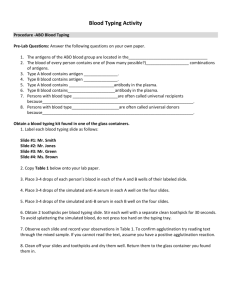
BLOOD TYPING
advertisement

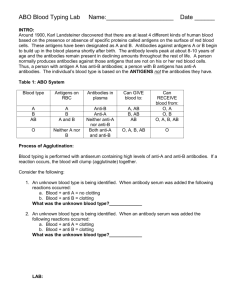
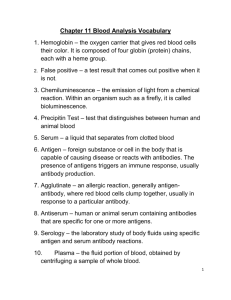
BLOOD TYPING Whose blood do we carry, our moms or dads? Or it doesn't matter because it could be from either one? Well, your blood is definitely all your own. But because of how the genetics of blood type works, it could seem like you have your mom's blood type, your dad's blood type, or a mix of the two. For every gene, you get two copies -- one from your mom and one from your dad. Even though the two copies are for the same gene, you can get different versions from each parent. These different versions are called alleles. Alleles are a little like cars -- the same make and model of car can come with either two doors or four doors. The cars do the same thing (get you where you're going!) but they are slightly different. Now let's talk about the genes for blood type. There are two main genes. One gene is for the ABO type. This gene codes for a protein that is on the surface of your blood cells. The different versions or alleles for the blood type protein are called A, B, and O. The other gene is for another protein on your blood cells called the Rh factor. The alleles are called plus (+) and minus (-). You can learn more about the Rh factor and its implications for health in the answer to another question on this website:http://www.thetech.org/genetics/ask.php?id=60. It doesn't matter what type your blood is unless you need a blood transfusion. In that case it is very important that you receive blood that is of the same type as yours (or type 0-, which I'll talk about at the end). If you get the wrong type of blood your body will see the transfused blood cells as foreign attackers and will destroy the new blood cells, making you very sick. The two genes for blood type are inherited separately, so we'll talk about them individually, and then put it all together at the end. Let's take an example of a mom who has blood type AB, and a dad who has blood type A. You might notice that the mom has two letters in her blood type. This is because she has the two different alleles she got from her parents (A and B). But then why does the dad only have one letter? It's because he either has two A alleles or he has one A allele and one O allele. This is just the way people write these things. There isn't any way to tell what kind of type A blood the dad has unless we know the blood types of his parents. For now we're going to assume that he has one A allele and one O allele, and we're going to write out both alleles when we talk about the possible blood types of the kids to make things easier for us. To figure out what blood type the kids of these two parents can have, we can use a genetics tool called a Punnett square. It's really just a chart that helps us organize the genes. We'll put the mom's alleles across the top, and the dad's alleles down the side. A B A O Each box in the chart represents a possible combination of the alleles donated by each parent (each box gets one entry from mom, one entry from dad). We can say what percent chance a child has of having a particular blood type by how many times that blood type shows up in the chart (one out of four is 25%, two out of four is 50%, etc.). 1 If we fill in the possible mixtures of alleles each kid could get in our example, we get a chart that looks like this. A B A AA AB O AO BO So the possible blood types are AA, AB, AO, and BO. Like I explained for the dad's blood type before, people with two A alleles (AA) and people with one A allele and one O allele are both called type A (the same thing goes for type B). So, the kids of these parents have a 50% chance of being what we call type A, a 25% chance of being type B, and a 25% chance of being blood type AB. You can do the same with the Rh factor gene. Let's say that the mom was Rh-positive (with one + allele and one - allele, though she could also have two + alleles) and the dad is Rh-negative (meaning both of his Rh alleles are -). + - - +/- -/- - +/- -/- There are two possibilities for the Rh-status of the kids. They have a 50% chance of being Rh-positive (+/-) and a 50% chance of being Rh-negative (-/-). Let's put it all together. The mom was blood type AB+, and the father was blood type AO-. A Punnett square for this is shown below. A+ A- B+ B- A - AA +/- AA -/- AB +/- AB -/O - AO +/- AO -/- BO +/- BO -/The possibilities for their child's blood type are. AA+, AA-, AB+, AB-, AO+, AO-, BO+, and BO-. (The Punnett square can also tell us that there is a 1 in 4 chance for either A+ or A-, and a 1 in 8 chance each for AB+, AB-, B+, and B-.) You can see that two of these, AB+ and AO- (in blue), are exactly like one of the parents. All the others are mixtures of the two. This is just one of the many examples of how the instructions for making you that are in your genes make you like your parents, but at the same time unique. I said at the beginning that if you needed a blood transfusion that you could either get the same blood type as your own, or else you could get O- blood. But why? People with O- blood are called universal donors because they can give blood to anyone. The reason is that the O and the - actually mean that their blood cells don't have any versions of either of the two proteins coded for by these gene on their surface. So there is nothing for a person's body to see as a foreign attacker. Unfortunately for these people, it also means that their bodies will see all other blood types as 2 foreign attackers and that they can only receive other O- blood. Is there a universal acceptor blood type? Yes, it is AB+. These people are lucky because their bodies are used to seeing both the A and B versions of the protein, and they are used to seeing the Rh+ factor. So no matter what kind of blood they receive, their bodies won't see it as a foreign attacker. Only about 3% of the population is this lucky (http://chapters.redcross.org/br/northernohio/INFO/bloodtype.html) Blood Types Human blood is grouped into four types: A, B, AB, and O. Each letter refers to a kind of antigen, or protein, on the surface of red blood cells. For example, the surface of red blood cells in Type A blood has antigens known as A-antigens. The Rh Factor Each blood type is also grouped by its Rhesus factor, or Rh factor. Blood is either Rh positive (Rh+) or Rh negative (Rh-). About 85% of Americans have Rh+ blood. Rhesus refers to another type of antigen, or protein, on the surface of red blood cells. The name Rhesus comes from Rhesus monkeys, in which the protein was discovered. Blood Transfusions Blood types become very important when a blood transfusion is necessary. In a blood transfusion, a patient must receive a blood type that is compatible with his or her own blood type—that is, the donated blood must be accepted by the patient's own blood. If the blood types are not compatible, red blood cells will clump together, making clots that can block blood vessels and cause death. Type O– blood is considered the “universal donor” because it can be donated to people of any blood type. Type AB+ blood is considered the “universal recipient” because people with this type can receive any blood type. Blood type Percent of Americans with this type Who can receive this type O+ 37% O+, A+, B+, AB+ O– 6 A+ 34 A– 6 B+ 10 B– 2 B+, B–, AB+, AB– AB+ 4 AB+ AB– 1 AB+, AB– All blood types A+, AB+ A+, A–, AB+, AB– B+, AB+ 3 Did You Know? Blood type is inherited, just like eye color. Certain blood types are more common in certain countries. In China, over 99% of the population has Rh+ blood. Different kinds of animals have different kinds of blood. Dogs have 4 blood types; cats have 11; cows have about 800. Some people think blood type tells about personality. Legend has it that Type A is calm and trustworthy; Type B is creative and excitable; Type AB is thoughtful and emotional; and Type O is a confident leader. In Japan, the idea of blood type as personality type is so popular that Japanese ask “What's your blood type?” about as often as Americans ask “What's your sign?” ABO Blood Types The most well known and medically important blood types are in the ABO group. They were discovered in 1900 and 1901 at the University of Vienna by Karl Landsteiner in the process of trying to learn why blood transfusions sometimes cause death and at other times save a patient. In 1930, he belatedly received the Nobel Prize for this discovery. All humans and many other primates can be typed for the ABO blood group. There are four principal types: A, B, AB, and O. There are two antigens and two antibodies that are mostly Karl Landsteiner responsible for the ABO types. The specific combination of these (1868-1943) four components determines an individual's type in most cases. The table below shows the possible permutations of antigens and antibodies with the corresponding ABO type ("yes" indicates the presence of a component and "no" indicates its absence in the blood of an individual). ABO Blood Type Antigen Antigen Antibody Antibody A B anti-A Anti-B A yes no no yes B no yes yes no O no no yes yes AB yes yes no no 4 For example, people with type A blood will have the A antigen on the surface of their red cells (as shown in the table below). As a result, anti-A antibodies will not be produced by them because they would cause the destruction of their own blood. However, if B type blood is injected into their systems, anti-B antibodies in their plasma will recognize it as alien and burst or agglutinate the introduced red cells in order to cleanse the blood of alien protein. ABO Blood Type Antigen A Antigen B Antibody anti-A Antibody Anti-B A yes no no yes B no yes yes no O no no yes yes AB yes yes no no Individuals with type O blood do not produce ABO antigens. Therefore, their blood normally will not be rejected when it is given to others with different ABO types. As a result, type O people are universal donors for transfusions, but they can receive only type O blood themselves. Those who have type AB blood do not make any ABO antibodies. Their blood does not discriminate against any other ABO type. Consequently, they are universal receivers for transfusions, but their blood will be agglutinated when given to people with every other type because they produce both kinds of antigens. ABO Blood Type Antigen A Antigen B Antibody anti-A Antibody Anti-B A yes no no yes B no yes yes no O no no yes yes AB yes yes no no It is easy and inexpensive to determine an individual's ABO type from a few drops of blood. A serum containing anti-A antibodies is mixed with some of the blood. Another serum with anti-B antibodies is mixed with the remaining sample. Whether or not agglutination occurs in either sample indicates the ABO type. It is a simple process of elimination of the possibilities. For instance, if an individual's blood sample is agglutinated by the anti-A antibody, but not the anti-B antibody, it means that the A antigen is present but not the B antigen. Therefore, the blood type is A. 5 Genetic Inheritance Patterns ABO blood types are inherited through genes on chromosome 9, and they do not change as a result of environmental influences during life. An individual's ABO type is determined by the inheritance of 1 of 3 alleles (A, B, or O) from each parent. The possible outcomes are shown below: Parent Alleles A B O A AA (A) AB (AB) AO (A) B AB (AB) BB (B) BO (B) O AO (A) BO (B) OO (O) The possible ABO alleles for one parent are in the top row and the alleles of the other are in the left column. Offspring genotypes are shown in black. Phenotypes are red. Both A and B alleles are dominant over O. As a result, individuals who have an AO genotype will have an A phenotype. People who are type O have OO genotypes. In other words, they inherited a recessive O allele from both parents. The A and B alleles are codominant. Therefore, if an A is inherited from one parent and a B from the other, the phenotype will be AB. Agglutination tests will show that these individuals have the characteristics of both type A and type B blood. CAUTION: the inheritance of ABO blood types does not always follow such straightforward rules of inheritance. ABO Blood type antigens are not only found on the surface of red cells. They are also normally secreted by some people in their body fluids, including saliva, tears, and urine. Whether someone is able to secrete them is genetically controlled. Police agencies now routinely use this so-called secretor system data to identify potential victims and criminals when blood samples are not available. Despite the fact that the blood types of children are solely determined by inheritance from their parents, paternity in the U.S. and many other nations can no longer be legally established based on conventional blood typing. To do that, it is necessary to compare HLA types and/or DNA sequences. The use of DNA is more accurate in determining paternity, but it is also more expensive than HLA typing. Antibodies to alien antigens in the ABO group are usually present in our plasma prior to the first contact with blood of a different ABO type. This may be partly explained by the fact that these antigens are also produced by certain bacteria and possibly some plants. When we come in contact with them, our bodies may develop long-term active immunity to their antigens and subsequently to the same antigens on the surface of red blood cells. This usually occurs to babies within the first six months following their birth. 6 Environmental Factors While blood types are 100% genetically inherited, the environment potentially can determine which blood types in a population will be passed on more frequently to the next generation. It does this through natural selection. Specific ABO blood types are thought to be linked with increased or decreased susceptibility to particular diseases. For instance, individuals with type A blood are at a somewhat higher risk of contracting smallpox and developing cancer of the esophagus, pancreas, and stomach. People who are type O are at a higher risk for contracting cholera and plague as well as developing duodenal and peptic ulcers. Research suggests that they are also more tasty to mosquitoes. That could be a significant factor in contracting malaria. NOTE: A small number of people have two different ABO blood types. They are not simply AB codominant. Apparently, most of these blood chimera individuals shared a blood supply with their non-identical twin before birth. In some cases, people are unaware that they had a twin because he or she died early in gestation and was spontaneously aborted. As many as 8% of non-identical twins may have chimeric blood. Some people are microchimeric--they have a small amount of blood of a different type in their system that has persisted from a blood transfusion or passed across the placental barrier from their mother before birth. Likewise, fetal blood can pass into a mother's system. This fact has led some researchers to suggest that the significantly higher frequency of autoimmune disorders in women is a result of the presence of foreign white blood cells that had come from their unborn children during pregnancy. NEWS: An international team of researchers led by Henrick Clausen of the University of Copenhagen, Denmark have discovered a bacterial enzyme that can convert red blood cells of types A, B, and AB into O by stripping away their identifying surface antigens. This has the potential for dramatically improving the safety of blood transfusions. Clinical trials of this technique are now underway. ("Bacterial Glycosidases for the Production of Universal Red Blood Cells", published online inNature Biotechnology, April 1, 2007.) NEWS: A research team led by Peer Bork of the European Molecular Biology Laboratory in Heidleberg, Germany discovered that people can be classified into one of 3 distinct types based on the kinds of bacteria in their guts. They refer to them as enterotypes. This type system is independent of blood types and may have equally important implications for peoples' health. How enterotypes are established is not known, but the authors suggest that babies may be randomly colonized by different species of bacteria and that they alter the gut so that only certain species of bacteria can live there. ("Enterotypes of the Human Gut Microbiome", published online in Nature, April 20, 2011.) 7 BLOOD IN THE BODY Blood transfusions were not possible until Karl Landsteiner first identified the major human blood groups -- namely O, A, B, and AB -- in a series of experiments in 1901 that earned him the Nobel Prize. (At the time, Landsteiner identified only groups A, B, and O; further analysis, two years later, revealed AB.) The ABO blood groups are defined by specific inherited molecules, or antigens, that are present on the surface of red blood cells. Thus, one inherits either A or B antigens (group A or B), both A and B antigens (group AB), or neither antigen (group O). Conversely, a person develops a natural immunity, or antibody, in their plasma to the ABO antigens that are absent on their own red cells. Thus, a group A person has anti-B antibodies, and group O person has both anti-A and anti-B antibodies. If group A red cells are mistakenly transfused to a group O recipient, for example, the anti-A antibody in the recipient's plasma destroys the transfused group A cells and a serious transfusion reaction occurs. Because group O has anti-A as well as anti-B antibodies, group O recipients can only accept blood from group O donors. Conversely, group AB recipients can receive blood from all groups. There are many other antigens on the red cell surface. The most important is the Rh factor. A person is defined as either Rh positive or Rh negative depending on the presence of the primary Rh antigen on the red cell. In contrast to ABO antigens, however, a person only develops anti-Rh after exposure to Rh-positive red cells through transfusion or pregnancy. Modern blood-banking technology uses highly sensitive tests to properly identify and match blood between donor and recipient. The most common blood types in the U.S. are A+ and O+ -- about 72 percent of the population has one or the other. AB- is the rarest blood type (1 percent of the population). 8