Reports on Progress in Physics 62
advertisement
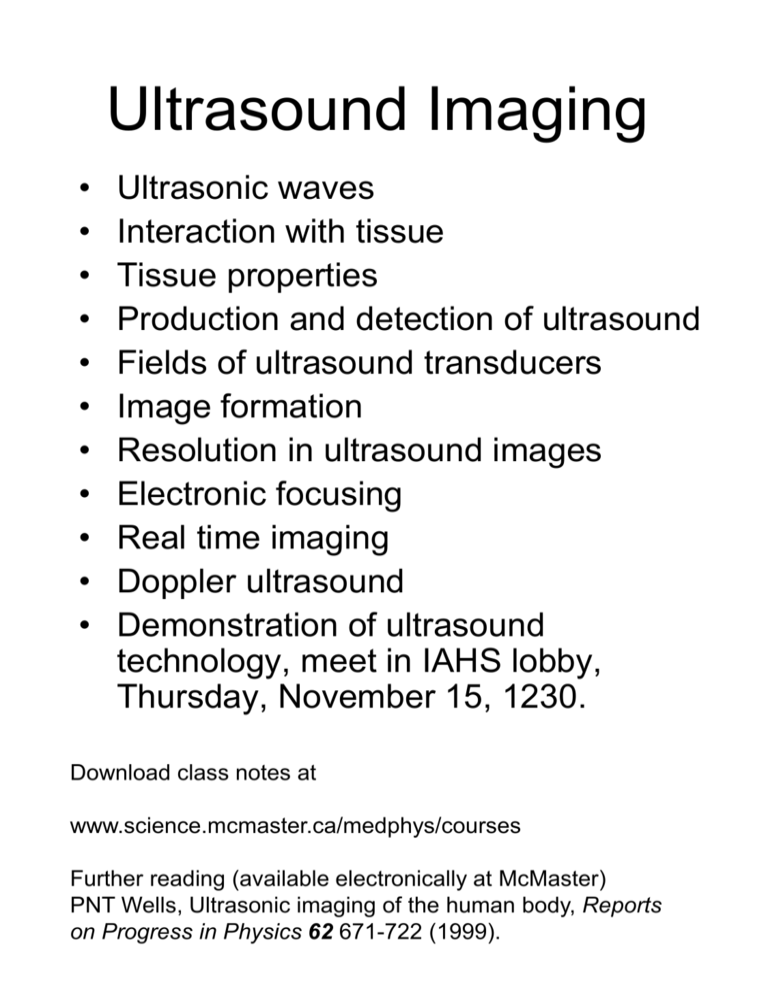
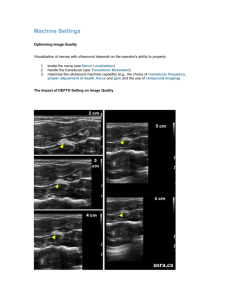
Ultrasound Imaging • • • • • • • • • • • Ultrasonic waves Interaction with tissue Tissue properties Production and detection of ultrasound Fields of ultrasound transducers Image formation Resolution in ultrasound images Electronic focusing Real time imaging Doppler ultrasound Demonstration of ultrasound technology, meet in IAHS lobby, Thursday, November 15, 1230. Download class notes at www.science.mcmaster.ca/medphys/courses Further reading (available electronically at McMaster) PNT Wells, Ultrasonic imaging of the human body, Reports on Progress in Physics 62 671-722 (1999). The Ultrasound Spectrum WAVELENGTH IN WATER 1.5 mm 0.015 mm l f = 1500 ms -1 FREQUENCY 1 GHz In water Ultrasound microscopy 100 MHz 0.15 mm 10 MHz 1.5 mm 1.0 MHz 15 mm 0.1 MHZ Medical imaging Therapeutic applications 0.02 MHz (20 kHz, hearing threshold) Description of Ultrasonic Waves • In general, both compressional and shear waves can propagate in a solid, but soft tissue will support only compressional waves. • While there are minor differences in the velocity of ultrasound in soft tissues, the value 1540 meters per second is assumed in image reconstruction. The variation of velocity with frequency ( i.e. dispersion) can also be ignored. A round trip of 1 cm takes 13 microseconds in tissue. • The product of wavelength and frequency is equal to the wave velocity, so in soft tissue the wavelength of 10 MHz ultrasound is 0.15 mm. The wavelength plays an important part in determining the ultimate resolution that can be achieved with an imaging system. • The energy transported by the wave per unit time per unit area is referred to as the intensity. The usual units are Watts per square centimeter. The average intensity in diagnostic applications is below 100 mW cm -2, but the peak intensity can be much higher. Propagation of Ultrasonic Waves Absorption This occurs even when the wave propagates in a homogeneous medium such as a tank of water. For simple fluids, the main mechanism is viscous loss. For complex media, such as tissue. “relaxation processes” in which acoustic energy is coupled to changes in molecular conformation are important. Both mechanisms are dependent on frequency - viscous losses vary as f2 and relaxation losses somewhere between linear and quadratic dependence. Scattering Scattering of the ultrasonic wave does not take place unless the wave encounters a change in acoustic impedance. For our purposes, the acoustic impedance is Z = ρc where ρ is the density and c is the speed of sound. For water Z is 1.48 X 106 kg m-2 s -1 and most soft tissues are within a ten per cent of this value. Note that the acoustic impedance of compact bone (e.g. the skull) is about five times higher and that of air is lower by a factor of 3,700. The physical process of scattering depends in a complex way on the size of the inhomogeneity and its acoustic impedance relative to the surrounding medium.In general, the fraction of incident energy scattered by the inhomogeneity will increase with both of these quantities. Two special cases for scattering #1 Object much smaller than the wavelength A classic example is scattering by a single red blood cell, of diameter about 10 microns. In this regime the scattering is approximately the same in all directions, and the scattering cross-section is proportional to f4. This is analogous to Rayleigh scattering of light by small particles. #2 Large object with a “smooth” boundary In this case the incident wave is reflected and refracted at the surface analogous to the behavior of a light wave at a discontinuity in refractive index. θ θ Specular reflection Z1 Z2 φ For the simple case of normal incidence the intensity reflection coefficient is R = [(Z2 - Z1)/(Z2 + Z1)]2 Implications of Specular Reflection Consider a soft tissue/bone interface. The intensity reflection coefficient is (7.80 - 1.63)2 / (7.80 + 1.63)2 = 0.42. In other words, the transmission is 58%. This means that if we were trying to use ultrasound to image the brain, we would only get 33% of the incident intensity into the brain, and only 33% of the scattered intensity out of the brain. 100% SKIN This is one reason that ultrasound is not used 58% to image the adult brain, 33% but it is used in infants where the skull is not BRAIN yet calcified. The reflection coefficient at gas/tissue SKULL interfaces is even larger, so ultrasound is not useful in imaging the lung. This also explains why a coupling gel is used during ultrasound exams. The gel fills the space between the transducer and the skin and prevents reflection by trapped air. TRANSDUCER SKIN COUPLING GEL Attenuation Together, absorption and scattering result in attenuation of the ultrasound wave. The intensity falls off exponentially with distance. We could express this as exp (-μx) using a linear attenuation coefficient μ, but with ultrasound it is conventional to express the attenuation coefficient in dB cm-1. Digression on the decibel The decibel scale is a way to represent the ratio of two intensities. If the two intensities are I1 and I2, we can express the ratio as dB ratio = 10 log10 (I1 / I2) so if the attenuation coefficient is, for example, 1 dB cm-1, after transmission through 10 cm of tissue the intensity will be reduced by 10 dB, or a factor of 10. After 20 cm it would be reduced by 20 dB or a factor of 100. Frequency dependence The attenuation coefficient is a function of ultrasound frequency. As shown on the next diagram, the coefficient is roughly proportional to frequency for a variety of tissues. In fact, a good rule-of-thumb is that the attenuation coefficient for soft tissue is 1 dB cm-1 MHz-1. Note the implications: at 1 MHz, transmission through 10 cm of tissue reduces intensity by a factor of 10, but at 10 MHz, transmission through 10 cm of tissue reduces intensity by a factor of 10,000,000,000! This frequency-dependent attenuation imposes limits on the performance of imaging systems. Generation and detection of ultrasound Both rely on the piezoelectric effect, first discovered in the late 1800’s. Certain natural crystals (e.g. quartz) undergo a change in physical size when an electric field is imposed on the crystal. + - This change can launch an acoustic wave in the surrounding medium. These materials also demonstrate a reciprocal piezoelectric effect: a voltage is generated across the crystal which is proportional to the applied pressure. This pressure can result from an acoustic wave incident on the crystal. The resulting voltage can be detected and amplified, so we have a means of detecting acoustic waves as well as generating them. In medical applications, the same “transducer” is used to generate acoustic waves and to detect the waves scattered by tissue. Synthetic materials demonstrate a much more efficient conversion of electrical to acoustic energy. Most medical transducers are fabricated from a ceramic material: lead zirconate titanate, or PZT. A transducer has a natural resonant frequency corresponding to a wavelength (in the material) that is twice the transducer thickness. For PZT, a 1 mm thick transducer resonates at 2 MHz. While resonance contributes to efficient energy conversion, it may be detrimental in other ways. POWER PRESSURE Most ultrasound imaging is based on the localization of “echoes” or scattered waves from structures within the tissue. Intuitively, we would expect that it is easier to figure out where a short pulse came from because longer pulses would lead to temporal overlap in the echoes and greater ambiguity about their source. Hence it is generally desirable for the source to emit a short pulse, but this is not what we get from a resonating transducer: TIME FREQUENCY PRESSURE POWER The emitted pulse lasts a long time and looks like a pure “tone”. This corresponds to a narrow frequency spectrum. If the transducer is “damped” so that it does not resonate, the pulse is much shorter, and the spectrum is correspondingly broad. TIME BANDWIDTH FREQUENCY This diagram shows a single element transducer with electrical connections and mechanical damping. Note also the matching layer. This is fabricated of material with an acoustic impedance between that of the PZT crystal (very high) and tissue. Its thickness is one quarter wavelength. It can be shown that this maximizes power transfer from the PZT to the tissue in the same way anti-reflective coatings work on glasses and other optics. Note also, that the PZT crystal is shaped like a spherical shell. This results in a focussed wave. Similar results could be achieved with an acoustic lens As discussed later, single element transducers are no longer used in medical imaging. Multi-element arrays offer potential for electronic focussing and real-time imaging. Acoustic fields of ultrasonic transducers A very small transducer (compared to the ultrasound wavelength) would act like a point source (and detector). This would be useless for imaging because we would not be able to direct the ultrasound pulse to a specific region, nor would we be able to tell which direction echoes were coming from. Let’s consider a larger transducer as shown below. We can conceptually divide the transducer into many small elements, all vibrating in phase. Each emits a spherical wave, but at some arbitrary point in the tissue, these waves do not arrive in phase because the distance to each element is different. In order to calculate the resulting field we must consider the possibility of interference and sum all of the waves taking into account their relative phase. This is exactly what you do to calculate the diffraction pattern from a single slit in optics, and the same sort of integral appears in the acoustic problem. AXIS OF SYMMETRY P This diagram shows the amplitude of the pressure field when the disk transducer vibrates at a single frequency. Close to the transducer in the “near field” there is a complex interference pattern. In the “far field” we see a well-defined peak on the axis of the transducer. The peak broadens and decreases in size as we move farther from the transducer. Mathematically, we can show that the amplitude of the acoustic pressure wave is proportional to 2 J1 (k a sin θ) where k = 2π/λ k a sin θ J1 is first order Bessel function We can do the same calculation for a focused transducer with the geometry shown below: Focal plane P a r z In the focal plane the pressure amplitude is proportional to 2 J1 (kr / 2f) (kr / 2f) where f = z / 2a is called the f - number or f# Note that the amplitude peak becomes narrower as we decrease λ (i.e. increase frequency) or as we decrease the f - number. If the transducer emits a pulse (as it usually does) rather than a continuous wave, the calculation is more complex because the pulse contains energy at many frequencies. The general features of the field are the same if we consider the frequency to correspond to the average of the power spectrum. The sharp maxima and minima of the interference pattern are not so evident for pulsed excitation. Note that a focused transducer can be used as a detector and that it will have the same directional sensitivity. …..so enough physics, how do you make images? To obtain a complete image it is necessary to a “fill in the box” by getting sufficient A scans. In the early days of ultrasound imaging this was accomplished by moving a single element transducer over the surface of the patient. Before considering modern methods, it is instructive to examine the resolution attainable with the older method. Typical ultrasound image – note the high resolution at 12 MHz, the “speckle” in the image, and the characteristic appearance of the cyst in the thyroid gland. Image courtesy of GE Healthcare Resolution in Ultrasound Images Axial direction Consider the case of a rectilinear scan where parallel A scans are obtained by translation of the transducer. Lateral direction The axial resolution is determined by the pulse length. This is why it is important to have well-designed wide-band transducers that emit a short pulse. Typical values of axial resolution are 1 mm or less. The lateral resolution depends on the focusing properties of the transducer. It can be improved by increasing the frequency or by decreasing the f#. The first option is limited by the clinical requirements for penetration. In general, systems use the highest frequency possible. For a small organ like the thyroid, a higher frequency can be used than is possible with a large organ like the liver. The second option is limited by the fact that stronger focusing (i.e. lower f#) will result in a reduced “depth-of-field”. This means that lateral resolution is rapidly degraded at depths out of the focal plane. Schematic illustration of the depth-of-field problem Low f-number transducer Focal plane High f-number transducer Electronic focusing The depth-of-field problem can be overcome to some extent by focusing the transducer at different depths for different parts of the image. The concept is illustrated below: Electronic focusing can be achieved with annular arrays or with linear arrays of transducer elements. A lens can be used with a linear array to provide some (fixed) focusing in the plane perpendicular to the array. Real time ultrasound imaging A major advantage of modern systems is the ability to acquire images in “real time”. Practically, this means that an image must be obtained in a time comparable to persistence of human vision. This requires about 30 images (or frames) per second. For a frame rate F, there is a relationship between the number of A scans in the image, L, and the maximum depth to be imaged, d. In order to avoid ambiguity in echo location we require 1/F = 2 L d/c where c is sound velocity Clearly it is not possible to translate a transducer quickly enough to get real time images. Early scanners overcame this problem by using a rotating or rocking scanner: Surface Shaded area is the imaged region. Because of its shape, this is sometimes called a sector scan. Another way to do this would be to have an array of transducer excited sequentially, so that each is used to get an A scan. The problem with this approach is that a single element has very poor lateral resolution. This can be overcome by using groups of array elements to steer and focus the beam as shown below: The implementation of these ideas requires sophisticated electronics and fabrication techniques. Advances in these technologies have allowed real time systems to become small, portable, and cheap compared to other imaging methods. Doppler ultrasound The Doppler shift is a familiar phenomenon at audible frequencies. The same thing happens when ultrasound is scattered by a moving object such as a red blood cell. Note: the factor of two appears in the equation because the moving object “hears” a Doppler shift, as does the observer of the scattered ultrasound. For typical blood velocities and ultrasound frequencies, the Doppler shift is in the kHz regime. In simple systems, this can be presented to the operator as an audible signal. POWER Large signal from stationary objects Blood moving away from the transducer Weak Doppler signals due to blood moving towards the transducer FREQUENCY The Doppler signal must be found in the “clutter” of signals from stationary objects. This is one case where a narrow-band or cw system is advantageous. One problem with such a system is that it provides no depth resolution so it may be difficult to localize the blood flow information. This is overcome in pulsed Doppler systems that determine the Doppler shift as a function of depth. Color flow imaging Blood vessel Consider the two signals above, acquired a short time apart without moving the transducer. As expected, the signal from stationary tissue is unchanged, but the signal from the blood vessel has changed because a different arrangement of scatterers fills the volume that contributes to the signal. The faster blood is flowing, the greater the difference in the signals. The “difference” can be mathematically quantified as a correlation, and there is a relationship between this and the blood flow velocity. This information can be obtained everywhere in the image and overlaid as a color on the normal gray scale image. Red and blue are used to code for direction of flow and the brightness of the color is used to indicate velocity. Example (from GE’s clinical image library) of color Doppler study of carotid stenosis. Instead of imaging flow velocity, another mode is “power Doppler” where the integral of the power spectrum is displayed. This increases sensitivity and allows imaging of organ perfusion For example, this image (courtesy of GE) shows renal perfusion.