Department of Health Department of Health Enhancing clinical skills
Simulated Learning Environments
Program
Final report
Enhancing clinical skills and collaborative working:
Developing an interprofessional simulated learning space
Submitted by:
Monash University
September, 2013
Department of Health
Definitions
For the purpose of the report, please use the definitions and explanations below:
Simulation
Learning methods provided in Simulated Learning Environments which support experiential learning. Key components of experiential learning include:
•
The learner interacts with a simulated or controlled real environment;
•
A high proportion of the learning activities enact activities and tasks representative of the learner’s real world responsibilities;
•
The environment needs to be sufficiently realistic for experiential learning to occur. Depending upon the learning objectives, realism can be built into the equipment, the surrounding environment or the overall integration of equipment, environment and interactions between learners and instructors.
Students
Students are participants in eligible simulation programs which may include professional entry-level courses, postgraduate and VET sector courses and ongoing professional development.
Total number of simulation education hours
The total number of simulation education hours is reported over the life of the project for the purposes of measuring the baseline and growth of simulation activity across all projects covered by this funding agreement.
The calculation for counting the total number of simulation education hours is as follows:
Calculation: As an example, if a simulation course, workshop or other form of simulation education program runs for a duration of eight hours and there are ten participants/students, the total number of simulation hours for that course or workshop is 80. All courses, workshops or other forms of simulation education programs delivered through the project during the period to which this report relates, should be included in this calculation of total number of simulation education hours.
Please calculate the growth in simulation education hours for the project using the baseline simulation education hours previously reported.
Rural and remote
For the purpose of these reports, use the AGSC RA (Remote Area Classifications) used by the Department of
Health and Ageing.
RA1
RA2
RA3
RA4
RA5
Major Cities of Australia
Inner Regional Australia
Outer Regional Australia
Remote Australia
Very Remote Australia
RA2 and RA3 are rural and are in scope for this report. RA4 and RA5 are remote and are in scope for this report.
The definitions can be found at: www.health.gov.au/internet/otd/publishing.nsf/content/ra-intro
To find the classification for a specific locality, click on the above link and select ‘What is the RA classification of my locality?’ Click on the available link and enter the postcode for the locality.
Interprofessional learning
Interprofessional education occurs when students from two or more professions learn about, from and with each other to enable effective collaboration and improve health outcome.
Page 2 Department of Health
Executive summary
The ability to work effectively as part of an interprofessional team is a key learning outcome of nursing and health science courses within the Faculty of Medicine, Nursing and Health Sciences at Monash University.
This project entitled ‘Enhancing clinical skills and collaborative working: developing an interprofessional simulated learning space ’ is a collaborative initiative between the School of Nursing and Midwifery, Department of Physiotherapy, and Department Community Emergency Health and Paramedic Practice.
The aim of the project was to increase student capacity, improve professional development opportunities and enhance interprofessional learning for health professional groups in the Mornington Peninsula Clinical
Placement Network (CPN). The project objectives were as follows:
•
Adapting existing facilities in-line with best practice teaching and recent professional accreditation guidance;
•
Develop interprofessional learning opportunities and scenarios; and
•
Conduct six instructor courses on simulated learning techniques.
The project activities to achieve the objectives were the recruitment of staff, development and implementation of interprofessional learning scenarios; train-the-train sessions and evaluation of the project.
Project outcomes demonstrated 553 hours in interprofessional simulation learning and 1521 hours of profession-specific simulation hours. In addition to learning technical skills, resuscitation technique and interdisciplinary management of the acutely unwell patient in acute care, participants were exposed to interprofessional sessions requiring demonstration of complex communication skills, teamwork capabilities and handover techniques.
Overall the project has been successful particularly in the way the different disciplines have been able to combine their expertise to develop meaningful interprofessional simulation learning experiences. Following the completion of the project the next steps are:
•
Continue to embed interprofessional simulation learning within curricula,
•
To improve the interprofessional learning access of industry partner in the Mornington Peninsula region,
•
Further provision of training sessions in the use and deliver of interprofessional simulation; and
•
Collaborative planning with Mornington Peninsula CPN to increase Simulated Learning Environment (SLE) capacity in the region creating affordable and innovative resources with good governance structures.
Background and context
The Monash University School of Nursing and Midwifery, Department of Physiotherapy and Department of
Community Emergency Health and Paramedic Practice (a partnership named as ‘NPP’) were funded in 2012 to deliver on the proposal ‘Enhancing clinical skills and collaborative working: developing an interprofessional simulated learning space ’. The subsequent funded project has been delivered as part of the National and
Victorian State response to expand clinical training capacity through simulated learning initiatives for students undertaking professional-entry programs of study. The Mornington Peninsula CPN was a key stakeholder in the project providing a regional link to health care and education providers with interests in the project outcomes.
The project was delivered in two parts. The first involved capital works to expand existing simulation facilities in the School of Nursing at Peninsula Campus (Frankston). The capital works and fit-out were completed in
November 2012 and has provided the NPP with a four bed medium fidelity clinical simulation area, an observation room and debriefing room which includes audiovisual equipment for recording and reviewing clinical cases, and additional equipment storage space. While this part of the project has been delivered successfully there have been issues in regards to tight project timelines, planning and implementing capital works and supply of equipment which delayed the implementation components within the second part of the project. However, all project objectives have been met at the time of this final report.
Page 3 Department of Health
Lessons to be learned from the capital works are as follows:
•
Project timelines need to take into account negotiations and contract signage for capital works which are completed after the signing of the head agreement;
•
Simulation and audiovisual equipment are constantly being improved and upgraded and there needs to be sufficient flexibility in the purchasing of equipment during the project timelines;
•
Sufficient time for installation and testing of the equipment needs to be built into project timelines. Suppliers of simulation equipment belong to a niche and resource limited market. Demands on same suppliers by projects within the same round of funding led to delays in the supply issues of critical pieces of equipment. In addition, testing of equipment demonstrated faults in overall equipment function which led to further delays.
Software did not have full capability and there have been ongoing technical issues during the operational rollout of the new facilities. Training by suppliers was restricted to basic functionality of equipment with more in-depth training offered as an additional cost; and
•
Project management has evolved as a hidden cost in the project and needs to be clearly identified and funded as a component of a simulation capital works project.
The second part of the project focused on the commissioning and operational rollout of educational activities within the new simulation facilities. Specifically, this project has been positioned within the Monash University
Faculty of Medicine, Nursing and Health Sciences Faculty Simulation Plan which was developed to support the objectives of the Victorian SLE Strategic Plan (2011). While the capital works were in progress curricula planning with the NPP project management group commenced with a focus on expanding interprofessional learning (IPL) across the disciplines of nursing, paramedicine and physiotherapy. As a starting point and based on existing evidence NPP reviewed IPL episodes of learning which were relevant to all participant curricula. In addition to the more traditional simulation scenarios involving critical incident management, the NPP have worked to develop and implement a range of clinical reasoning scenarios reflective of issues of complex issues in clinical practice. The remainder of this report is focused on the outcomes of the second part of the project which was supported by the fixed term funding completed by June 2013.
Project objectives and expected impacts
The overall objectives of the project were to increase student capacity, improve professional development opportunities and enhance interprofessional learning for health professional groups in the Mornington Peninsula
CPN. The fixed term project had three specific objectives:
•
Adapting existing facilities in-line with best practice teaching and recent professional accreditation guidance,
•
Develop interprofessional learning opportunities and scenarios,
•
Conduct six instructor courses on simulated learning techniques.
The anticipated impacts were:
•
An increased entry-level capacity by recruiting additional students to undergraduate programs;
•
Enhanced clinical induction and learning, through increased utilisation of SLE;
•
Optimisation of clinical training experiences with contemporary facilities, equipment, manikins and simulation techniques;
•
Enhanced collaborative working with professional partners and health service providers to ensure that clinical skills facilities are utilised to their maximum capacity;
•
Development of interprofessional learning opportunities/scenarios and instructor courses in SLE techniques; and
•
Enhancement of interprofessional teaching capacity for educators and clinical supervisors in the region.
Page 4 Department of Health
Project management
The following outlines the overall project management framework for this project.
Governance
A Project Management Committee was convened at the commencement of the project and has met regularly to oversee the project activities and deliverables. Representatives from key stakeholders from nursing, physiotherapy and paramedicine formed the Committee. A key requirement of representatives was an ability to demonstrate expertise in education, simulation and interprofessional learning. The role of the Project
Management Committee was to share expertise and provide advice on all aspects of the project inclusive of development of the learning environment, implementation and maintenance of education activities located within the new learning space. In particular, the Committee provided advice, support and active expertise in relation to:
•
Advise and feedback on discipline-specific input into education needs and interprofessional expansion options relevant to functions of the new simulation area;
•
The identification and preparation of project simulation education activities to be integrated within curricula requirements in-line with best practice teaching and professional accreditation requirements;
•
The provision of timely information and feedback to enable the project to meet all project reporting and deliverables;
•
Advise on potential risks associated with the project and implementation of strategies to mitigate identified risk; and
•
Advise and implement project evaluation and research initiatives relevant to the project.
The Project Management Committee reported through its representatives to the appropriate School Executive and the Faculty Health Workforce Australia (HWA) Coordinating Committee.
Staffing
In order to deliver on the learning and development project plan, an Academic Lecturer B Interprofessional
Simulation Learning Project was appointed in January 2013. The position had particular requirements to fit with the Monash University requirements for academic appointments and the specific staffing support needs for the project. The timing of the appointment was delayed until January 2013 due to project issues.
To facilitate the development of the position, resources on the HWA SimNet online portal for simulation education and training resources were used (www.simnet.net.au). As a result the project appointed a flexible highly skilled staff member with ability to work across disciplines who has been a key enabler of the ability of the project to meet the project key performance indicator requirements. The staff member has reported to the
Project Lead and worked collaboratively with the Project Management Committee to coordinate the simulation sessions, provide technical and troubleshooting expertise, contribute to the development of educational material as required and implement orientation programs as well as the evaluation plan.
Stakeholder engagement and consultations
To deliver on this project the following external and internal stakeholders were engaged through a range of communication channels:
External
•
Department of Health
–
Attendance at workshops provided by the Department to support the project, regular emails, progress reports and final report.
•
Risk mitigation
–
To ensure consistency regarding the expectations of project outputs and outcomes and that reporting requirements were met.
Page 5 Department of Health
•
Mornington Peninsula CPN
–
The CPN Coordinator met regularly with the Project Lead to link the project into the overall CPN program of work. In addition, information was provided for the local CPN bulletin regarding project progress which was disseminated to the Mornington Peninsula external health services and education stakeholders. In addition, the Project Lead attended CPN meetings to provide an update on the project progress and outcomes.
•
Risk mitigation
–
To integrate CPN expectations within the project and provide a mechanism for feedback and engagement.
•
Mornington Peninsula health services providers
–
Verbal updates were provided through existing clinical placement channels for nursing, paramedicine and physiotherapy.
•
Risk mitigation
–
To provide communication regarding the development of education curricula and its relevance to 2013 and 2014 clinical placement requirements.
Internal
•
Faculty HWA Project Coordinating Committee
–
Verbal updates were provided to the Faculty Committee at the regular three-monthly meetings.
•
Risk mitigation
–
To ensure a key Faculty leadership group was appropriately briefed on cross discipline educational simulation activities.
•
School of Nursing and Midwifery, Department of Community Emergency Health and Paramedic Practice,
Department of Physiotherapy
–
Representatives from the project management group provided feedback to the relevant school and department staff through discipline emails, briefings and executive reports and verbal feedback at staff meetings.
•
Risk mitigation
–
Lack of engagement from partner disciplines would impede project progress.
•
Academic staff
–
Email communication regarding simulation training nursing, paramedicine, physiotherapy.
•
Risk mitigation
–
To provide sufficient notice for academics to attend training in key areas of simulation education and to encourage engagement in the use of the facilities.
•
Professional staff
–
Agenda item on the regular Clinical learning Environment Group meeting.
•
Risk mitigation
–
To ensure professional staff providing cross campus support for clinical learning are appropriately briefed and engaged regarding the project activities as a key enabling group of simulation education.
Budget
Financial management of the project was achieved through the establishment of a separate budget line item. All expenditure for the project has come directly from the established fund code and all costs associated with the project have been committed as spent as of 30 June 2013. Budget progress and expenditure was tracked and reviewed by the Project Lead and overseen by the Faculty Accounts Manager.
Page 6 Department of Health
Timelines
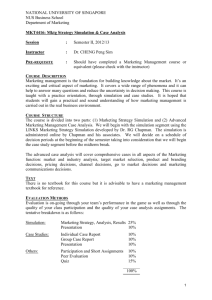
Activity
Recruitment of the Lecturer Interprofessional Simulation
Learning Project
Implementation of simulation education hours in semester 1
Writing interprofessional clinical simulations
Evaluation and its application to teaching and learning
Planned start date
January 2013
February 2013
November 2012
February 2013
Planned completion date
January 2013
June 2013
June 2013
June 2013
Project activities and methodology – performance against stated deliverables
Project activities
Project activity
Education of staff
Evaluation of project includes educators, students and industry partners
Project deliverable Due date Achieved / not achieved
Six train-the-trainer sessions
June 2012 – June 2013 Achieved: While planning was underway in
2012, the delay in the commencement of the project meant that this could not be completed until June 2013.
Phase 1: Questionnaire
Phase 2: Focus groups
January
– March 2013
April – June 2013
Achieved: Simulation sessions for staff and students have been followed by evaluation questionnaires specific to the type of sessions.
Focus groups were not performed as the project was not mature enough for this activity.
Project outcomes and discussion
The NPP had expectations that the interprofessional project would contribute to improved assessment, clinical decision making and teamwork skills for both undergraduate and postgraduate students and other health professionals in the Mornington Peninsula region. There were three key elements to the project:
•
Planning and development of interprofessional scenarios which were appropriate to nursing, physiotherapy and paramedicine;
•
Recruitment of project implementation support staff to ensure the technical and educational support was available; and
•
Implementation of interprofessional simulation education in a new simulation facility with a focus on students undertaking professional-entry courses and the training of staff to effectively plan and conduct scenarios.
The ability of the project to deliver on the objectives was greatly influenced by the following factors:
Objective 1: Adapting existing facilities in-line with best practice teaching and recent professional accreditation guidance.
Influencing factors and delivery
The representatives from each discipline comprising the NPP have a range of andragogical expertise teaching across the nursing, midwifery, allied health and paramedic curricula with specific foci on the development of safe clinical expertise. In addition, the NPP project team had extensive practical expertise in simulation education, both in developing and delivery of simulation training and its relationship to clinical practice. This background and mix of personnel was critical to the success of the project as timelines were very tight and meant that much could be achieved in a short space of time.
Page 7 Department of Health
Objective 2: Develop interprofessional learning opportunities and scenarios.
Influencing factors and delivery
The project was able to demonstrate over 2074 simulation education hours to professional-entry students and of these hours 553 hours were in the interprofessional context. The student target groups for this project came from three of the eligible professional-entry groups identified by HWA, namely nursing, paramedicine and physiotherapy. Second and third-year students from the Bachelor of Nursing, Bachelor of Physiotherapy and
Bachelor of Nursing Bachelor of Emergency Health (Paramedic) were specifically targeted prior to their clinical placements.
The decision to adapt existing IPL episodes of learning from profession-specific curricula decreased the amount of time for scenario development and also meant that scenarios were within the requirements of the accredited curricula discipline specific resources. As a result implementation of learning activities commenced in the first semester of 2013. To encourage discipline engagement it was also necessary to allow for profession-specific simulation scenarios to be conducted.
The setting for the interprofessional simulation activities was acute care. For the professions involved and the available setting the focus of simulation interprofessional activities could have been limited to crisis resource management (scenarios on interprofessional learning of resuscitation technique and interdisciplinary management of the acutely unwell ward patient were conducted for nursing and physiotherapy students about to go on clinical placement). The NPP however, found additional areas of focus for interprofessional learning and practice which demonstrated an increase in the flexibility and adaptability of the learning scenarios delivered in an acute setting simulation environment. These were sessions relating to communications with palliative care patients, clinical assessment linked to clinical decision making in complex care situations and teamwork (360 hours), handover techniques (paramedics and nurses working in emergency departments, and combining a tutorial on handover communication with a manikin simulation scenario for ‘English as a second language ’ students) and managing delirium patients in an acute care environment. An added value of the delirium workshops was the engagement of medical students. Scenarios related to the patient with delirium in acute care were conducted with third-year nursing and medicine students (twenty-four, three-hour workshops).
An opportunity arose in nursing to deliver a simulation session in palliative care combining student nurses and postgraduate nurses. A total of thirty simulation hours were delivered where using video recording and role-play to demonstrate and engage learning of exemplary practice in palliative care.
While communications with industry partners has occurred, the opportunities to engage in interprofessional activities has not yet occurred due to delays in the commencement of the project and up-skilling timelines for staff. Further work will be done during the sustainability of the project to ensure that health services in the
Mornington Peninsula region have opportunities to access and engage in interprofessional simulation learning.
Objective 3: Conduct six instructor courses on simulated learning techniques.
Influencing factors and delivery
Taking the time to develop a position description relevant to the specific needs of this project led to the appropriate recruitment of the simulation and evaluation support required for the project.
While staff had knowledge of simulation their experience in case-based learning and scenario-based learning was diverse. As a result training focused on developing consistency in simulation education and setting baseline parameters. This had the added benefit of using staff training as a change management technique to encourage the uptake of interprofessional simulation.
In order to meet the learning requirements of staff a range of learning approaches were used to meet the objectives. The first were two train-the-trainer days (eighteen participants by eight hours and twelve participants by six hours) which focused on how to develop learning scenarios, debriefing of students and providing feedback. The other training focus was technical training on the use of simulation equipment as the setting provided medium fidelity equipment in a four-bed acute care environment. Technical training has been provided in small groups and one-on-one but requires follow-up as issues with equipment functionality during the rollout has meant that the software has not yet met its full capacity.
Page 8 Department of Health
In planning the training of staff in simulation learning techniques, the project drew on other current and previously funded initiatives. Linkages were made with Southern Metropolitan CPN to provide expertise into the introduction of teaching and learning in simulation environments. Staff were encouraged to undertake the national NHET-Sim learning modules. The 2007 clinical skills resources developed by St Vincent’s (Melbourne) and commissioned by the Victorian State Government were also used to develop the baseline skills and while references require updating the principles in the modules were found to be applicable to simulation education in
2013.
Sustainability
A major advantage to this project has been that Monash University employs lecturers, technicians, and administrative staff who will now ensure the viability and sustainability of project outcomes beyond the limits of this project. The interprofessional staff links developed during the project has enhanced communications across disciplines and discussions and activities in the latter part of 2013 and beyond are already well underway. The
IPL learning opportunities have led to significant collaborative interprofessional activities which have extended to include medicine.
Plans have been put into place for additional train-the-trainer education programs. These will be extended to clinical educators in industry going forward to ensure that all educators have the expertise to manage SLE for the long-term. Key sustainability activities for the project are:
•
The embedding of the interprofessional learning activities into curricula;
•
Embedding of activities into budget allocation for 2014;
•
Enhancement of collaborative relationships with Mornington Peninsula health services to provide access and support regarding the interprofessional learning scenarios. Cost recovery model limited to consumables; and
•
Continue to work collaboratively with the Mornington Peninsula CPN.
Ongoing sustainability
Simulation activity
Simulation hours provided January
– June 2013
Estimated simulation hours
July
– December
2013
Interprofessional entry-to-practice
553 553
Estimated simulation hours January
– June
2014
Rationale for change to activity level
700
Professional entry-to-practice
1521
Postgraduate 30
Industry 0
1000
30
15
1500
30
30
Embedding of activities into curricula. Gradual uptake to ensure success.
Maintained to review capacity for increase in interprofessional activity.
Maintained to review capacity for increase in interprofessional activity.
Based on interest and gradual uptake.
Limitations and solutions
Below is some of the project challenges encountered:
•
Successful engagement of interprofessional learning requires significant input into cross discipline coordination and timetable issues. Gradual implementation of interprofessional activities, regular meetings and forward planning with NPP are assisting with overcoming some of these issues.
•
Lack of ownership and engagement by academic staff is being addressed by ensuring that there are ongoing staff development sessions in using simulation equipment and teaching in a simulation environment.
•
Issues with student access to streaming and viewing simulation activities due to software limitation. Work is in progress to provide students with portable access of viewing outside of the debriefing and feedback sessions.
Page 9 Department of Health
Evaluation
Evaluation of the project was conducted throughout the project lifecycle. The overall aim of the evaluation was to synthesise data collected during the content development and implementation of the project. The NPP project team focused on the outcomes of the project in-line with the project objectives and impact. The evaluation pro cess was aligned with Kirkpatrick’s (1967) hierarchy of impact covering individual, team and community impact implementation of feedback mechanisms has meant that outcomes have been are fed back to the project team and SLE staff. This has been of particular importance to the positioning and review of simulation learning within curricula.
The evaluation was designed and conducted in three parts. The first stage was the preparation of content. Audit and analysis of curricula content suitable for the project was conducted across the three participating disciplines. Key outcomes from the analysis demonstrated that in order for the simulation learning scenarios to be successful learning objectives should be clearly documented and have applicability to the specific target groups, scenario outlines should be clear and straightforward with sufficient opportunities for participant engagement and simulation resources should be clearly identified. In addition and of equal importance is the need to provide sufficient time for debriefing and feedback into the simulation learning experience.
The second part of the evaluation was focused on participant feedback of simulated learning. This was achieved through participant questionnaires (using a Likert scale and questions relating to self-assessment, applicability to clinical skill development and ability to prioritise care) and requested staff feedback in relation to specific simulation learning scenarios.
Staff positively evaluated their role in the development and implementation of simulation but special acknowledgement was made for the successes of:
•
Combining a tutorial on handover communication with a manikin simulation scenario for ‘English as a second language ’ students;
•
Using live video role-play to model communication in palliative care.
In relation to participant experiences of interprofessional the learning of technical skills was highly rated, however the ability to communicate, discuss and deliver information in a concise and effective manner demonstrates an unders tanding of own and others’ roles that improves patient outcomes is also highly regarded by participants.
The identification of these factors has led to the formulation of a pilot study focused on interprofessional communication in a patient handover context. The following are some sample data collected from the yet to be completed pilot study:
•
A total of nine paramedic and nursing students have completed an interdisciplinary pre-hospital simulation scenario.
•
The following is a brief sample of their responses to selected items graded using a five-point Likert scale:
–
The simulation allowed me to prioritise my assessment and care/treatment – most either strongly agreed
(n=5) or agreed (n=2) with this statement.
–
The simulation allowed me to analyse my own behaviour and actions – most either strongly agreed (n=6,
66%) or agreed (n=2, 22%) with this statement.
–
The scenario resembled a real-life situation actions – most either strongly agreed (n=5, 55%) or agreed
(n=3, 33%) with this statement.
–
Real-life factors and situations were built into the scenario – most either strongly agreed (n=3, 33%) or agreed (n=3, 33%) with this statement.
Responses from the simulation workshop for students with ‘English as a second language’ were also insightful regarding the usefulness of practicing handover techniques in an acute simulation setting; examples are as follows:
“The workshop provides us an opportunity to learn about the handover section, which is a big challenge for international students.”
Page 10 Department of Health
“It was good to observe a situation where I may get in real medical environment so that I could get ideas of how to man age that situation of handover.”
“The demonstration of the scenario is close to realistic and the presentation of handover is useful too.”
The evaluation of the ongoing simulation activities will continue and has now been embedded into the overall review of curricula inclusive of feedback from clinical educators regarding the student performance in the clinical setting. The outcomes of the evaluation are also feeding into research in an effort to build on the body of knowledge for interprofessional simulation learning.
Future directions
Future directions for this project are as follows:
•
Improve access through existing interprofessional and industry partner relationships and through the NPP;
•
Further development of whilst the development of instructor courses;
•
Collaborative planning with Mornington Peninsula CPN to increase SLE capacity in the region creating affordable and innovative resources with good governance structures;
•
Collaborate with Southern Metropolitan CPN and Australia Centre for Health Innovation in relation to further funding opportunities to sustain and expand SLE programs.
Conclusion
Overall the project has achieved its objectives and had many added value interprofessional teaching and learning successes.
Page 11 Department of Health