Rheumatology 4 – Synovial Joints and Osteoarthritis
advertisement
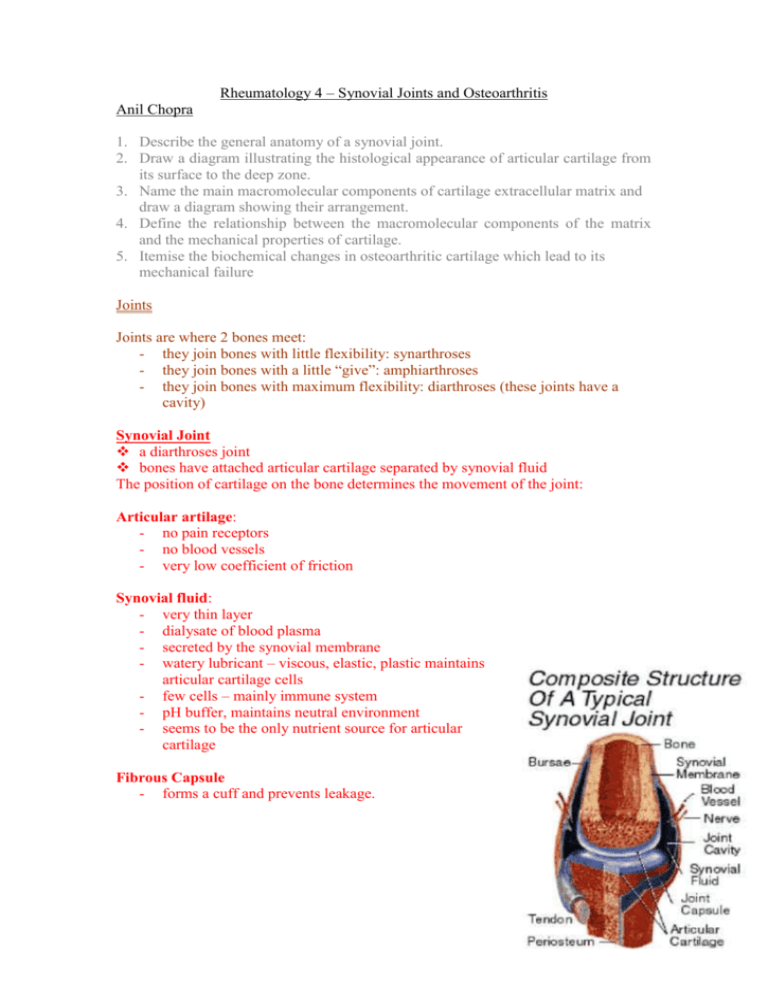
Rheumatology 4 – Synovial Joints and Osteoarthritis Anil Chopra 1. Describe the general anatomy of a synovial joint. 2. Draw a diagram illustrating the histological appearance of articular cartilage from its surface to the deep zone. 3. Name the main macromolecular components of cartilage extracellular matrix and draw a diagram showing their arrangement. 4. Define the relationship between the macromolecular components of the matrix and the mechanical properties of cartilage. 5. Itemise the biochemical changes in osteoarthritic cartilage which lead to its mechanical failure Joints Joints are where 2 bones meet: - they join bones with little flexibility: synarthroses - they join bones with a little “give”: amphiarthroses - they join bones with maximum flexibility: diarthroses (these joints have a cavity) Synovial Joint a diarthroses joint bones have attached articular cartilage separated by synovial fluid The position of cartilage on the bone determines the movement of the joint: Articular artilage: - no pain receptors - no blood vessels - very low coefficient of friction Synovial fluid: - very thin layer - dialysate of blood plasma - secreted by the synovial membrane - watery lubricant – viscous, elastic, plastic maintains articular cartilage cells - few cells – mainly immune system - pH buffer, maintains neutral environment - seems to be the only nutrient source for articular cartilage Fibrous Capsule - forms a cuff and prevents leakage. Other inclusions: - Non-articular bony surface - Tendons and ligaments passing through - Local apertures – bursae (purse-like spaces) - Articular disc or meniscus may split the cavity completely into two joints (e.g. TMJ temporomandibular joint) or be partial and partly divide cavity - menisci of the knee - Labra or lips cartilage around the edge of an articular margin which may deepen a concavity and add stability - Fat pads Classification of Synovial Joints Complexity Simple – with only 2 articular surfaces one convex (male) and one concave (female) Compound – there are more than 2 articular surfaces. Degrees of Freedom Moves in one plane uniaxial (i.e. elbow) Moves in two planes biaxial (i.e. MCPs) Moves in three planes triaxial (i.e. shoulder) Shape Hinge - interphalyngeal Pivot – proximal radio-ulnar Plane – carpal joints Condylar - wrist Saddle – thumb CMC Ball and socket – hip Function Movements at two bone ends are made up of: gliding of one surface over another - slide angulation of one surface over another – roll rotation about bone axis - spin Limitation of Joint movement Either by: - using up all the articular surface - adjacent soft tissue in the way ( these can be trained to be more flexible) - pain and stretch receptors NB: spastic paralysis (paralysis of muscles that move a joint) can result in restriction of joint movement Articular Cartilage As the adjacent diagram shows, there are four zones of cartilage, and a tidemark which is the boundary between the articular cartilage and bone junction. Zones Zone 1: Lamina splendens - Makes up around 10% of total cartilage - Most superficial - Collagen fibres are thin and horizontal - Low levels of glycosaminoglycans Zone 2: transitional zone - Makes up around 50% of total cartilage - Thicker collagen fibres - Arranged radially - High levels of proteoglycans & water Zone 3: Radial zone - Makes up around 20% of total cartilage - Largest collagen fibres - Arranged radially - Many chondrocytes Zone 4: Calcified zone. - Makes up around 20% of total cartilage - Separates cartilage from subchondral bone. - Collagen fibres penetrate into this zone and anchor cartilage to bone. The adjacent diagram shows the tidemark area – the articular cartilage and bone junction. As you can see, the tidemark falls between the subchondral bone and zone IV of the cartilage. Macromolecular Components of Cartilage Consist mainly of collagen and proteoglycans – type II collagen is the most abundant form Water is the most abundant component of articular cartilage. Water separates everything in cartilage, giving the cartilage a plasticity character. Chondrocytes are specialised cartilage cells which are found mainly in the deeper zone of the cartilage, and they are able to excrete their own extracellular matrix network. Functions • A load-bearing connective tissue • Can absorb impact and withstand shearing forces • These abilities are brought about by the compostion and structure of the cartilage matrix. • The fibres have an angular arrangement i.e. the fibres do not run in the same direction. Osteoarthritis Osteoarthritis is an extremely common age related disorder affecting synovial joints (knees, hips, hands, spine) involving dysregulation of normal tissue turnover and repair affecting all tissues of the joint and leading to joint failure. Pathological features include focal areas of destruction of articular cartilage associated with hypertrophy of the subchondral bone, joint margin, and capsule. Histopathological changes in Osteoarthritis include: - swelling of cartilage - increased water content - cracks due to increased water content (known as clefts) - cartilage thins and softens - underlying bone is exposed to synovial fluid therefore resulting in weight-bearing cysts - remodelling of subchondral bone - Sclerosis of bone - Bones get closer together and eventually rub Molecular Changes in osteoarthritis include: • Loosening of collagen framework restraint • Chondrocytes increase proteoglycan synthesis but also release more degradative enzymes which are meant to get rid of the old cartilage but also damage the new • Increased cartilage water content and softening • Cartilage fibrillation • Loss of substance • Osteophyte formation (bony projections) • Increased bone density below the area of cartilage loss Risk Factors Radiographs of OA joints OA can be seen in radiographs of several joints – the most common are included below… The radiograph shown here are slab radiographs of a normal and an OA femoral head. In OA, the three things to look for are subchondral sclerosis, cartilage loss, and presence of osteophytes all of which are indicated in the OA femoral head. Remember that sclerosis is the result of osteophyte activity – they attempt to repair the damaged joint by making the existing bone thicker/ The adjacent diagrams here show the clinical radiological features that are present in the hands with OA. The subchondral sclerosis is again very obvious, and here you can see a loss of joint space in the first carpometacarpal joint of the thumb – this is why OA patients often experience pain in this joint – it is because the carpal bone and metacarpal bone are rubbing against each other causing friction. Finally, this set of radiographs shows radiological features of OA in weightbearing joints. As you can see, the three key features are present – a loss of joint space (cartilage loss), subchondral sclerosis, and the presence of osteophytes. The loss of cartilage at weight-bearing joints is particularly relevant as it means that a great deal of pain is experienced during any activity that involves weight bearing.