Slides
advertisement

6/20/2013
Welcome to the
Learning and Action Network to
Reduce
Healthcare-Associated Infections!
Session 3: Stop CAUTI-CUSP
Thursday, June 20, 2013
Your Hosts for Today’s Event
Centers for Medicare & Medicaid Services
and the
National Coordinating Center for
Improving Individual Patient Care
Annese Higgs,
CMS
Cathy Maffry,
IIPC NCC
1
6/20/2013
Objectives & Agenda
• Connect and share
evidence based practices
and tools to reduce CAUTIs
•
• Describe why and how On
the CUSP: Stop CAUTI can
reduce CAUTI rates
•
•
•
• Interpret and identify how to
implement On the CUSP:
Stop CAUTI methods in
your facility
•
•
•
Welcome from CMS (3 min.) CAUTIs
result in patient discomfort, excess
health care costs, and sometimes
mortality. CAUTI can be preventable.
On the CUSP: Stop CAUTI shares
ways to “Cut the CAUTI”
Patient Perspective (5 min.)
CAUTI – A Clinical Perspective (2025 min.) Dr. Carolyn Gould, CDC
What it is? Why it is difficult to reduce?
How can CUSP help reduce CAUTI?
(20-25 min.) Barb Edson, RN, HRET
Project Context, Overview, Outreach
Lessons from the Field (15 min.)
Representatives from hospitals will
share their success
Discussion Room (15 min.)
Call to Action (2 min.)
Disclosures
No Known Conflict of Interest from
Sponsorship, Hosted activities, or Funding sources
No Commercial Support was received
Non–endorsement of Products
There are no products endorsed in conjunction of this program.
Any use or demonstration of commercial products does not imply
endorsement by the Oklahoma Nurses Association, CMS, or
OFMQ.
Off-Label Use
There is no product use for a purpose other than that for
which is approved by the FDA.
It is the policy of the Oklahoma Nurses Association to ensure balance, independence, objectivity and scientific rigor in
all continuing nursing activities. This educational program was developed free from control from a commercial interest,
has no product endorsement or off-label product use.
2
6/20/2013
CMEs and CNEs Offered
(1.5 credits)
Event Evaluation Survey for this event is to be completed at
the end of the event presentation. Please launch the "Survey"
widget from the On24 Webcast console and complete the
Event Evaluation.
Post-Test link to Survey Monkey will be emailed to you AFTER
you attend the event.
This activity has been planned and implemented in accordance with the Essential Areas and Policies of the Oklahoma State
Medical Association (OSMA).
The Oklahoma Foundation for Medical Quality (OFMQ) is accredited by the OSMA to provide continuing medical education for
physicians. OFMQ designates this live activity for a maximum of 2 AMA PRA Category 1 Credit(s)™. Physicians should only
claim credit commensurate with the extent of their participation in the activity.
** It is the policy of the Oklahoma Nurses Association to ensure balance, independence, objectivity and scientific rigor in all
continuing nursing activities. This educational program was developed free from control from a commercial interest, has no
product endorsement or off-label product use. Oklahoma Nurses Association is an approved provider of continuing
nursing education by the Texas Nurses Association, an accredited approver by the American Nurses Credentialing
Center’s Commission on Accreditation.
How to Participate
Widgets on your Console:
Q&A
Group Chat
Slide box
Survey
Resources
And more
All can be moved around on your screen to suit your
needs.
3
6/20/2013
Poll & Chat
If you are representing a QIO, please use
the Group Chat box to tell us how many
of your recruited facilities are currently
implementing or plan to implement the
CUSP program.
We’d also like to know who is in the
audience, so please indicate that in the
pop-up poll on your screen.
Exciting
Line-Up
Barbara Edson,
HRET
Carolyn Gould, CDC
Melissa Varela
Valley Hospital
Michael Mutter
Valley Hospital
Mary Fine
Ozark Medical
Center
Kathryn Hoffman
Saint joseph Mercy
Hospital
4
6/20/2013
CAUTI Clinical Perspectives:
Diagnosis and Prevention
Carolyn Gould, MD, MSCR
Division of Healthcare Quality Promotion
Centers for Disease Control and Prevention
Cut the CAUTI
National Learning and Action Network to Reduce HAIs
June 20, 2013
National Center for Emerging and Zoonotic Infectious Diseases
Division of Healthcare Quality Promotion
Outline
National data on CAUTI
Recommendations for CAUTI prevention
Diagnostic challenges
Asymptomatic bacteriuria and antimicrobial use
From recommendations to implementation
5
6/20/2013
Pathogenesis of CAUTI
Source of microorganisms
• Endogenous (meatal, rectal,
or vaginal colonization)
• Exogenous (contaminated
hands of healthcare personnel
during catheter insertion or
manipulation of collecting
system)
Figure from: Maki DG, Tambyah PA. Emerg Infect Dis 2001;7:1‐6
Impact of CAUTI
• Most common type of HAI
> 30% of infections reported to NHSN
• Up to 139,000 hospital-onset, symptomatic
CAUTIs occur annually
• Leading cause of secondary BSI with ~10%
mortality
• $131 million in excess direct medical costs
Hidron AI et al. ICHE 2008;29:996‐1011
Richards M, et al. Crit Care Med 1999;27:887‐92
Wise M, et al. SHEA Abstract, Dallas, TX 2011
Scott R, et al. SHEA Abstract, Dallas, TX 2011
6
6/20/2013
Urinary Catheter Use
•
•
•
•
•
15‐25% of hospitalized patients receive catheters
5‐10% of NH residents have catheters
Often placed for inappropriate indications
Physicians frequently unaware
In a recent survey of U.S. hospitals:
– > 50% did not monitor which patients catheterized
– 75% did not monitor duration and/or discontinuation
Weinstein JW et al. ICHE 1999;20:543‐8
Warren JW et al. Arch Intern Med 1989;149:1535‐7
Benoit SR et al. J Am Geriatr Soc 2008;56:2039‐44
Rogers MA et al J Am Geriatr Soc 2008;56:854‐61
Munasinghe RL et al. ICHE 2001;22:647‐9
Saint S et al. Am J Med 2000;109:476‐80
Jain P et al. Arch Intern Med 1995;155:1425‐9
Saint S. et al. Clin Infect Dis 2008;46:243‐50
Historical Data: Reductions in CAUTI in
ICUs, 1990-2007
Pooled Mean Annual CAUTI Rate (SUTI)
per 1,000 Urinary Catheter Days
8
7
6
5
4
3
2
1
0
Medical
Surgical
Med/Surg Non‐Major Teaching
Med/Surg Major Teaching
Cardiothoracic
Coronary
*Hospitals participating in CDC’s NNIS, 1990-2004, and NHSN, 2006-07 (2005 data estimated
from log-linear models of annual CAUTI trends)
Burton DC, Edwards JR, Srinivasan A,
Fridkin SK, Gould CV. ICHE
2011;32(8):748-756
7
6/20/2013
Historical Data: Urinary Catheter Utilization
in ICUs, 1990-2007
Burton DC et al. ICHE 2011;32(8):748-756.
Challenges with evaluating
current CAUTI trends
• Reporting mandates and influx of new
facilities/units
• NHSN definitions
– Changes in 2009, 2013, 2015 (projected)
– Variable adherence to reporting rules
• Potential effects of reducing catheter-days
(effects unclear)
16
8
6/20/2013
State and National CAUTI
Reporting Mandates
• 11 states mandate CAUTI reporting via NHSN
– AL, AR, HI, GA, IN, NC, NJ, PA, TN, UT, WV
• National reporting mandates
– Acute care hospitals: Jan 2012 (adult and pediatric
ICUs)
– LTACHs, Inpatient rehab facilities: Oct 2012 (all
inpatient locations)
17
CAUTI PREVENTION
9
6/20/2013
CAUTI as Agency Priority Goal
• HHS has identified reduction of CAUTI and
CLABSI as Agency Priority Goals
• CAUTI baseline = 2010 SIR: 0.94 (2009 referent period)
• FY 2012 end goal = 10% reduction = SIR 0.85 (0.94 x
0.9)
• FY 2013 end goal = 20% reduction = SIR 0.75 (0.94 x
0.8)
http://www.hhs.gov/ash/initiatives/hai/
http://www.cdc.gov/hicpac/pdf/CAUTI/CAUTIguideline2009final.pdf
10
6/20/2013
Evidence-based Risk Factors
for CAUTI and/or bacteriuria
Prolonged catheterization*
Female sex
Older age
Impaired immunity
Disconnection of drainage system*
Lower professional training of inserter*
Placement of catheter outside of OR
Incontinence
* Main modifiable risk factors
CAUTI Core Prevention
Strategies
Catheter Use
• Insert catheters only for
appropriate indications
• Leave catheters in place
only as long as needed
Catheter
Insertion
Catheter
Maintenance
• Ensure that only properly
trained persons insert
and maintain catheters
• Maintain a closed
drainage system
• Insert catheters using
aseptic technique and
sterile equipment
• Maintain unobstructed
urine flow
http://www.cdc.gov/hicpac/cauti/001_cauti.html
11
6/20/2013
Appropriate Indications
http://www.cdc.gov/hicpac/cauti/001_cauti.html
Core Prevention Strategies:
Catheter Use
• Leave catheters in place only as
long as needed
– Remove catheters ASAP
postoperatively, preferably within 24
hours, unless there are appropriate
indications for continued use
http://www.cdc.gov/hicpac/cauti/001_cauti.html
12
6/20/2013
Core Prevention Strategies:
Catheter Insertion
• Insert catheters using aseptic
technique and sterile equipment
– Hand hygiene
– Use sterile gloves, drape, sponges,
antiseptic or sterile solution for
periurethral cleaning, single-use packet of
lubricant jelly
– Properly secure catheters
http://www.cdc.gov/hicpac/cauti/001_cauti.html
Core Prevention Strategies:
Catheter Maintenance
• Maintain a closed drainage system
– If disconnection or leakage occurs,
replace catheter and collecting system
– Consider systems with preconnected,
sealed catheter-tubing junctions
– Obtain urine samples aseptically
http://www.cdc.gov/hicpac/cauti/001_cauti.html
13
6/20/2013
Core Prevention Strategies:
Catheter Maintenance
• Maintain unobstructed urine flow
– Keep catheter and collecting tube free
from kinking
– Keep collecting bag below level of
bladder at all times (do not rest bag
on floor)
– Empty collecting bag regularly using a
separate, clean container for each
patient
http://www.cdc.gov/hicpac/cauti/001_cauti.html
Supplemental Prevention
Strategies: Examples
• Alternatives to indwelling urinary
catheterization
– Intermittent catheters
– External catheters
• Use of portable ultrasound devices
http://www.cdc.gov/hicpac/cauti/001_cauti.html
14
6/20/2013
CAUTI DIAGNOSTIC
CHALLENGES
Challenges in the diagnosis of CAUTI
Paucity of UTI-specific signs and symptoms (either
present or documented)
Special populations with atypical signs and
symptoms
Ventilated/sedated, altered mental status, spinal cord injury,
immunosuppressed, elderly
Frequency of bacteriuria and pyuria in catheterized
patients and the elderly
15
6/20/2013
IDSA Guidelines:
Signs and symptoms compatible with CAUTI
new onset or worsening of fever, rigors, altered mental status,
malaise, or lethargy with no other identified cause
flank pain
costovertebral angle tenderness
acute hematuria
pelvic discomfort
In those whose catheters have been removed, dysuria, urgent
or frequent urination, or suprapubic pain or tenderness
In patients with spinal cord injury, increased spasticity,
autonomic dysreflexia, or sense of unease
Hooton TM. Clin Infect Dis 2010;50
National Healthcare Safety Network
Surveillance Definitions for SUTI
http://www.cdc.gov/nhsn/PDFs/pscManual/7pscCAUTIcurrent.pdf
16
6/20/2013
Improving the UTI Surveillance
Definitions
Definitions should be:
Credible
Sensitive & specific – favoring specificity
Objective – minimizing need for interpretation/decision
making
Easy to capture – ideally, amenable to electronic reporting
Minimal burden
Appropriate for current laboratory protocols – criteria
should be applicable in most cases
Major issues being addressed
1.
2.
3.
4.
5.
6.
7.
Inclusion of yeasts
Polymicrobial urine cultures
Low urinary colony counts
Clinical criteria
Fever
Inclusion of urinalysis
New metrics
17
6/20/2013
ASYMPTOMATIC BACTERIURIA
AND ANTIMICROBIAL USE
Asymptomatic Bacteriuria (ASB)
18
6/20/2013
Asymptomatic bacteriuria (ASB)
• Definition
– Quantitative culture with ≥105 colony forming units/ml in an
appropriately collected urine specimen without clinical
signs/symptoms localizing to the urinary tract
• Incidence of bacteriuria with indwelling urinary catheters
– 3-10% per catheter-day
– 26% of people with a catheter between 2-10 days
– 100% of people with long-term (>30 d) catheters
• Bacteriuria is rarely symptomatic
Prevalence of ASB
IDSA Guideline: Nicolle LE et al. Clin Infect Dis 2005; 40:643–54
19
6/20/2013
ASB: DON’T screen/ treat
Nicolle, LE Int J Antimicrob Agents. 2006; 28S:S42-S48
When is it recommended to screen for
and treat ASB?
In pregnant women
Before transurethral resection of the prostate
and other urologic procedures where mucosal
bleeding is anticipated
“No recommendation can be made for screening
for or treatment of asymptomatic bacteriuria in
renal transplant or other solid organ transplant
recipients.”
Nicolle LE et al. Clin Infect Dis 2005; 40:643–54
20
6/20/2013
Is pyuria diagnostic?
Hooton TM. Clin Infect Dis 2010;50
Pyuria and ASB
• Pyuria accompanying bacteriuria is NOT an
indication for antimicrobial treatment
Nicolle LE. Int J Antimicrob Agents 2006;28S:S42-8
21
6/20/2013
Inappropriate treatment of catheterassociated ASB
32% of CA-ASB episodes identified at one center
over 3 months were treated inappropriately with
antibiotics
Independent risk factors for inappropriate treatment
of ASB:
Older age
Gram-negative organisms
Higher urine WBC
Three patients developed C. difficile infection shortly
after treatment for ASB
Cope M. Clin Infect Dis 2009;48:1182-8
Risks of antimicrobial use for ASB
Selection for antimicrobial resistant pathogens
Adverse reactions to antimicrobials
C. difficile infection
Exposure to antibiotics increases the risk of CDI by at least 3 fold for at least a month
Stevens et al. Clin Infect Dis. 2011 Jul 1;53(1):42-8
22
6/20/2013
“When antimicrobial agents are prescribed for the treatment
of UTIs, not only the antimicrobial spectrum of the agent but
also the potential ecological disturbances, including the risk
of emergence of resistant strains, should be considered.”
Strategies to reduce treatment of
ASB
Reduce inappropriate catheter use
Reduce inappropriate orders for urine cultures
Avoid reflex orders for UA/Ucx for “soft” indications (e.g., falls)
If you look you will find (and treat)!
• Difficult for clinicians to ignore a positive culture, regardless of
symptoms
• Pressure to treat – from physicians, RNs, patients, families
Reduce contamination/colonization
If CAUTI suspected, remove/replace long-term catheters (> 2
weeks) prior to culture
Doernberg SB, V Dudas, KK Trivedi, ID Week 2012, Poster presentation
Hooton TM. Clin Infect Dis 2010;50
23
6/20/2013
Downstream effects of urinary catheters
Secondary BSI
CAUTI
Bacteriuria
Immobilization
Urethral
Trauma
Antimicrobials
Pressure
Ulcers
Urinary
Catheter
Microbiome
Disruption
47
C.
difficile
infection
MDRO
colonization
MDRO
infection
Increased
LOS
MDRO
transmission
IMPLEMENTATION
24
6/20/2013
CAUTI Trends
11 prevention collaboratives in 8 states
p=0.02
p=0.02
p=0.8
States with ARRAfunded CAUTI
Collaboratives
States without
ARRA-funded
CAUTI
Collaboratives
Kate Ellingson et al. Presented at ID Week 2012
Quality Improvement Initiatives
Goals:
Ensure appropriate utilization of catheters
Identify and remove unnecessary catheters
Ensure hand hygiene and proper care of catheters
Examples of effective programs:
Alerts or reminders
Guidelines and protocols for nurse-directed removal of
unnecessary urinary catheters
Education and performance feedback
Guidelines and algorithms for appropriate peri-operative
catheter management
http://www.cdc.gov/hicpac/cauti/001_cauti.html
25
6/20/2013
One Reason Catheters Are Used
Inappropriately
Level
Proportion
Unaware of
Catheter
Medical Students
18%
House Officers
25%
Attending Physicians
38%
Saint et al Am J Med 2000
26
6/20/2013
Results of the Meta-analysis
Rate of CAUTI reduced by 52% (P < .001) with use of reminder or stop order
Mean duration of catheterization decreased by 37%, resulting in 2.6 fewer days
of catheterization per patient
Meddings et al. Clin Infect Dis 2010; 51
Catheter insertion: We have the
technique down, so what’s the
problem?
• Untrained personnel often given the
responsibility of placing catheters
– A known risk factor for bacteriuria
– Task often delegated to nursing
assistants/techs
– Poor oversight by hospitals
– ED placement often a routine practice and
undocumented
27
6/20/2013
Resources for catheter insertion
training
•
NEJM Videos in Clinical Medicine:
– Male Urethral Catheterization
T. W. Thomsen and G. S. Setnik - 25 May, 2006
– Female Urethral Catheterization
R. Ortega, L. Ng, P. Sekhar, and M. Song - 3 Apr, 2008
•
Educate, document competency (e.g., simulation),
and audit
•
http://www.nejm.org/
Example of Auditing Tool
Urinary Catheter Checklist
Yes
No
Insertion
Hand hygiene performed before and after insertion
Catheter placed using aseptic technique and sterile equipment
Catheter secured properly after insertion
Catheter insertion and indication documented
Maintenance
Hand hygiene performed before and after manipulating catheter
Catheter and collecting tubing are not disconnected (irrigation avoided)
Urine bag emptied using aseptic technique
Urine samples obtained aseptically (via needless port for small volume)
Urine bag kept below level of bladder at all times
Catheter tubing unobstructed and free of kinking
Need for urinary catheters reviewed daily with prompt removal of
unnecessary urinary catheters
28
6/20/2013
Summary
Reduction of unnecessary urinary catheter use has
many potential patient safety benefits
Reduction of CAUTI, antimicrobial use, MDRO colonization, CDI,
urethral trauma, immobility, etc
Evaluation of recent national CAUTI trends is
complicated by influx of new reporters and shifting
surveillance definitions
Taking a systems-approach to prevention is highly
effective
Thank you!
Questions?
For more information please contact Centers for Disease Control and
Prevention
1600 Clifton Road NE, Atlanta, GA 30333
Telephone, 1-800-CDC-INFO (232-4636)/TTY: 1-888-232-6348
E-mail: cdcinfo@cdc.gov Web: www.cdc.gov
The findings and conclusions in this report are those of the authors and do not necessarily represent the official
position of the Centers for Disease Control and Prevention.
National Center for Emerging and Zoonotic Infectious Diseases
Place Descriptor Here
29
6/20/2013
On the CUSP: Stop CAUTI
National Project Overview
Barb Edson, RN, MBA, MHA Vice President of Clinical Quality, HRET 59
Agenda
Topic
Presenter(s)
On the CUSP: Stop CAUTI
National Project Goals & Overview
Barb Edson, HRET
The Valley Hospital, Ridgewood, NJ
Michael Mutter & Melissa Varela
Ozarks Medical Center, West Plains, MO
Mary Fine
St. Joseph Mercy Hospital
Katy Hoffman
Questions and Wrap‐up
Barb Edson
60
30
6/20/2013
Acknowledgments
The Health Research & Educational Trust and HPOE would like to thank:
• Agency for Healthcare Research and Quality
• Michigan Health & Hospital Association Keystone Center for Patient Safety & Quality
• University of Michigan Health System
• St. John Hospital and Medical Center
• Johns Hopkins Armstrong Institute for Patient Safety and Quality
• Extended Faculty Organizations:
• Association for Professionals in Infection Control and Epidemiology
• Emergency Nurses Association
• Society for Healthcare Epidemiology of America
• Society of Hospital Medicine
61
Poll
Have you ever used CUSP in your unit or has your hospital ever used CUSP in another unit?
a. I have heard of CUSP, but have never used it.
b. I have never heard of CUSP.
c. Our unit has not used CUSP, but other units have.
d. Our hospital uses CUSP in at least one unit.
62
31
6/20/2013
On the CUSP: Stop CAUTI
The goals of the national project are to:
• Reduce mean CAUTI rates in participating clinical units by 25 percent
• Improve safety culture as evidenced by improved teamwork and communication by employing CUSP methodology
Part of the Hospital
Engagement
Network (HEN)
CAUTI
Pressure ulcers
Urinary Catheter Harm
Venous thrombo‐
embolism?
Immobility
Falls?
63
Increased Length of Stay
Patient dignity*
Trauma
*Saint S, Ann Intern Med 2002; 137: 125-7
64
32
6/20/2013
Participation
As of June 10:
• 870 Hospitals Registered
• 1,368 Registered Units
• 35 states, Puerto Rico & UHC HEN 65
Project Vitals • Duration – 18 Months • Components – Technical and Adaptive (cultural)
• 3 Learning Sessions
• Monthly Content Calls
• Monthly state‐specific Coaching Calls • All Units & Emergency Departments
66
33
6/20/2013
Inpatient Implementation Timeline
WHAT
WHEN
State and QIO Commit to Participate
September 6, 2013
Hospital Unit Informational Webinars
Late September 2013
Hospital Units Commit to Participate
October 25, 2013
Kickoff & Onboarding Webinars
November 2013 – January 2014
Start Monthly Content Calls
February 2014
Baseline Data Collection
January – March 2014
Start Monthly Coaching Calls
February 2014
Implementation Data Collection
March – April 2014
67
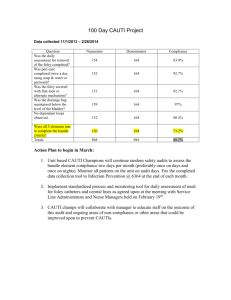
Measuring Progress
Measure
Collection Schedule
CAUTI RATES (Outcome):
• # Symptomatic CAUTIs
• # urinary catheter (UC) days per month
• # of patient days per month
Collect monthly for 5 months beginning January 2014, then quarterly thereafter (January—March will be considered outcome baseline).
PREVALENCE & APPROPRIATENESS (Process):
• Assess each patient on unit for presence of UC
• Record the reason for the UC
Baseline: Mon‐Fri for 3 weeks; Implementation: Mon‐Fri for 2 weeks, 1 day per week for 6 weeks, then 1 week per quarter thereafter.
TEAM CHECK‐UP TOOL
• Assess how well the unit team is implementing CUSP & CAUTI prevention activities
Complete and submit quarterly starting in April 2014.
68
34
6/20/2013
CAUTI Rate: (CAUTI Episodes/Catheter Days) x 1,000
CAUTI Rate: Overall
3.0
2.5
2.0
1.5
1.0
0.5
0.0
BL 1
(n=973)
BL 2
(n=970)
BL 3
(n=963)
P 1
(n=947)
Overall Rate
P2
(n=907)
P3
(n=585)
P4
(n=439)
P5
(n=264)
P6
(n=150)
Baseline Rate
69
BL=Baseline; P=Post Baseline
Overall Relative Reduction
Post Post Post Post Post Post Baseline Baseline Baseline Baseline Baseline Baseline Baseline
1
2
3
4
5
6
(n=990) (n=947) (n=907) (n=585) (n=439) (n=264) (n=150)
Overall Rate
Relative
Reduction
2.580
2.283
2.381
2.451
2.420
2.044
1.575
NA
‐11%
‐8%
‐5%
‐6%
‐21%
‐39%
Note: Relative reduction based upon CAUTI rate calculated using NHSN methodology. All reductions are
relative to baseline. Cohort 5 is in baseline data collection phase and therefore not reflected in the above
calculations.
70
35
6/20/2013
Utilization Ratio: By Cohort
Utilization Ratio: (Catheter Days/Patient Days)x100
50%
45%
40%
35%
30%
25%
20%
15%
10%
5%
0%
BL 1
(n=973)
BL 2
(n=970)
Cohort 1 Ratio
BL 3
(n=963)
P 1
(n=947)
Cohort 2 Ratio
P2
(n=907)
P3
(n=585)
Cohort 3 Ratio
P4
(n=439)
Cohort 4 Ratio
P5
(n=264)
P6
(n=150)
Overall Ratio
71
BL=Baseline; P=Post Baseline
Partnerships & Dissemination CAUTI National Project Team
HRET MHA UM/St. Johns JHU
State Hospital Associations, Partners & Coalitions
Extended Faculty
Network
State Leads, QIO, HEN‐
Coaching/CUSP/
Recruitment/Project Liaison
National & Regional CAUTI Faculty APIC, SHEA, SHM, ENA
Coaching/Recruitment/ Endorsement
Hospitals/Units
72
36
6/20/2013
CUSP ‐ CAUTI Goals:
Required Data GOAL #1
Improving the Culture of Safety: CUSP
REQUIRED DATA:
• Quarterly Team Checkup Tool (TCT)
STEPS: 1. Educate on the science of safety
• HSOPS at baseline and post‐intervention
2. Senior Executive Adopts Unit
3. Identify Safety Defects
4. Learn from Defects
5. Use teamwork/ communication tools 73
From Higher to Lower Use Areas
ICU
PACU/OR
• Remove promptly after surgery before transfer out
• Evaluate for continued need
• Discontinue no longer needed before transfer out
ED
• Avoid initial placement
• Reevaluate for continued need after patient stabilizes
Non‐ICU
Evaluate need on admission
Evaluate for continued need
74
37
6/20/2013
Poll
Do you have a program in the ED to decrease urinary catheter utilization?
a. Yes
b. No
75
Intervening in the ED
• ED: an area where a large number of urinary catheters are placed
• Addressing the appropriateness of placement of urinary catheters in the ED may also help reduce unnecessary urinary catheter use
ED
ED: Prevent
inappropriate
urinary catheter
placement
All hospital
units
76
38
6/20/2013
Early Efforts in the ED • One center: institutional guidelines in ED, intervention with physicians; UC use dropped about a third with intervention, with physicians ordering fewer UCs post‐intervention (Fakih et al, Acad Emerg Med, 2010; 17:337–340).
• Pilot work recently implemented in >30 EDs in Michigan (through MHA) and Ascension Health with successful results; key was engaging nurses and physicians using champions
77
ED Improvement Intervention
• Expand the reach of the On the CUSP: STOP CAUTI national collaborative
• Engage national societies to support the work
American College of Emergency Physicians (ACEP)
Emergency Nurses Association (ENA)
• Goals: improve appropriateness of catheter placement, and proper insertion technique
• Focus on the technical and adaptive (including teamwork and CUSP)
78
39
6/20/2013
ED Improvement Intervention Resources
National project support includes:
•
Comprehensive ED Tool Kit with customizable resources
•
Educational events:
•
National expert presentations
Coaching support by the National Project Team
In‐person training opportunities
Data collection and analysis:
Number of admits from the ED, including observation patients
Number of admits from the ED, including observation patients with a newly placed indwelling catheter
79
ED Toolkit
• ED quick guide for implementation
• Educational material (posters, brochures, pocket cards, algorithms)
• Toolkit and other resources available on the CUSP website:
http://www.onthecuspstophai.org/on‐the‐cuspstop‐
cauti/toolkits‐and‐resources/emergency‐department‐
improvement‐intervention/
80
40
6/20/2013
ED Implementation Timeline
Week 1 ‐ 2 Baseline: Collect urinary catheter initial placement prevalence; number of admissions from the ED as well as admissions from the ED with a newly placed indwelling catheter (14 days).
Week 3
Pre‐Implementation: Prepare for the implementation. Create staff awareness and excitement about the program. Begin emergency physician and nursing staff education.
Weeks 4‐5 Implementation: Educate on proper (aseptic) insertion technique and maintenance, as well as removal of catheters placed prior to transfer to inpatient units if appropriate. Collect number of admissions from the ED as well as admissions from the ED with a newly placed urinary catheter (14 days).
Quarterly
Sustainability: Collect urinary catheter initial placement prevalence (total of 14 days per quarter).
81
ED Implementation Roll‐out
• 1st ED Cohort starting June 2013
• 2nd ED Cohort starting Mid‐September 2013
82
41
6/20/2013
Facility Presenters
Michael Mutter, MS, RP
Director of Patient Safety
Mary Fine, RNC, QMHP
Director of Quality
Ozarks Medical Center
West Plains, MO
&
Melissa Valera, MSN, RN
Coordinator, Patient Safety
The Valley Hospital
Ridgewood, NJ
Kathryn L. Hoffman, RN, BSN
Director, Patient Care Services Women's, Children's, and Specialty Services
Saint Joseph Mercy Hospital
Ann Arbor, MI
83
•The Valley Hospital, Ridgewood, NJ
42
6/20/2013
Poll
How effective is collaborative learning to drive quality improvement in your facility?
a) Collaborative learning has been highly effective in our organization b) Collaborative learning has been somewhat effective in our organization
c) We are new to collaborative learning d) Collaborative learning was not effective in our organization
85
Organizational Commitment
• Collaborative participants
• Early Adoption of Bundles
• Strategic Initiative/Leadership Support
43
6/20/2013
Team Work
• Clinical
• Medical
• Administrative
Staff Education
• Technical 44
6/20/2013
Staff Education
• Environmental Reward & Recognition
• Recognize Team success!
• Celebrate our outcomes!
45
6/20/2013
Patient & Family Education
• “Knowledge is power”
• Hand Hygiene
Measurement & Evaluation
• Rates vs Raw numbers
• Power of a story
46
6/20/2013
Results
Urinary Catheter Infections
16
14
Number of CAUTI
12
10
8
6
4
2
0
ICU
Critical Care
Spread & Sustainability
• Align unit based goals with system wide goals
• Create Evidence Based Practice ACTION PLANS
• Awareness of vulnerabilities
47
6/20/2013
Cut the CAUTI: The Ozarks Medical Center Story
Mary Fine, RNBC, QMHP, SANE Ozarks Medical Center:
Our Story of CUSP Implementation
• Chose our ICU‐ 12 bed open unit
• Began with CUSP kick off‐ 2hrs
– Josie King video
– Brief power point with CUSP overview
– Science of Safety video by Dr Provonost
(Kick off includes all team members that was selected)
• Front line unit leaders present power point and Josie King to peers
• Time is assigned to watch science of safety and attendance is recorded by completion of the staff safety assessment tool
• Learning from defect is chosen from results
• Then began rolling out to other floors
48
6/20/2013
First Ideas
• Educate
• Visual trigger
• Electronic triggers
• Flag chart
• Add documentation
*** We solved it all
97
Next Steps
•
•
•
•
•
Add members to CUSP team
Visual reminder
Paper documentation
Label chart
Education to staff
98
49
6/20/2013
Stumbling Blocks
• Part paper and part computer
• Need to update nursing shift assessment to capture indications
• ED is on a different system
99
Solutions
100
50
6/20/2013
Solutions
• Created an electronic order that can be placed by US to send trigger to nurses work list for Foley removal in two days……..
(Creating this order then identified where education needed to be provided. 2N was calling floors asking why was the catheter indicated)
101
Solutions
Nurses Work List
102
51
6/20/2013
Solutions
• Education on indications and alternatives. Posted the indication cards on all nursing units
1.
2.
3.
4.
5.
6.
7.
Appropriate Indications for Foley Catheter: Acute urinary retention or obstruction
Perioperative use in selected surgeries
Assist healing of perineal and sacral wounds in incontinent patients
Hospice/comfort/palliative care
Required immobilization for trauma or surgery
Chronic indwelling urinary catheter on admission
Accurate measurement of urinary output in critically in ill patients (ICU only)
103
CAUTIs per 1000 Patient Days
SCIP Inf 9‐ removal POD 1 or 2 increased to 99.9% (1 fall out)
52
6/20/2013
Sustainability
105
Reward and Recognition
53
6/20/2013
Success Stories
• Patient in the hospital more than 20 days, multiple units then comes to 2N. Patient has Foley. Nurse Manager asks physician are you aware she has a Foley? We don’t have an indication and we are a no Foley floor
Result is that Foley was removed because nursing inquired
107
Success Story
• Bariatric patient with amputee requested for physician to allow the patient to have a Foley. Staff reviewed Foley’s during huddle board and no appropriate indication was available so nursing called physician and Foley was removed
Result is that the patients risk for acquiring a CAUTI was reduced by removal of an unnecessary line
108
54
6/20/2013
On the CUSP: STOP CAUTI
The Improvement Journey: A Sprint and a Marathon
Katy Hoffman, RN, BSN, NE‐BC
St. Joseph Mercy Hospital, Ann Arbor, MI
The CAUTI Journey at SJMH
• Keystone HAI Team formed in 2005
• Began Improvement journey with implementation of CUSP in alignment with Hand Hygiene program
• Planning for CAUTI pilots in 2007
• The team and the work have adapted along the way
• Still going strong today . . . .
This is our Journey
55
6/20/2013
Objectives
• Relate St. Joseph Mercy Hospital’s experience in using CUSP to reduce CAUTI
• Describe the technical aspects of the CAUTI prevention strategies
• Demonstrate alignment of CUSP in the prevention of CAUTI
CUSP and CAUTI Improvement Model
• Adaptive Interventions
– 4E’s Model
– Comprehensive Unit‐
based Safety Program
Appropriate Use
• Technical Interventions
– Appropriate Catheter Use
– Proper Catheter Insertion and Maintenance Intervention
– Prompt Catheter Removal Intervention
4 E
CUSP
Prompt Removal
Proper Insertion and Maintenance
56
6/20/2013
CUSP: The Science of Safety
• AHRQ Safety Culture Survey
– Understand current state
– Action plan for areas of opportunity
• Safety as a System Video (Brian Sexton) http://dukepatientsafetycenter.com/video.asp
•
•
•
•
•
•
Josie King Story/Video Executive Safety Rounds
Focus on Systems
Huddle Boards: Visibility of Data Unit‐based Safety Ambassadors Interdisciplinary Rounding and Standard Work
SJMH Technical Interventions: Appropriate Use
Initial Implementation •
•
•
•
•
•
Engage: CAUTI facts, Josie King Video
Keystone “Bladder Bundle” Implementation on 2 Pilot Units
– Baseline assessment
– 2 –week education/coaching intervention – Follow‐up assessment
– Ongoing data collection
Educate: Individual “on the spot” education/coaching by rounder
Educate: CDC/HICPAC Indications
Initial Education
– Nurse managers
– Bedside RN’s
– Physicians
– Leadership teams
Execute: Paper physician reminder process based on RN assessment at MN
Current State
•
•
•
•
•
•
•
•
Spread System‐wide
Physician Champion/Buy In
Eliminate/Reduce use in certain surgical procedures through standard order sets
Data: Quarterly audits
– Point prevalence measures
– Process measures
Leverage EMR: Hard Stop for Indication
Equipment and Supplies to limit use
– BSC in every room
– Bladder scanners
Education
– Yearly resident education
– Yearly healthstream education
– 3‐6 month updates to quality and practice teams
Patient/Family Education
57
6/20/2013
Technical Interventions: Insertion and Maintenance
Initial Implementation
• Policy Review/Revision
• Education
– Reducing manipulation of catheter
– Securing catheter: Stat‐lock, leg strap, tape
– Closed system
– Specimen collection
– Inclusive of transporters
• Competency in orientation
• Standard equipment (kits)
•
•
•
•
Current State
Quarterly Audit: point prevalence and process measures
Updated supply chain to include Stat lock standard in all catheter kits and urometers for all surgical cases
Aseptic technique competency (100%)
Yearly Healthstream Education (RN/PCT)
Quarterly Point Prevalence Audit Example
Is there an order? (Yes/No)
Check reason for initial Foley insertion:
– Acute urinary retentions or obstruction
– Accurate measurements of urinary output in critically ill patients
– Perioperative use for selected surgical procedures
– Assist in healing of open sacral or perineal wound in incontinent patients
– Improve comfort for end of life care
– Patient requires prolonged immobilization
–
Other, please specify _________________________________________
IUC Insertion Documented (Yes/No) Date ___________
Time _____________
Is IUC still indicated? (Yes/No)
Check reason for continued Foley maintenance: (Selections same as above)
Is the IUC secured to the patient?
How is the IUC secured? (Stat lock/Tape/Other {please specify _______________})
Is the IUC positioned below the level of the patient’s bladder? (Yes/No)
Is the urine bag tubing free of dependent loops? (Yes/No) Is the bag secured to the bed or chair to prevent pulling of the entire catheter system? (Yes/No)
Is the IUC bag hanging free without touching the floor? (Yes/No) 58
6/20/2013
Technical Interventions: Prompt Removal
Initial Implementation
• Paper daily screening tool
• Nurse focused intervention
• Paper daily reminder in chart for physician signature
• Manual collection of catheter days
Current State
• Order sets with stop orders
– Anesthesia buy‐in for discontinue with thoracic epidurals
• Daily alert: – Nursing and Physician alerts (Safety Page)
– Requires response in the form of an order
• Standardized documentation for insert/removal
• Automated Report: Catheter Days
• Presence of catheter displays in various locations within EMR
• Huddles
• Learning from defects (SCIP)
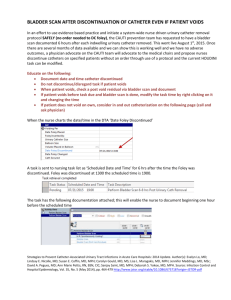
Leverage EMR: Screen Shots
59
6/20/2013
Leverage EMR: Screen Shots
Preventing CAUTI: Lessons Learned
• A Sprint and a Marathon
– Urgency for quick wins and immediate results
– Consistency for continued progress and goals for improvement
• Join Forces: Work with the surgical team to improve SCIP and CAUTI
• Include front line staff: don’t underestimate the power of engaged physician partners
• Change involves adaptive and technical challenges, plan interventions for both
60
6/20/2013
Preventing CAUTI: Next Steps
• Extend the collection and reporting of CAUTI rates beyond the ICU’s and Rehab Unit: Perform LFD on all CAUTIs in the ICU’s
• Include catheter use in Standard Work of Interdisciplinary Rounding Teams
• Continue to leverage EMR reporting capabilities
for real‐time response (New Safety Page)
• Further explore nursing discontinuation protocol
• Implement catheter appropriateness pilot intervention in ED
61
6/20/2013
For More Information
For more information of the On the CUSP: Stop CAUTI project, please visit:
http://www.onthecuspstophai.org/on‐the‐
cuspstop‐cauti/
123
Questions? 124
62
6/20/2013
Let’s Chat
Carolyn Gould, CDC
Melissa Varela
Valley Hospital
Please use the
Q&A Widget
on your Console
Michael Mutter
Valley Hospital
Mary Fine
Ozark Medical
Center
Barbara Edson,
HRET
Kathryn Hoffman
Saint joseph Mercy
Hospital
Thank you!
Follow up questions can be submitted to your local QIO or to
the IIPC NCC Aim Team at:
iipcaimncc@okqio.sdps.org
Please take a minute to provide feedback
on this educational activity using your survey widget.
To receive CE, please complete the Post Test as well
Thank you!
This material was prepared by the Oklahoma Foundation for Medical Quality and Stratis Health, the National Coordinating Center (NCC) for Improving Individual Patient Care (IIPC), under contract with the Centers for Medicare & Medicaid Services (CMS), an agency of the U.S. Department of Health and Human Services. The contents presented do not necessarily reflect CMS policy. 0710SOW‐IIPC NCC‐C7‐221 04252013
63