Special Procedures in Veterinary Radiology-
advertisement
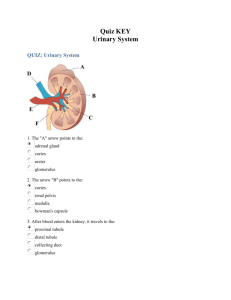
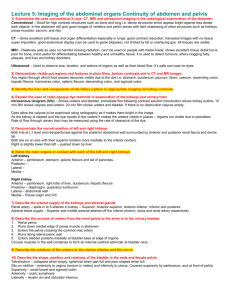
Special Procedures in Veterinary Radiology--Urogenital Travis C. Saveraid, DVM, DACVR Assistant Clinical Professor College of Veterinary Medicine – University of Minnesota Roentgen Signs • Margin • Shape • Opacity • Number • Size • Location 1 Urogenital Contrast Procedures • Intravenous Pyelogram (IVP); a.k.a. Intravenous Urogram (IVU), Excretory Urogram (EU) • Cystography (positive, negative, double) • Urethrography (retrograde, normograde) • Vaginography IVP IVP-indications • Identification / characterization of kidneys and ureters • Ectopic ureters • Suspected renal or ureteral calculi • Identification of enhancement voids in renal parenchyma • Rough estimate of renal function 2 IVP-indications • Abnormal renal size/shape on survey radiographs or palpation • Inability to identify kidney(s) on palpation or radiographs • Identify filling defects in renal pelvis / ureters • Hematuria without lower urinary tract signs • Suspected ureter rupture IVP-indications • Incontinence • Assess involvement of kidney/ureter in adjacent disease processes (e.g. neoplasia in bladder trigone) • Suspected pyelonephritis 3 Diverticulum Renal Pelvis Ureter IVP-contraindications • • • • DEHYDRATION Allergy to Iodine Heart failure Renal failure/azotemia are NOT contraindications but will affect the quality of the study 4 IVP-complications • Vomiting • Hemodynamic effects (hypotension, hypervolemia) • Contrast medium induced renal failure • Allergic reaction to contrast (hives, anaphylaxis) • Non-diagnostic study IVP-materials • Enema materials • Contrast agent— iodinated (ionic fine for most patients, consider using nonionic for azotemic or critical patients • IV catheter – typically cephalic vein IVP-materials • Compression band? - Vetrap • Fluoroscopy unit – if available • Crash kit – Fluids – Endotracheal tube – Drugs (epinephrine, steroids, antihistamines, dopamine) 5 IVP-preparations • Fast 12-24 Hours, enemas as needed to clear colon • Survey radiographs to establish technique, assess preparation, and check for changes since last radiographs • Sedation or anesthesia can be helpful in some patients Non-prepared abdomen. Prepared Abdomen 6 Collect Urine for Urinanalysis before IVP • Most contrast will increase urine specific gravity for up to 24 hours following IVP • Some contrast medium inhibits growth of urinary pathogens • If urine not collected before IVP, collect urine at least 24 hours after procedure. IVP-procedure • Details vary from reference to reference and radiologist to radiologist • Basic principles – Adequate dose for opacification of tract – Adequate timing to assess functional questions – Adequate views to assess anatomic questions (e.g. obliques for ureter termination) IVP-procedure • Typical dose 800-900 mg I/kg body weight – Most ionic agents are 350-400 mg I/ml, so 1 ml/lb (Omnipaque is 240 mg I/ml) – Maximum volume 90ml – Dose may be increased 1.5 to 2 X for azotemic patients to compensate for poor uptake – Inject as a bolus through catheter – Helps to warm contrast (less viscous) 7 IVP-procedure • Ventrodorsal view at time 0 • VD and lateral views at 5, 10, 20 and 40 minutes • Oblique lateral views (or fluoro) at 5 minutes to assess termination of distal ureters IVP-options • Compression band is referred to in some references – Tight bandage around caudal abdomen – Increases distension of pelvis and proximal ureters – Yields little additional information and carries small risk • Concurrent negative cystogram – Urethral catheter placed, bladder distended with gas (room air o.k. in most situations, NO2 or CO2 in cases of hematuria) – Provides improved contrast with the ureters as they enter the trigone – Helpful for suspected ectopic ureters IVP-options 8 IVP-options • “Paddle” views – Radiolucent paddle (e.g. wooden spoon) gently applied to abdomen during exposure to displace organs – Particularly useful to displace intestines away from kidneys and bladder – Less useful in large, blocky patients – May need to decrease technique (thinner) Bladder Stones? Yes – Look closely! 9 IVP-normal findings • Three phases – Angiogram phase: all blood vessels opacify, very brief (usually miss it), not too relevant in our patients – Nephrogram phase: kidneys are actively concentrating iodine, persists to some degree throughout study. Early phase cortex brighter than medulla, later enhancement is uniform – Pyelogram phase: pelvis and ureters enhance Survey Angiography phase to early Nephrogram phase IVP-normal findings • Uniform, symmetric renal enhancement • Opacity of kidneys fades over time • Size (on VD view) – Dog: 2.5-3.5 x L2 – Cat: 2.4(1.9?)-3.0 x L2 • Shape elongated, may be flattened on lateral view (cats slightly rounded) 10 IVP-normal findings • Without abdominal compression, renal pelvis and pelvic recesses approximately 2mm or less • Pelvis and recesses sharply marginated • Proximal ureter generally less than 2.5 mm • Visibility of ureters is variable due to peristalsis IVP-normal IVP-normal 11 IVP-normal findings • Ureters course medially on VD, dorsally on lateral from renal pelvis • Ureters often superimposed on spine on VD, each other on lateral • Ureters terminate at trigone dorsally, with a hook • Bladder gradually fills with contrast IVP-normal findings IVP-abnormal findings • Enhancement timing – – – – – – – Never Poor, fading Poor, persistent Poor, increasing Fair-good, fading (normal) Fair-good, persistent Fair-good, increasing 12 IVP-no enhancement • Renal absence (agenesis, excision) • No blood flow (infarcted, transected, ligated, avulsed) • Nonfunctional (may get vascular blush) • Contrast dose too low, too slow or wrong place (extravascular, connectors popped loose) Unilateral enhancement 13 IVP-Poor, fading • Any cause of polyuric renal failure • Contrast dose too low or too slow IVP-poor, persistent • Chronic glomerular dysfunction • Non-specific generalized renal disease IVP-poor, increasing • Acute obstruction • Hypotension • Ischemia 14 IVP-good, persistent • Acute tubular necrosis • Contrast mediuminduced renal failure • Hypotension postcontrast IVP-good, increasing • Hypotension post contrast • Acute obstruction • Contrast mediuminduced renal failure IVP-abnormal findings • Enhancement pattern – – – – Uniform (normal) Focally non-uniform Multifocally non-uniform Absent 15 IVP-focal • NAG (neoplasia, abscess, granuloma) • Cyst • Infarct IVP-focal IVP-multifocal • NAGs (including FIP) • Polycystic • Infarcts (including pyelonephritis) • Chronic generalized disease 16 IVP-abnormal findings • Size – Too small – Too large • Shape – Too round (usually also large) – Irregular • Margin – Irregular – Fuzzy IVP-normal size, irregular • NAG with atrophy of more normal tissue • Chronic infarcts • Chronic inflammation • PKD • Remember you don’t know how big they were to begin with… IVP-small, smooth • Hypoplasia • Glomerulonephritis • Amyloidosis 17 IVP-small, irregular • “End-stage” renal disease • Dysplasia IVP-large, smooth • Hydronephrosis • Infiltrate (neoplasia, amyloid) • Inflammation • Hypertrophy • Perinephric pseudocysts • Subcapsular fluid or infiltrate IVP-large, smooth 18 IVP-large, smooth IVP-large, irregular • NAG • Hematoma • Perirenal pseudocyst • Polycystic Kidney Disease (PKD) IVP-fuzzy margin • Perinephric edema • Perinephric hemorrhage • Urine leak 19 IVP-abnormal findings • Number – Too few – Too many • Location – Formed in wrong location? – Herniated? – Displaced? IVP-number • Too few—see “non opacification” • Too many—transplant (hopefully in history), supernumery kidneys (a.k.a. renal duplication) has been reported, RARE – If the extra kidney-shaped thing on surveys doesn’t enhance, probably not a kidney IVP-location • Anomalous location not uncommon, particularly left • Kidney herniations are uncommon, can be body wall, diaphragm • Being displaced by an adjacent mass is most common 20 IVP-abnormal findings • Pelvis abnormal size – Large • Shape/Margin – Irregular – Rounded • Opacity – Filling defects IVP-pelvis enlarged • Pyelectasia, mild – Physiologic – Pre-hydronephrosis • Hydronephrosis – Obstructive – Pyelonephritis – Space-occupying lesion IVP-pelvis irregular, rounded • “Marginal” filling defects (next slide) • Pyelonephritis • Neoplasia 21 IVP-pelvic filling defects • NAG • Calculi (more detail in cysto. section) • Blood clots IVP-abnormal findings • Ureter size – Large – Small • Shape/Margin/opacity – Dilation – Irregularity – Filling defects • Location 22 IVP-ureter large, small • Large=hydroureter – Obstructive – Ureteritis • Small=stricture Ureteral Obstruction IVP-ureter stricture 23 IVP-ureter irregular • Ureteritis • Infiltration – Most commonly from bladder neoplasia IVP-ureter filling defects • Calculi • Blood clots • Bubbles IVP-ureter filling defects 24 IVP-ureter location • Ectopic ureter common cause of incontinence – – – – – – – Urethra Vagina Uterus Vulva Colon “tunneling” Females >>> Males IVP-ureter location • Hydroureter is common, but not invariable • Pyelonephritis is often concurrent • Other anomalies may be present (ureterocele, pelvic bladder, etc) • Often difficult to capture – Gas in bladder, “paddle” views, obliques, fluoro can help IVP – Ectopic Ureter 25 IVP-ectopic ureter IVP-ectopic ureter IVP-ectopic ureter 26 IVP-ureter rupture • Should be considered with any retroperitoneal fluid/loss of detail • Can be difficult to “capture”, particularly if tear is small and renal function is poor IVP-ureter rupture IVP Alternatives-ultrasound • Advantages: Provides better anatomic and vascular information. Allows for acquiring samples (FNA or biopsy of renal parenchyma, pyelocentesis). Can combine with radiography (pyelography). • Disadvantages: Not as widely available. No functional information. More operator and equipment dependent. Findings often nonspecific and may be misleading. 27 Ultrasound IVP Alternatives-scintigraphy • Advantages: Provides detailed functional information (global and each kidney) • Disadvantages: Not widely available. Makes patient radioactive. Limited anatomic information. • Advantages: Detailed cross sectional anatomy (no superimposition) • Disadvantages: Not widely available, expensive. Greater radiation dose. Less temporal information. Requires heavier sedation or general anesthesia IVP AlternativesCT scan 28 Cystography Cystography-indications • To determine the following for the urinary bladder: – – – – – Location Shape Contents Integrity Wall thickness and texture Cystography-indications • • • • Hematuria with lower urinary tract signs Palpable abnormality (e.g. crepitus) Recurrent urinary tract infections Lower urinary tract signs without evidence of infection on urinalysis 29 Cystography-indications • Abnormalities on survey radiographs – – – – Opacity Shape Size “Number” • As an aid in surgical planning for known abnormality Cystography-indications • To investigate other mass effects and diseases in the area of the bladder • To investigate causes of urinary incontinence or retention • Suspected rupture Cystography-contraindications • Really are none other than, perhaps, previous allergic response to iodine • Some known or suspected conditions may alter the protocol 30 Cystography-complications • • • • • Bladder rupture Fatal gas embolus Hematuria Splitting of mucosa Vesicoureteral reflux (risk of inducing pyelonephritis if cystitis present) • Infection Cystography-materials • Urinary catheter (Foley if possible, stopcock, lube • Positive contrast material (ionic iodine, NOT BARIUM) • Negative contrast material (gas; room air o.k., but risk of fatal air embolism, CO2 or NO2 safer) • Sedation? Cystography-materials 31 Cystography-preparations • Fast and enemas as for IVP • Survey radiographs • Sedation • Urinary catheter placed and urine drained Cystography-procedure From: Manual of Veterinary Echocardiography; June A. Boon Cystography-procedure • Urinary bladder distended with gas until palpably full (not taut) • Draw up 10cc/kg and palpate constantly while infusing, also check for back pressure on the syringe • After bladder distended with gas, instill a small “puddle” of full-strength positive contrast (1-5cc total, depending on size of the bladder; can always put more in!) 32 Cystography-procedure • Have less bubbles when inject air first • Roll patient 360° to coat mucosa with positive contrast • Take right AND left lateral views, VD (or two obliques off of VD) Cystography-options • Can instill local anesthetic solution first to decrease spasticity • Can use only gas (negative cystography) or only iodine (positive cystography) rather than “double contrast” – Negative-not very helpful – Positive-use dilute agent (25%), often precedes urethrography, arguably better for diverticuli Cystography-normal findings • Bladder should be oval with a caudal taper toward trigone (cats more spherical, especially males) • Mucosal surface should be smooth • Wall should be approximately 1 mm thick and uniform • No filling defects in puddle 33 Cystography-normal findings • Distended bladder should be entirely within the abdomen • Minimal contrast may reflux into the ureters and even the renal pelvis • No contrast material should leak into the peritoneum or retroperitoneum Cystography-normal Cystography - Normal 34 Cystography - Normal Cystography-normal Cystography-abnormal findings • Mobile filling defects – – – – Air bubbles Stones Blood clots Foreign bodies • Immobile filling defects – Attached stones/clots/foreign bodies – Masses 35 Cystography-stones Cystography-stones Cystography-stones • Opaque stones (On SURVEYS-all lucent with positive contrast) – Oxalate – Silica – Phosphate (less opaque than above) • Lucent stones – Cystine – Urate • Algorithm exists on CVM website 36 Cystography-air bubbles • Most common artifact in lower urinary tract procedures • Mimic stones • Differentiating features – Round unless in direct contact with another bubble (side flattens) – Change with time and position (move, dissipate, coalesce with others) – At margins of puddle (remember that “down” is the MIDDLE of the puddle) Cystography-air bubbles Cystography-blood clots • Typically very irregular, inhomogeneous opacity, poorly marginated, and mobile • Organized, adherent clots are dead ringers for masses • Lavage may break up clot, also should dissipate with time (hours to days) 37 Cystography-abnormal findings • • • • • Wall abnormally thick Wall irregular without distinct mass Outpouching of wall Leakage of contrast material Dissection of contrast material into wall Cystography-wall thickness • • • • Neoplasia Inflammation Hemorrhage Edema Cystography – Wall Thickness 38 Cystography – Wall Dissection Cystography-outpouching wall • Urachal diverticulum common congenital – May predispose to UTI • Can see eventration with trauma (basketball with torn cover) Cystography-leakage 39 Cystography-leakage Bladder Rupture Cystography-abnormal findings • Intrapelvic (“pelvic”) bladder • Bladder displaced into hernia • Bladder displaced by other structures 40 Cystography-displacement Cystography-displacement Cystography-displacement 41 Cystography Alternativesultrasound • Advantages: Fast, non-invasive, may allow sampling, can potentially find smaller abnormalities • Disadvantages: May miss “big picture” lesions, operator dependent, expensive equipment Bladder Ultrasound Cystography Alternativescystoscopy • Advantages: allows direct visualization and sampling of lesions • Disadvantages: expensive, time consuming, operator dependent, patient size dependent, may not be able to see whole bladder 42 ??????????????????????????? 43