Connective Tissue - Serrano High School AP Biology
advertisement

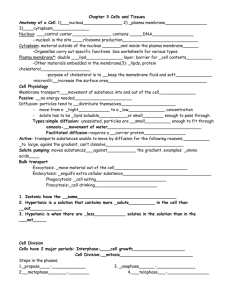
Connective Tissue: Connective tissue varies widely in appearance and function. However, they all have three basic components: 1) Specialized cells 2) Extracellular protein fibers 3) A fluid filled ground substance The protein fibers and fluid, together, make up the matrix that surrounds cells. Connective Tissue Overall Functions: Form the structural framework of the body. Transport fluids and dissolved materials. Protects organs. Support, surround, and interconnect other tissues. Stores energy, usually in the form of lipids. Defend our body from invasion. Classification of Connective Tissues: there are three general categories that are based on physical properties: 1) Connective Tissue Proper: this includes all connective tissues in the ground substance and is divided into a. Loose connective tissue b. Dense connective tissue 2) Fluid Connective Tissue: Different types of cells are suspended in a watery matrix. This matrix also contains dissolved proteins. 3) Supporting Connective Tissue: This tissue will protect soft tissues and support the weight of the body. Connective Tissue Proper: This connective tissue is made of extra cellular factors, ground substances (syrupy), and different types of cells. These cells migrate through the tissue. Cells of the connective tissue proper: 1) Fibroblasts: The most abundant and permanent resident. This is the only cell that is always present. The fibroblast secretes hyaluronan (a polysaccharide) and proteins. The hyaluronan combines with the proteins to form a proteoglycans. This makes the ground substance (the fluid) very syrupy. The proteins produced by the fibroblasts interact to form large extracellular fibers. 2) Macrophages: Large ameboid cells that is part of our immune system. This cell is the key to our nonspecific and specific immunity. They engulf invaders or damaged cells and can start the production of antibodies. They can also release chemicals that attract other phagocytes or start a fever. There are two types of macrophages: fixed (spend most of their time in tissues) or free (migrate). 3) Adipocytes/Adipose Cells: Fat cells. These cells vary from one tissue to another. 1 4) Mesenchymal Cells: Stem cells that are present in connective tissue. These cells will respond to injury and infection by dividing to produce daughter cells that can become other specialized connective tissue cells. 5) Melanocytes: These cells are found in the epidermis that produce melanin and provide skin pigment. 6) Mast Cells: These are small cells in connective tissue. These cells contain histamine and heparin. When stimulated, the mast cells will release those compounds, and these compounds cause the blood vessels to dilate. Basophils are blood cells that also release histamine and heparin. 7) Lymphocytes: B and T cells. These cells travel through connective tissues. These cells are responsible for your specific immune response. 8) Microphages: Neutrophils and Eosinophils. These are white blood cells (WBC) that will kill invaders. When macrophages release a chemical in tissues, these respond and help ‘clean’ the tissue. Connective tissue fibers: There are 3 types of fibers produced by fibroblasts: 1) Collagen: long straight and unbranched proteins. This is the most common type of protein in the connective tissue proper. These proteins are wound together like strands of rope to make the protein strong and flexible. Tendons (connect muscle to bone) are almost all collagen. 2) Reticular fibers: Thinner than collagen and branch. These fibers form a network. These fibers can resist forces that are applied in all directions. This network helps stabilize the relative positions and functions of specialized cells (parenchyma). 3) Elastin: Proteins that are branched and wavy. These proteins can snap back to their original length after being pulled. These form elastic proteins. Ground Substance: Ground substance fills space between cells and surround connective tissue fibers. Embryonic Connective Tissue: Embryonic connective tissue is called mesenchyme. Mesenchymal cells, star shaped stem cells, will produce all of the connective tissue. Mucous connective tissue (AKA: Wharton’s Jelly) is the connective tissue found in many parts of the embryo (even the umbilical cord). Although adults don’t have any embryonic connective tissue, we do have mesenchymal cells that help with tissue repairs. Loose Connective Tissue: This connective tissue fills the spaces between organs. It cushions and stabilizes the specialized tissue in the organs and supports the epithelia. Loose connective tissue is the styrofoam packing material of the body. Loose connective tissue surrounds and supports blood vessels and nerves, stores lipids and allows a route for substances to diffuse through. This tissue includes aveolar, adipose, and reticular tissue. 2 Aveolar Tissue: This tissue has a loosely organized, open framework. The viscous ground substance accounts for most of its volume. This tissue contains elastin fibers that allow it to return to its original shape after the external pressure has been removed. This tissue forms a layer that separates the skin from the deeper structures. There is much independent movement that this layer allows. Pinch your skin and move it around a little bit. Your skin moves and snaps back into the correct place? You don’t affect your muscle layer underneath. Make a muscle. Your muscle doesn’t pull on the skin, due to the aveolar tissue. This tissue also has an extensive blood supply. This is why it is common to inject drugs under the skin. Epithelium usually covers the aveolar tissue. Fibroblasts maintain the reticular lamina of the basal lamina that separates the aveolar tissue from the epithelium. The epithelium relies on the diffusion of oxygen and nutrients from the aveolar tissue. Adipose Tissue: Adipose cells are found in adipose tissue. This tissue provides padding, absorbs shocks, insulates and fills around structures. Adipose tissue is found under all of your skin, but there is a high concentration of adipose cells (Adipocytes) under the skin of your hips, buttocks, breasts and stomach. Most of the adipose tissue is called white fat, due to its pale yellow, white color. In infants and children, there is brown fat between the shoulder blades and around the neck. This fat is highly vascularized, and the adipose cells have a high number of mitochondria. This fat has a brown color and can increase the body temperature, by creating heat energy, by 100% quickly. However, it usually isn’t present in adults. Adipocytes are metabolically active cells. The lipids that we store are constantly being broken down and replaced. When food is scarce the Adipocytes deflate, the cells don’t die, they just decrease in size. When food is plentiful, the cells store the excess food as lipids. However, the cells can’t divide. The number of cells is established in the first few weeks of a newborns life. However, mesenchymal cells in the loose connective tissue can differentiate into adipose cells if the circulatory lipid levels are always high. Liposuction can remove unwanted adipose tissue, but adipose tissue can regenerate through the mesenchymal cells, so it is only temporary. Reticular tissue: this is found in many organs. The tissue has a complex 3-D stroma. This stroma supports the parenchyma cells (functional cells). Fixed macrophages and fibroblasts are associated with reticular fibers. Dense Connective Tissue: This is made up of mostly fibers. This tissue is usually called collagenous tissue, due to the fact that collagen fibers are the dominant protein. There are two types of dense connective tissue: dense regular connective tissue and dense irregular connective tissue. 3 Dense regular connective tissue: Collagen fibers are parallel to each other and they are tightly packed together. Tendons and ligaments are cords of dense regulary connective tissue. Tendons attach to muscles to bones. Ligaments line up bones by attaching bone to bones. The dense regular connective tissue also positions internal organs. An aponeurosis is a tendon sheet that attaches a large muscle to several bones. This is associated with the large muscles of the abdomen and back. Dense irregular connective tissue: This is an interwoven meshwork (without a pattern) of fibers. Areas that are subjected to stress from different directions are supported and protected by this connective tissue. Dense irregular connective tissue is found in the skin, around cartilage and bone (periosteum), and around internal organs. Both dense regular and irregular connective tissues contain elastin fibers and collagen. There is more elastin than collagen, which allows the tissue to be more flexible. Fluid Connective Tissue: Blood and Lymph: The watery matrix is called plasma. The plasma contains blood cells, cell fragments, proteins, and ions. There are 3 formed elements (cells and cell fragments): 1) Red Blood Cells (erythrocytes) 2) White Blood Cells (leukocytes) 3) Platelets Red Blood Cells: This cell is responsible for the transport of oxygen with hemoglobin. White Blood Cells: These include phagocytic cells: monocytes and macrophages, neutrophils, eosinophils, basophils and lymphocytes. These cells are responsible for non-specific and specific defenses. Platelets: Cell fragments that combine with proteins to form a blood clot. Lymph: Fluid that is forced out of the blood vessels and is collected by the lymph vessels. The fluid moves the through the vessels, through the lymph nodes (where the blood is filtered and cleaned), and back into the blood stream. Supporting Connective Tissue: Cartilage and bone provides the framework that supports the body. Cartilage: The matrix of the cartilage contains polysaccharide derivatives—chondroitin sulfate that joins with proteins to form proteoglycans. Cartilage cells are chondrocytes and are the only cells in the cartilage matrix. These cells occupy spaces called lacunae. Chondrocytes are avascular and must obtain nutrients and oxygen by diffusion. In fact, the chondrocytes produce antiangiogenesis factor—a protein that decreases blood vessel growth to cartilage cells. 4 Cartilage is set apart from other tissues by a fibrous perichondrium. The perichondrium contains two layers—outer fibrous layer and an inner cellular layer. The inner layer is important for growth and maintenance by chondrocytes. Cartilage Growth: Cartilage cells either grow by interstitial growth or appositional growth. Interstitial Growth: Chondrocytes in matrix divide and daughter cells produce more matrix. This process enlarges cartilage from within. Appositional Growth: New layers of cartilage cells are added to the surface. The inner layer of the perichondrium will undergo cell division. The inner most layer cells will then differentiate into cartilage cells. These cells will begin to produce a matrix and mature into chondrocytes. Types of Cartilage: There are three main types of cartilage: hyaline, elastic, and fibrocartilage. 1) Hyaline: This is the most common form of cartilage. The matrix of the cartilage contains closely packed collagen fibers—making it tough but somewhat flexible. This cartilage if found in the sternum, between the ribs, in the nose… 2) Elastic: This cartilage contains numerous elastin fibers, which makes it very flexible. This cartilage is found in the external ear (pinna), epiglottis, cartilage flaps in the larynx… 3) Fibrocartilage: This cartilage has little ground substance and is dominated by densely interwoven collagen fibers. This tissue is extremely durable and tough. You can find this cartilage in the intervetebral discs, pubic symphasis and within and around joints. Fibrocartilage resists compression, abrasions, shocks and prevents damaging bone to bone contact. This cartilage heals poorly. Several complex joints contain both hyaline and fibrocartilage. The hyaline covers the boney surfaces and fibrocartilage pads the joints to prevent bone to bone contact. If you tear fibrocartilage, it will not heal. The cartilage must be removed and smoothed over. Bone: We’ll be learning about the bones later. The biggest difference between connective tissue and the bone is the amount of ground substance. The bone has very little ground substance. Bones consist mostly of calcium phosphate and calcium carbonate (to a lesser degree). The collagen fibers (strong and flexible) are surrounded by the calcium salts (phosphate and carbonate). This provides a strong, hard, yet somewhat flexible structure. The collagen is like the rebar (steel bars) in concrete, and the calcium salts are the cement. Bone Organization: Lacunae is the space in the matrix that holds osteocytes. The lacunae are arranged around a blood vessel (and nerve) that branch through the bone. Osteocytes communicate with each other through tiny channels called canaliculi. The bone surface is covered by the periosteum 5 (connective tissue) that helps with the bone attachment to other tissues, helps heal when injured, provides blood vessels an nerves, and provides bone cells. With increased stress on the bones, they will become thicker and stronger. With little activity, the bones become thin and brittle. Membranes: The membrane is a physical barrier. Each membrane 1) covers the body and 2) consists of epithelia that is supported by connective tissue. We’ll learn about 4 membranes: 1) mucous membrane 2) serous membrane 3) cutaneous membrane 4) synovial membrane Mucous Membrane/Mucosae: These membranes line the passage ways and chambers that are exposed to the external environment: digestive, respiratory, reproductive, and excretory systems. The surfaces must be kept moist to 1) decrease friction, 2) increase absorption, and 3) trap antigens. These surfaces are lubricated by goblet cells or multicellular glands. The areolar tissue is called the lamina propria. Many of the mucous membranes are lined by simple epithelial cells and produce mucin that combines with water to form mucus. Serous Membranes: These membranes cover organs and body walls. There are three types: 1) Peritoneum: lines the peritoneal cavity and the surfaces of the organs. 2) Pleura: lines the pleural cavity and the lungs. 3) Pericardium: lines the pericardial cavity and the heart. These membranes are thin and firmly attached to the body wall and organs. The main function of the membrane is to reduce the friction between the organ and the body wall. Fluid called transudate is continually formed on the tissue membrane to reduce the friction. Cutaneous Membrane: Skin covers the surface of the body and consists of stratified, squamous epithelium with a layer of aveolar tissue reinforced by underlying dense irregular connective tissue. This membrane is thick and waterproof. Synovial Membrane: A fibrous capsule that surrounds the joint is lined with synovial membrane, which produces synovial fluid. The synovial membrane is areolar tissue containing a matrix of interwoven collagen fibers, proteoglycans, and glycoproteins. Synovial fluid decreases friction in the joints. 6 Connective Tissue Framework: These are the layers of tissue that connect the organs to the body. These layers: 1) provide strength and stability, 2) maintain relative positions of the internal organs, and 3) provide a route for blood vessels, lymph vessels and nerves. Fasciae are connective tissue layers (wrappings) that support and surround organs. There are three types of fascia: superficial fascia, deep fascia, and subserous facia. Superficial Fascia/Subcutaneous layer (AKA: hypodermis): This layer of aveolar tissue and fat separates the skin from the underlying tissues and organs. This layer provides insulation and padding, and lets the skin and underlying tissue move independently. Deep Fascia: This is made up of dense irregular connective tissue. This layer resembles plywood—how the fibers of the different layers run in different directions. This makes the tissue strong and tough. The capsules that are bonded to organs are also connected to deep fascia. Subserous Fascia: This layer lies between the deep fascia and the serous membranes. 7