Mesenteric Meckel's diverticulum: a real variant
advertisement

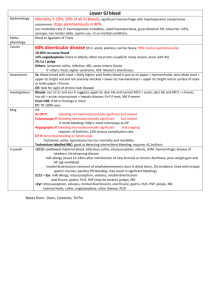
eISSN 1308-4038 International Journal of Anatomical Variations (2013) 6: 145–148 Case Report Mesenteric Meckel’s diverticulum: a real variant Published online September 11th, 2013 © http://www.ijav.org Susanne G. CARPENTER Ann E. McCULLOUGH [2] Shabana PASHA [3] Kristi L. HAROLD [1] [1] Departments of Surgery [1], Pathology [2], Gastroenterology [3], Mayo Clinic, Phoenix, AZ, USA. Abstract A Meckel’s diverticulum is the most common congenital abnormality of the gastrointestinal tract and can present a variety of diagnostic and surgical challenges. A longstanding surgical dictum is that a Meckel’s diverticulum must be anti-mesenteric. This study reports the case of an adult male who presented with an obscure gastrointestinal bleed and was ultimately found to have a Meckel’s diverticulum on the mesenteric intestinal border which was resected laparoscopically. Diagnostic characteristics that facilitate identification of a Meckel’s diverticulum along with reported deviations from these characteristics are reviewed in this study. © Int J Anat Var (IJAV). 2013; 6: 145–148. Kristi Harold, MD Mayo Clinic Arizona 5777 E. Mayo Blvd. Phoenix, AZ 85054 USA. +1 (480) 342-2849 harold.kristi@mayo.edu Received July 4th, 2012; accepted September 30th, 2012 Introduction Key words [Meckel’s diverticulum] [mesenteric sided Meckel’s diverticulum] [Meckel’s diverticulitis] [congenital gastrointestinal anomalies] Case Report A Meckel’s diverticulum (MD) is the most common congenital A 35-year-old otherwise healthy gentleman noticed a small anomaly of the gastro-intestinal tract, and can present quantity of maroon colored stools for one week, worsening over diagnostic and surgical challenges. Arising from failure time. He eventually reported to a local emergency department of the omphalomesenteric duct to close properly, MD can with symptoms of orthostasis and required transfusion of 2 occur in up to 2% of the population and can manifest as units of packed red blood cells. Extensive gastroenterologic obscure gastrointestinal bleeding, Meckel’s diverticulitis, workup included a video-capsule endoscopy which identified obstruction, and intussusception [1]. While most MDs present blood in the ileum. A subsequent double-balloon enteroscopy in childhood, adult patients are also at risk for complications, indicated friable ileal mucosa with contact bleeding reportedly though these tend to decrease with increasing age [2, 3]. 120 cm from the ileocecal valve. A tattoo was placed at the Several characteristics that facilitate identification of a point of interest. A Meckel’s scan was then performed at the Meckel’s diverticulum include location two feet proximal to outside facility and was negative. the ileocecal valve, the presence of an independent vessel No additional intervention was undertaken by the patient supplying the structure, five layers of small intestine, and until two weeks prior to his presentation to our clinic, which ectopic mucosa of either gastric, pancreatic or another origin was one year after his first episode. Upon further questioning other than small intestine in a majority of specimens [4]. the patient had used NSAIDs prior to first episode of There are very few cases of mesenteric-sided MD reported bleeding and aspirin prior to second episode. Workup at our in surgical literature (Table 1), and several authors have institution included computed tomography (CT) scanning suggested that what some call a mesenteric-sided MD may with enterography, as well as a review of the patient’s outside in fact be an intestinal duplication cyst [4–9]. This study capsule endoscopy. CT enterography revealed a “tubular reports a case of what the authors believe to be a mesenteric outpouching” adjacent to the distal ileum and ascending MD and reviews the literature concerning identification and colon that was considered consistent with the expected appropriate treatment of a MD in the minimally invasive era. appearance of a Meckel’s diverticulum (Figure 1). In light of Carpenter et al. 146 Table 1. Cases of mesenteric-sided MD reported in surgical literature. Author & year Segal et al. 2004, [7] Manukyan et al., 2009, [9] Sarioglu-Buke et al., 2008, [5] Seitun et al., 2011, [6] Carpenter et al., 2013 Presentation Procedure performed Distance from ICV OR findings Path findings 19-year-old, M, acute abdominal pain Low transverse RLQ incision, small bowel resection, WLE mesentery 63.5 cm Adenopathy, forshortened mesentery Gastric mucosa w/ metaplasia 15-year-old, F, acute abdominal pain 7-month-old, M 65-year-old, F, RLQ abdominal pain 35-year-old, M, obscure GI bleed Standard laparotomy Laparotomy, small bowel resection and anastomosis Lower midline incision, stapled transverse diverticulectomy Laparoscopic small bowel resection Mesenteric MD 40 cm Mesenteric lymphadenopathy, 2 cm base, wide ileal connection 40 cm Mesenteric abscess RLQ, inflamed MD 60 cm Mesenteric MD Pancreatic, gastric mucosa with chronic ulceration Fibrin accumulation, gastric mucosa Heterotopic gastric mucosa w/ perforation Gastric mucosa M: male; F: female; WLE: wide local excision; RLQ: right lower quadrant; ICV: ileocecal valve; OR: operating room; Path: pathology the enterography results, a Meckel’s scan was repeated and revealed tracer uptake in the right lower quadrant consistent with a Meckel’s diverticulum (Figure 2). With this information, the patient was taken to the operating room where an exploratory laparoscopy with small bowel resection and side-to-side anastomosis was performed. The initial dissection was performed using three 5 mm trochars placed along the lateral left abdominal wall. Upon examination of the small intestine, a diverticulum was noted at approximately 60 cm from the ileocecal junction. However, this was found along the mesenteric border of the ileum (Figure 3). The tattoo indicating the furthest extent of the previous outside institution double balloon enteroscopy was noted to be at least 20 cm distal to the diverticulum (Figure 4). This area was not resected. One of three 5 mm trocars was upsized to a 12 mm in order to permit use of an Endo-GIA stapler (Covidien) which was employed for the transaction of the small bowel and mesentery surrounding the diverticulum (Figure 5). The diverticulum was sent to pathology where gross examination as well as frozen and permanent sections revealed the presence of ectopic gastric mucosa (Figure 6a & b). Final pathology revealed a 7 cm x 2.5 cm pouch-like diverticulum containing a 3.5 cm area of mucosa with a granular appearance as opposed to the tan folds of the surrounding ileum. Microscopically, hematoxylin and eosin staining revealed erosion adjacent to reactive oxyntic gastric type mucosa. Figure 1. CT enterography demonstrating intestinal outpouching consistent with Meckel’s diverticulum. Mesenteric Meckel’s diverticulum 147 [5]. Another explanation is that the vitelline duct would simply adhere to the ileal mesentery [1]. Several other authors presenting cases of mesenteric-sided MD have openly pondered if they may have been dealing with an intestinal duplication cyst rather than a MD [4]. This begs the question of how one might differentiate the two. It seems that the absence of a distinct communication of a structure with adjacent intestinal lumen would favor intestinal cyst or duplication [7]. Our patient had a clear connection between lumens of his MD and the ileum. Another possible area of distinction is with ectopic gastric mucosa, which our patient demonstrated. However, ectopic gastric or pancreatic mucosa can be found in both MD (approximately 55%) and intestinal duplication cysts (approximately 16-39%) [1, 7, 10]. Figure 2. Meckel’s scan with uptake in right lower quadrant. Figure 3. Laparoscopic view identifying Meckel’s diverticulum (arrow) embedded in mesentery. Figure 4. Tattoo (arrow) of previous double-balloon endoscopy. Discussion Several other authors have reported MD presenting on the mesenteric border. Some argue this can only be an intestinal duplication cyst, but a case reported by Kurzbart and colleagues suggests otherwise as contrast was administered to a newborn infant of 28 weeks gestation via a fourth lumen in the transected umbilical cord [5, 7, 8]. Contrast filled the small bowel upon injection. At 3 months of age, the infant underwent an umbilical hernia repair. No residual omphalomesenteric structures were present, however a MD was found 40 cm from the ileocecal junction but adherent to the mesentery [8]. Several explanations for the reported mesenteric locations have been offered including that a shortened vitelline artery could form a mesodiverticular band from the ileal mesentery to the tip of the diverticulum which would then divert the diverticulum away from the antimesenteric border during elongation and fetal growth Figure 5. Resection of small bowel and mesentery surrounding diverticulum using Endo GIA stapler (Covidien). (Arrow: mesenteric staple line) Carpenter et al. 148 a b SIM GFM Figure 6. a) Opened diverticulum. Gastric fundic type mucosa is pink granular mucosa on right; small intestinal mucosa is tan mucosa with folds on left. b) Diverticular mucosa, hematoxylin and eosin, x40. Villi from small intestinal mucosa (thin arrow), erosion at 6 o’clock (short arrow), reactive oxyntic gastric type mucosa (thick arrow) Some authors have asserted that the presence of a vitelline artery or a clear independent blood supply to a diverticulum is definitive evidence of MD whereas intestinal duplications share blood supply with the surrounding intestine [7, 11]. However, Kusumoto and colleagues have indicated that a distinct vitelline artery could be identified in only 10% of 776 patients with MD [12]. In the case here presented, a distinct blood supply was identified on CT scan, but attempts were not made to delineate this vessel intraoperatively or pathologically. In brief, we are left with the conclusions of previous authors that while the behavior and presentation of the lesion were more consistent with MD, we cannot definitively rule out a simple intestinal diverticulum or duplication cyst. References [7] Segal SD, Albrecht DS, Belland KM, Elster EA. Rare mesenteric location of Meckel’s diverticulum, a forgotten entity: a case study aboard USS Kitty Hawk. Am Surg. 2004; 70: 985–988. [8] Kleinman R. Chapter 29. Atlas of Pediatric Gastrointestinal Disease. Hamilton, Ontario, B.C. Decker Inc. 1998; 113. Kurzbart E, Zeitlin M, Feigenbaum D, Zaritzky A, Cohen Z, Mares AJ. Rare spontaneous regression of patent omphalomesenteric duct after birth. Arch Dis Child Fetal Neonatal Ed. 2002; 86: F63. [9] Walczak DA, Falek W, Zakrzewski J. An uncommon location of Meckel’s diverticulum or small intestine duplication? Case report and literature review. Pol Przegl Chir. 2011; 83: 457–460. Manukyan MN, Kebudi A, Midi A. Mesenteric Meckel’s diverticulum: a case report. Acta Chir Belg. 2009; 109: 510–512. [10] Cavar S, Bogovic M, Luetic T, Antabak A, Batinica S. Intestinal duplications--experience in 6 cases. Eur Surg Res. 2006; 38: 329–332. [5] Sarioglu-Buke A, Corduk N, Koltuksuz U, Karabul M, Savran B, Bagci S. An uncommon variant of Meckel’s diverticulum. Can J Surg. 2008; 51: E46–47. [11] Li L, Zhang JZ, Wang YX. Vascular classification for small intestinal duplications: experience with 80 cases. J Pediatr Surg. 1998; 33: 1243–1245. [6] Seitun S, Vito LD, Rossi UG, Panetta M, Cabiddu F, Tedeschi U, Viotti A. Perforated Meckel’s diverticulitis on the mesenteric side: MDCT findings. Abdom Imaging. 2012; 37: 288–291. [12] Kusumoto H, Yoshida M, Takahashi I, Anai H, Maehara Y, Sugimachi K. Complications and diagnosis of Meckel’s diverticulum in 776 patients. Am J Surg. 1992; 164: 382–383. [1] Uppal K, Tubbs RS, Matusz P, Shaffer K, Loukas M. Meckel’s diverticulum: a review. Clin Anat. 2011; 24: 416–422. [2] Soltero MJ, Bill AH. The natural history of Meckel’s Diverticulum and its relation to incidental removal. A study of 202 cases of diseased Meckel’s Diverticulum found in King County, Washington, over a fifteen year period. Am J Surg. 1976; 132: 168–173. [3] [4]