthly during normal menses; and lose about 750 mg iron during a 250-day pregnancy. Therefore, premenopausal females require about 2 mg iron from food sources and during pregnancy about 4 mg (this assumes that they still have a 1-mg daily insensible loss). Most diets contain about 7 mg iron per 1,000 calories. Worldwide, the average caloric intake is about 2000 calories. Food iron comes in three varieties: ferrous, ferric, and heme. Iron is absorbed in the proximal duodenum by specialized cells called enterocytes [56]. Heme iron is readily absorbed into these cells, whereas ferric and ferrous iron are subject to chelation by a variety of substances in various foods. Absorption of ferric iron is also influenced by the pH of the intestinal lumen, because it is insoluble in an alkali medium. The divalent metal transporter located on the luminal surface of enterocytes, in proximity to an enzyme that reduces ferric iron to ferrous, facilitates transport of ferrous iron into the enterocyte [57]. The diet of more prosperous peoples contains a larger amount of heme iron, which is derived mainly from muscle tissue; whereas poorer diets include a larger percentage of inorganic iron. Once in the enterocyte, iron is either incorporated into ferritin and sloughed with the aging enterocyte or is transported through the basolateral surface of the enterocyte and enters the bloodstream, where it is attached to transferrin (TF1) for transport to the developing erythroid cells. There the iron-saturated TF1 interacts with the transferrin receptor (TFR1) for transport into the cell where the divalent metal transporter facilitates the release of iron from the TF1 and its transport to the mitochondria for synthesis of heme. Regulation of the amount of iron that is transported from the enterocyte into the bloodstream is critical, as only 1 or 2 mg is required by the erythroid precursors and, once their TFR1 is saturated, the remainder is likely to be taken up into the hepatocytes, the cardiac myocytes, etc. Accumulation of iron in these cells can cause serious tissue damage. Iron is transported from the basolateral surface of the enterocyte through a tubular transmembrane protein, ferroportin. (FPN1) [58,59]. This gateway protein is regulated by a hepatocyte generated protein, hepcidin [60,61] that binds to FPN1 and causes the phosphorylation of several amino acids on the intracellular portion of FPN1. This then causes the internalization and ubiquitization of the FPN1-hepcidin complex. Therefore, an increase in hepcidin production will decrease iron absorption from the gastrointestinal tract, whereas a decrease will have the opposite effect. W. Fried/ Experimental Hematology 2009;37:1007–1015 Synthesis of hepcidin is regulated by both a storage regulator and an erythropoietic regulator. The storage regulator controls production of hepcidin in accord with the body’s iron needs as determined by the body’s iron stores. This involves the complex interaction of the atypical class I major histocompatibility complex protein, HFE (the hemochromatosis gene), transferrin receptor 2 (TFR2). and hemojuvalin (HJV). HJV is a glycophosphoinositide linked protein on the hepatocyte membrane, which functions as a coreceptor with the receptor for the bone morphogenic proteins (BMP) [62]. The BMP-HJV receptor, when activated by interaction with its ligand, transmits a signal, by phosphorylation of SMAD, to the nucleus to activate the hepcidin gene and thereby increase the synthesis of hepcidin. The activation of the BMP-HJV receptor is postulated to be linked to the status of the body’s iron stores as follows: the HFE protein competes with diferric (saturated) transferrin for a binding site on TFR1. If, as occurs in iron overload states, there is an excess of diferric transferrin, then HFE binds to TRF2. The TRF2-HFE complex interacts with the BMP-HJV receptor to sensitize it and increase the synthesis of hepcidin. In the case of hypoferremia, on the other hand, HFE binds preferentially with TRF1. The TRF1-HFE complex cannot interact with the BMP-HJV receptor and hepcidin production is not increased. Increased hepcidin results in decreased iron absorption and decreased release of iron from the macrophages and visa versa [63]. The erythropoietic regulator is sensitive to changes in the rate of erythropoiesis and particularly in the rate of ineffective erythropoiesis [64,65]. An increase in the amount of ineffective erythropoiesis results in decreased production of hepcidin. This effect is more potent than that of the storage regulators and if both iron overload and increased ineffective erythropoiesis coexist, the erythropoietic effect will override that of the storage regulator and hepcidin production will decline and iron absorption will increase despite iron overload. The mechanism by which increased ineffective erythropoiesis causes a decrease in hepcidin synthesis is the subject of active research. Both EPO and the Hippel von Landau HIF have been shown to decrease hepcidin production by hepatocytes in vitro [66,67]. GDF15, a member of the transforming growth family (TGF-b) has been found, by transcription profiling, to be upregulated during accelerated erythropoiesis and is capable of suppressing hepcidin production. Therefore, it is also a potential mediator of the erythropoietic regulator [68]. Hepcidin is critically involved in regulating the amount of iron absorbed from the gastrointestinal tract. It is, however, also involved in regulating the availability of iron from the reticuloendothelial system. FPN1 is present on the membrane of the macrophages that phagocytose senescent RBCs and is the site through which iron is transported from the macrophages into the bloodstream. 1011 In addition to the storage regulators and the erythropoietic regulators of hepcidin production, there is also an inflammatory regulator, which is mediated through the inflammatory cytokine interleukin-6 [69]. This acts on the hepcidin gene in the hepatocyte and possibly also on a hepcidin gene in the monocyte to stimulate hepcidin production and thereby to inhibit iron absorption from the gastrointestinal tract and also to inhibit the release of iron from the macrophages. Interleukin-6 induced hepcidin production causes the characteristic changes of the anemia of chronic inflammatory and/or malignant disease. The increased hepcidin decreases the number of FPN1 molecules available to recycle iron from senescent erythrocytes and, therefore, patients with malignancy and/or inflammatory diseases have increased iron stores, decreased serum iron, and cannot compensate for the loss of RBCs that become senescent. They, therefore, become anemic. The anemia of chronic disease has been regarded by many as a virtual iron-deficiency anemia because there is a deficiency of iron being delivered to the erythroid precursors to satisfy their EPO receptors. As mentioned here, inflammatory cytokines also cause a decrease in EPO production, which contributes to the anemia. Let us return now to our average 70-kg male who requires 20 mg iron daily to compensate for the daily loss of senescent RBCs. This person requires 1 mg of iron from food sources, and he will have to recycle 19 mg iron from his senescent RBCs. Iron derived from newly phagocytosed RBCs is readily recycled to the erythroid precursors if the regulatory mechanism for hepcidin production is functioning normally and an adequate, but not excessive, amount of FPN1 molecules are present on the basolateral surface of the enterocytes and on the membranes of the macrophages. However, if there is an excess of hepcidin and excessive FPN1 have been internalized and ubiquitized, then there will be a decrease in the rate of iron absorption from the gastrointestinal tract and the newly deposited iron from senescent RBCs will not be completely recycled. The iron then is deposited in ferritin and with time it is converted to hemosiderin. The longer the iron is deposited, the less available it becomes [70]. In experimental animals, newly deposited iron is most readily mobilized from the macrophages. In humans, this concept has also been supported by the following clinical observations: Eschbach et al. [71,72] noted in their classical study on the treatment of the anemia of chronic renal failure with EPO that patients who responded with a brisk increase of their RBC mass often stopped responding and developed hypoferremia before their iron stores were exhausted. Similarly, patients with hemochromatosis who regenerate their RBCs rapidly after repeated phlebotomies often stop regenerating before their iron stores are totally exhausted. Conversely, if hepcidin production is inhibited, as in patients with hemochromatosis, iron uptake from the gastrointestinal tract increases 1012 W. Fried/ Experimental Hematology 2009;37:1007–1015 and the iron deposited in the macrophages is more readily released. This results in an increase in the iron-saturated TF1 and consequently in the uptake of iron into hepatocytes. This also explains why patients with hemochromatosis have less than the expected amount of iron stored in their macrophages. Persons with increased ineffective erythropoiesis due to thalassemia intermedia or myelodysplastic syndromes are prone to develop organ damage due to iron deposition into their hepatocytes and cardiac myocytes [73,74]. They absorb excess iron from the gastrointestinal tract. In addition, the iron that is deposited into their macrophages after blood transfusion is rapidly released because the erythropoietic regulator overpowers the iron storage regulator and the resulting decrease in hepcidin allows the iron to be transported out of the macrophages and become deposited in the hepatocytes. To complete the discussion of the nutrients required for the synchronous production of hemoglobin and for sufficient DNA to complete three terminal divisions, I will just mention the need for vitamin B-12 and folic acid to generate endogenous thymidine. The study of the role of EPO in human disease began in 1957, when Dr. Gurney and his colleagues [75] bioassayed plasma EPO levels of a large variety of anemic patients and observed that only those with renal failure regularly contained reduced EPO levels. This was subsequently also observed by Gallagher et al. [76]. In 1986, Cotes et al. [77] developed a reliable immunoreactive assay for EPO, which used recombinant DNA to produce pure EPO to obtain a specific anti-EPO antibody. This is the prototype for the commonly available commercial assays for serum EPO that are now available. For the most part, serum EPO in various anemias increases proportionally to the severity of the anemia [78–80]. However, as mentioned previously, serum EPO titer of patients with inflammatory states or malignancies is lower than that of comparably anemic patients with other anemias [78]. Also serum EPO titer of patients with anemias due to marrow failure are higher than those of comparably anemic patients with other anemias [79,80]. Also, the assay is best able to detect elevated EPO titers. Because the range of normal EPO titer is large, identification of reduced EPO titers is often tenuous [78–80]. Where then is the assay of the EPO titer clinically useful? It is essential to assay the endogenous EPO titer before beginning therapy with EPO in patients with myelodysplasia. If the serum EPO titer is excessive (O500 U), then it is unlikely that the person will respond because the very high endogenous EPO level probably is indicative of a very small effective ERC population. In patients with erythrocytosis, diagnosis of polycythemia rubra vera was usually made clinically using the criteria developed by the Polycythemia Study Group, because decreased serum EPO titers are not reliably detected [81]. Now, with the discovery of the role of the JAK-2 mutation in the pathogenesis of polycythemia rubra vera [82], the determination of EPO titer is even less useful. However, in patients with erythrocytosis without the common mutation in the JAK-2 gene, serum EPO titers are still useful [83]. I have found, however, that it is most useful to phlebotomize patients to a normal hematocrit prior to assaying the EPO titer because the plethoric condition might reduce serum EPO titer of patients with any of the forms of hypoxia-induced erythrocytosis. If serum EPO titer is still normal after the hematocrit is normalized, one might consider one of the less common forms of congenital erythrocytosis, or a less common mutation of the JAK-2 gene, detection of which requires a different probe [83]. The first clinical use of EPO was reported by Winearls et al. [84] in the United Kingdom and by Eschbach et al. [71] in the United States. These were combined phase I and II trials of patients with chronic renal failure on hemodialysis. Since then, extensive phase III trials have documented the efficacy of EPO to correct the anemia of renal failure in patients both on and off dialysis. Complications are few. However, one must be observant for development of functional iron deficiency, as the available iron stores are utilized by the rapid increase in erythropoiesis. Also, hypertension is observed to increase in some patients and must be treated. More recently, the optimum targeted hematocrit has been reduced to 11 g because of a suggestion that there is an increased incidence of thromboembolic complications if the hematocrit is completely normalized. Use of EPO has had a marked beneficial effect on the well-being of most patients with renal failure. Following the initial studies documenting the effectiveness of EPO in correcting the anemia of chronic renal failure, EPO has been used in the management of a variety of refractory anemias. These include, the anemia of chronic disease [85]; anemia of patients with various neoplasms that are undergoing chemotherapy [86], anemias of patients with myeloma [87]; anemia of some patients with myelodysplasia and aplastic anemia [88,89], and anemia associated with the use of antivirals to treat HIV [90]. The dosage of EPO required to treat these anemias must be significantly increased relative to that is effective in correcting the anemia of patients with renal failure. However, EPO has been successful in reducing the transfusion requirements and improving the quality of life of many patients with these disorders. It has also been used in patients without anemia that must undergo frequent phlebotomies to accumulate blood for autologous blood transfusions at the time of orthopedic surgery [91]. In 2003, Henke and coworkers [92] presented data that looked at the effect of EPO on the long-term survival of patients with head and neck cancers undergoing radiotherapy in a randomized double-blind placebo-controlled trial. Prior to that time, the endpoint of studies on the use of EPO in patients with the anemia of cancer were its effects W. Fried/ Experimental Hematology 2009;37:1007–1015 on the blood hemoglobin concentration, transfusion requirements, and effect on quality of life. In Dr. Henke’s study, EPO raised the hemoglobin, as expected and also the quality of life of the patients. However, the unexpected and very disturbing finding was that the patients who received EPO had a significantly shorter overall survival than did those in the placebo group. Leyland-Jones and colleagues [93] reported that administration of EPO to maintain normal hemoglobin levels in patients with metastatic breast cancer also shortened the overall survival of the EPO recipients. There are shortcomings to both of these studies, which I will not discuss here. However, there have also been other trials since with similar results [86,94]. The explanation is uncertain. One possibility is that in these studies, EPO was given to reach a higher-target hemoglobin than is now considered to be desirable; thereby increasing the incidence of thromboembolic events [94]. Another explanation is that EPO interacts with EPO receptors, which have been identified on the tumor cells. There is, however, uncertainty whether the investigators, studying these receptors had sufficiently specific antibodies to separate those that react with EPO receptors from those that react with heat shock proteins [95]. There is also evidence suggesting that EPO can react with receptors on endothelial cells to stimulate angiogenesis [96]. At this time, the reason(s) for the observed decreased survival of patients with cancer that receive EPO is unclear. However, the results of these studies have led to a change in the guidelines for use of EPO to treat the anemia of cancer. These new guidelines limit the use of EPO to the anemia of patients with cancer that are undergoing chemotherapy; and reduce the target blood hemoglobin concentration to 12 g/100 mL. Conclusions Since 1953, when Erslev [5] first demonstrated, in a convincing and reproducible way, the existence of EPO, much has been learned about the major sites of EPO production and the conditions that control its rate of production and the rate of erythropoiesis. Successful extraction of pure EPO from the urine of aplastic patients by Miyake and Goldwasser [13] in 1977 facilitated production of specific antibodies to EPO. Subsequently, it became possible to more accurately identify the cellular site of EPO production and its action at the cellular level. Also, this made possible the development of commercially available accurate and specific iimmuunoassays [77] for diagnostic purposes and the production of commercial amounts of EPO for therapeutic use [14]. There are, however, also new questions that have arisen and that are now the target of investigation. The success in treating patients with chronic renal failure and a variety of refractory anemias has been gratifying in that it has decreased the transfusion requirements and increased the quality-of-life of many patients. However, in the past 6 years, we have also been made aware of important 1013 complications of EPO therapy. EPO increases the incidence of thromboembolic disease in patients with malignancy and with renal failure who already have a hypercoagulable state [94]. This may be particularly pertinent if the blood hemoglobin concentration is raised to normal or near-normal levels. Also, there is evidence that patients with a variety of cancers who receive EPO may have a shortened overall survival [92,93]. This has led to development of new guidelines regarding who should receive EPO and what the optimal target blood hemoglobin concentration should be [86]. Trials in patients with breast cancer that reported that EPO shortened the overall survival suggested that the cancer cells contain EPO receptors that are activated by EPO. There is also data suggesting that endothelial cells contain EPO receptors and that EPO has angiogenic activity [96]. EPO receptors have been described on a number of nonerythroid cells. Their physiologic significance requires clarification. Also, extrarenal EPO production has been reported in a number of sites [28,29] (nonparaneoplastic). The significance of this extrarenal EPO also requires clarification. A great deal has been learned about EPO and erythropoiesis in the past 50 years. As is the case in all important research areas, important new knowledge generates important new questions. Conflict of Interest No financial interest/relationships with financial interest relating to the topic of this article have been declared. References 1. Bert P. Sur la richesse en hemoglobine du sang de animaux vivant sur les hauts. C R Acad Sci. 1882;94:805–806. 2. Carnot P, DeFlandre C. Sur l ‘activite’ hematopoietique des differents organs au cours de la regeneration du sang. C R Acad Sci. 1906;143: 432–434. 3. Grant WC, Root WS. Fundamental stimulus for erythropoiesis. Physiol Rev. 1952;32:449–498. 4. Reissman KR. Studies on the mechanism of erythropoietic stimulation in parabiotic rats during hypoxia. Blood. 1950;5:372–380. 5. Erslev AJ. Humoral regulation of red cell production. Blood. 1953;8: 349–357. 6. Plzak LF, Fried W, Jacobson LO, Bethard WJ. Demonstration of stimulation of erythropoiesis by plasma from anemic rats, using Fe59. J Lab Clin Med. 1955;46:671–678. 7. Fried W, Plzak LF, Jacobson LO, Goldwasser E. Assay of erythropoietin in hypophysectomized rats. Proc Soc Exp Biol Med. 1956;92:203–207. 8. Degowin RL, Hofstra D, Gurney CW. The mouse with hypoxia induced erythremia, an erythropoietin assay animal. J Lab Clin Med. 1962;60:846–852. 9. Goldwasser E, Jacobson LO, Fried W, Plzak LF. Mechanism of the erythropoietic effect of cobalt. Science. 1957;125:1085–1086. 10. Fried W, Gurney CW. Erythropoietic effect of the plasma from mice receiving testosterone. Nature. 1965;206:1160–1161. 11. Stohlman F Jr, Rath E, Ross JC. Evidence of a humoral regulation of erythropoiesis: Studies on a patient with polycythemia secondary to regional hypoxia. Blood. 1954;9:721–733. 12. Jacobson LO, Goldwasser E, Fried W, Plzak LF. Role of the kidney in erythropoiesis. Nature. 1957;139:633–634. 1014 W. Fried/ Experimental Hematology 2009;37:1007–1015 13. Miyake T, Goldwasser E. Purification of human erythropoietin. J Biol Chem. 1977;252:5558–5564. 14. Lin FK, Suggs S, Lin CH, et al. Cloning and expression of the human erythropoietin gene. Proc Natl Acad Sci U S A. 1985;82:7580–7584. 15. Krantz SB, Goldwasser E. Specific binding of erythropoietin in spleen cells infected with the anemia strain of Fried virus. Proc Natl Acad Sci U S A. 1984;81:7574–7578. 16. Broudy VC, Lin N, Brice M, Nakamoto B, Papayannopoulou T. Erythropoietin receptor characteristics on primary human erythroid cells. Blood. 1991;15:2583–2590. 17. McCaffrey PJ, Fraser JK, Lin FK, Berridge MV. Subunit structure of the erythropoietin receptor. J Biol Chem. 1989;264:10507–10512. 18. Witthuhn BA, Quelle FW, Silvennoinen O, et al. JAK2 associates with the erythropoietin receptor and is tyrosine phosphorylated and activated following EPO stimulation. Cell. 1993;74:227–236. 19. Miura O, Nakamura N, Quelle FW, Witthuhn BA, Ihle JN, Aoki N. Erythropoietin induces association of the JAK2 protein tyrosine kinase with the erythropoietin receptor in vitro. Blood. 1994;84:1501–1507. 20. Kilbridge T, Fried W. Response of mice with decreased number of hematopoietic stem cells to doses of erythropoietin. J Lab Clin Med. 1968;72:85–92. 21. Stein RS. The role of erythropoietin in the anemia of myelodysplastic syndrome. Clin Lymphoma. 2005;6:52–55. 22. Fisher JW, Koury S, Ducey T, Mendel S. Erythropoietin production by interstitial cells of hypoxic monkey kidneys. Br J Haematol. 1996;95: 27–36. 23. Koury ST, Bondurant MC, Semenza GL, Koury MJ. The use of in situ hybridization to study erythropoietin gene expression in murine kidney and liver. Microsc Res Tech. 1993;39:25–29. 24. Zanjani ED, Ascensao JL, McGlave PM, Banisadre M, Ash RC. Studies on the liver to kidney switch of erythropoietin production. J Clin Invest. 1981;67:1183–1188. 25. Fried W. The liver as a source of extrarenal erythropoietin production. Blood. 1972;40:671–677. 26. Fried W, Barone J, Schade S, Anagnostou A. Effect of carbon tetrachloride on extrarenal erythropoietin production. J Lab Clin Med. 1979;93:700–705. 27. Simon P, Meyrier A, Tanqueerel T, Ang KS. Improvement of anemia in hemodialysed patients after viral or toxic hepatic cytolysis. Br Med J. 1980;280:892–894. 28. Conrad KP, Benyo DF, Westerhausen-Larsen A, Miles TM. Expression of erythropoietin by the human placenta. FASEB J. 1996;10:760–768. 29. Zhang F, Laneville P, Gagnon RF, Morin B, Brox AG. Effect of chronic renal failure on the expression of erythropoietin message in a murine model. Exp Hematol. 1996;24:1469–1474. 30. Burk JR, Lertora JJ, Martinez Jr IR, Fisher JW. Renal cell carcinoma with erythrocytosis and elevated erythropoietic stimulatory activity. South Med J. 1977;70:955–958. 31. Scott D, Theologides A. Hepatoma, erythrocytosis, and increased serum erythropoietin developing in long-standing hemochromatosis. Am J Gastroenterol. 1974;61:206–211. 32. Suzuki M, Takamizawa S, Nomaguchi K, et al. Erythropoietin synthesis by tumour tissues in a patient with uterine myoma and erythrocytosis. Br J Haematol. 2001;113:49–51. 33. Matsuo M, Koga S, Kanetake H, et al. EPO-producing gastric carcinoma in a hemodialysis patient. Am J Kidney Dis. 2003;42:E3–E4. 34. Fried W, Plzak LF, Jacobson LO, Goldwasser E. Studies on erythropoiesis III. Factors controlling erythropoietin production. Proc Soc Exp Biol Med. 1957;94:241–243. 35. Goldberg MA, Dunning SP, Bunn HF. Regulation of the erythropoietin gene: evidence that the oxygen sensor is a heme protein. Science. 1988;242:1412–1415. 36. Wang GL, Semenza GL. General involvement of hypoxia inducible factor in transcriptional response to hypoxia. Proc Soc Natl Acad Sci U S A. 1993;90:4304–4308. 37. Huang LE, Ho V, Kraine D. Erythropoietin gene regulation depends on heme dependant oxygen sensing and assembly of interacting transcription factors. Kidney Int. 1997;51:548–522. 38. Kickler TS, Spivak JL. Repeated blood donations and erythropoietin levels. JAMA. 1989;261:1443–1444. 39. Mirand EA, Gordon AS, Wenig J. Mechanism of testosterone action on erythropoiesis. Nature. 1965;206:270–272. 40. Alexanian R, Vaugh WH, Ruchelman MW. Erythropoietin excretion in man following androgens. J Lab Clin Med. 1967;70:777–785. 41. Doane B, Fried W, Schwartz F. Response of uremic patients to Nandrolone Decanoate. Arch Intern Med. 1975;135:972–975. 42. Jelkmann WE, Fandrey J, Frede S, Pagel H. Inhibition of erythropoietin production by cytokines. Implications for the anemia involved in inflammatory states. Ann N Y Acad Sci. 1994;718:300–309. 43. Krantz SB. Pathogenesis and treatment of the anemia of chronic disease. Am J Med Sci. 1994;307:353–354. 44. Kilbridge T, Fried W, Heller P. The mechanism by which plethora suppresses erythropoiesis. Blood. 1969;33:104–113. 45. Necas E, Neuwirt J. Feedback regulation by red cell mass of the sensitivity of the erythropoietin producing organ to hypoxia. Blood. 1970;36:754–763. 46. Fried W, Heller P, Johnson C. Observations on regulation of erythropoiesis during periods of prolonged hypoxia. Blood. 1970;36:607– 616. 47. Stohlman F, Brecher G. Humoral regulation of erythropoiesis V. Relationship of plasma erythropoietin activity to bone marrow activity. Proc Soc Exp Biol Med. 1959;100:40–43. 48. Fried W, Barone-Varelas J. Regulation of the plasma erythropoietin level in hypoxic rats. Exp Hematol. 1984;12:706–711. 49. Fried W, Knospe WH, Trobaugh FE Jr. Regulation of plasma erythropoietin levels in mice with impaired response to erythropoietin. J Lab Clin Med. 1971;78:48–56. 50. Naets JP, Wittek M. Effect of erythroid hyperplasia on utilization of erythropoietin. Nature. 1965;206: 736–728. 51. Beguin Y, Baron F, Fillet G. Influence of marrow erythropoietic activity on serum erythropoietin levels after autologous stem cell transplant. Haematologia. 1998;83:1076–1081. 52. Cazzola M, Guarnone R, Cerani P, Rovati A, Beguin Y. Red blood cell precursor mass as an independent determinant of serum erythropoietin level. Blood. 1998;91:239–241. 53. de Klerk G, Rosengarten PC, Vet RJ, Goudsmit R. Serum erythropoietin titers in anemia. Blood. 1981;58:1164–1170. 54. Hammond DA, Ishikawa A, Keighly G. The relationship between erythropoietin and severity of anemia in hypoplastic and hemolytic states. In: Jacobson LO, Doyle M, eds. Erythropoiesis. New York: Grune and Stratton Inc; 1962. p. 351–358. 55. Finne PH. On the correspondence between red cell production and plasma erythropoietin level. Scand J Clin Lab Invest. 1965;17: 135–141. 56. Morgan EH, Oates PS. Mechanisms and regulation of intestinal iron absorption. Blood Cells Mol Dis. 2002;29:384–399. 57. Mims MO, Prchal JT. Divalent metal transporter 1. Hematology. 2005; 10:339–345. 58. Abboud S, Haile DJ. A novel mammalian iron-regulated protein involved in intracellular iron metabolism. J Biol Chem. 2000;275: 19906–19912. 59. Donovan A, Lima CA, Pincus JL, et al. The iron exporter ferroportin/Sic40a1 is essential for iron homeostasis. Cell Metab. 2005;1:191–200. 60. Park CH, Valore EV, Waring AJ, Ganz T. Hepcidin, a urinary antimicrobial peptide, synthesized in the liver. J Biol Chem. 2001; 276:7806–7810. 61. Nemeth E, Tuttle MS, Powelson J, et al. Hepcidin regulates cellular iron efflux by binding to ferroportin and inducing its internalization. Science. 2004;306:2090–2093. W. Fried/ Experimental Hematology 2009;37:1007–1015 62. Babitt JL, Huang FW, Xia Y, Sidis Y, Andrews C, Lin HY. Modulation of bone morphogenetic protein signaling in vivo regulates systemic iron balance. J Clin Invest. 2007;117:1933–1939. 63. Ganz T. Molecular control of iron transport. J Am Soc Nephrol. 2007; 18:394–400. 64. Pak M, Lopez MA, Gabayan V, Ganz T, Rivera S. Suppression of hepcidin during anemia requires erythropoiesis. Blood. 2006;108: 3730–3735. 65. Gardeghi S, Marongiu MF, Ramos P, et al. Ineffective erythropoiesis in (beta) thalassemia is characterized by increased iron absorption mediated by-down regulation of hepcidin and up-regulation of ferroportin. Blood. 2007;109:5027–5035. 66. Pinto JP, Ribeiro S, Pontes H, et al. Erythropoietin mediates hepcidin expression in hepatocytes through OPOR signaling and regulation of C/EBPalpha. Blood. 2008;111:5727–5733. 67. Peyssonnaux C, Zinkernage AS, Schuepbach RA, et al. Regulation of iron homeostasis by the hypoxia-inducible transcription factors (HIFs). J Clin Invest. 2007;117:1926–1932. 68. Tanno T, Bhanu NV, Oneal PA, et al. High levels of GDF15 in thalassemia suppress expression of the iron regulatory protein hepcidin. Nat Med. 2007;13:1096–1101. 69. Wrighting DM, Andrews NC. Interleulin-6 induces hepcidin expression through STAT3. Blood. 2006;108:3204–3209. 70. Schade SG, Fried W. The utilization of senescent re cell and hemolysate iron for erythropoiesis. Proc Soc Exp Biol Med. 1976; 151:78–83. 71. Eschbach JW, Egrie JC, Downing MR, et al. Correction of the anemia of end stage renal failure with recombinant human erythropoietin. Results of a combined phase I and II clinical trial. N Engl J Med. 1987;316:73–78. 72. Eschbach JW, Abdulhadi MH, Browne JK, et al. Recombinant human erythropoietin in anemic patients with end stage renal disease. Ann Intern Med. 1989;111:992–1000. 73. Origa R, Galanello R, Ganz T, et al. Liver iron concentrations and urinary hepcidin in beta thalassemia. Haematologica. 2007;92:583–588. 74. Cazzola M, Malcovati L. Myelodysplastic syndromesdcoping with ineffective erythropoiesis. N Engl J Med. 2005;352:536–538. 75. Gurney CW, Goldwasser E, Pan C. Studies on erythropoiesis. IV. Erythropoietin in human plasma. J Lab Clin Med. 1957;50:534–540. 76. Gallagher NI, McCarthy JM, Hart KT, Lange RD. Evaluation of plasma erythropoietic stimulating factor in anemic uremic patients. Blood. 1959;14:662–667. 77. Cotes PM, Dor’e CL, Liu Yin JA, et al. Determination of serum immunoreactive erythropoietin in the investigation of erythrocytosis. N Engl J Med. 1986;315:283–287. 78. Ward HP, Kurnick JE, Pisarczyk MJ. Serum erythropoietin in anemias associated with chronic infection, malignancy, and primary hematopoietic disease. J Clin Invest. 1971;50:332–335. 79. Erslev AJ, Wilson J, Caro J. Erythropoietin in anemic non-uremic patients. J Lab Clin Med. 1987;109:429–433. 80. Jelkmann W, Weidmann G. Serum erythropoietin level: relationship to blood hemoglobin concentration and erythrocytic activity of the bone marrow. J Mol Biol. 1990;68:403–407. 81. Berlin NI, Wasserman LR. Polycythemia vera: a retrospective and reprise. J Lab Clin Med. 1997;130:366–372. 1015 82. James C, Ugo V, LeCouedic J-P, et al. A unique clonal JAK2 mutation leading to constitutive signaling causes polycythaemia vera. Nature. 2005;434:1144–1147. 83. Tefferi A, Thiele J, Orazi A, et al. Proposals and rationale for revision of the World Health Organization diagnostic criteria for polycythemia vera, essential thrombocythemia, and primary myelofibrosis: recommendations from an ad hoc international expert panel. Blood. 2007;110:1092–1096. 84. Winearls GC, Oliver DO, Pippard MJ, et al. Effect of human erythropoietin derived from recombinant DNA on the anemia of patients maintained by chronic hemodialysis. Lancet. 1986;2:1175–1178. 85. Means RT Jr. Erythropoietin in the treatment of anemia in chronic infectious, inflammatory and malignant diseases. Curr Opin Hematol. 1995;2:210–213. 86. Rizzo JD, Somerfield MR, Hagerty KL, et al. Use of epoietin and darbepoietin in patients with cancer: 2007 American Society of Hematology/American Society of Clinical Oncology clinical practice guideline update. Blood. 2008;111:25–41. 87. Mittleman M, Zeidman A, Fradin Z, Magazanik A, Lewinski UH. Recombinant human erythropoietin in the treatment of multiple myeloma-associated anemia. Acta Haematol. 1997;98:204–210. 88. Mundle S, Lefebvre P, Vekeman F, Duh MS, Rastogi R, Moyo V. An assessment of erythroid response to epoeitin alpha as a single agent versus in combination with granulocyte or granulocyte-macrophage colony-stimulating factor in myelodysplastic syndromes using a meta-analysis approach. Cancer. 2009;15:706–715. 89. Casadevail N, Duroeux P, Dubois S, et al. Health, economic, and quality-of-life effects of erythropoietin and granulocyte-colony stimulating-factor for the treatment of myelodysplastic syndromes: a randomized, controlled trail. Blood. 2004;104:321–327. 90. Henry DH, Beall GN, Benson CA, et al. Recombinant human erythropoietin in the treatment of anemia associated with human immunodeficiency virus (HIV) infection and Zidovudine therapy. Ann Intern Med. 1992;117:739–748. 91. Goodnough LT, Price KD, Friedman M, et al. A phase III trial of recombinant human erythropoietin therapy in nonanemic orthopedic patients subjected to aggressive removal of blood for autologous use: dose, response, toxicity, and efficacy. Transfusion. 1994;34:66–71. 92. Henke M, Laszig R, Rube C, et al. Erythropoietin to treat head and neck cancer patients with anemia undergoing radiotherapy: randomized, double-blind, placebo-controlled trial. Lancet. 2003;362:1255– 1260. 93. Leyland-Jones B, Semiglazov V, Pawlicki M, et al. Maintaining normal hemoglobin levels with epoietin alfa in mainly nonanemic patients with metastatic breast cancer receiving first line chemotherapy: a survival study. J Clin Oncol. 2005;23:5960–5972. 94. Bennett CL, Silver SM, Djulbegovic B, et al. Venous thromboembolism and mortality associated with recombinant erythropoietin and darbopoietin administration for the treatment of cancer associated anemia. JAMA. 2008;299:914–924. 95. Fandry J. Erythropoietin receptors on tumor cells: what do they mean. Oncologist. 2008;13(Suppl 3):16–20. 96. Ribatti D, Marzulla A, Gentile A, et al. erythropoietin/erythropoietin receptor system is involved in angiogenesis in human hepatocellular carcinoma. Histopathology. 2007;50:591–596.