Mary A. Petersen, MSN, RN
advertisement
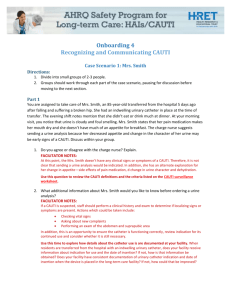
Urine-8 Project: Next Step Mary A. Petersen, MSN, RN: Director of Professional Nursing Practice Betsy Demarest, BBA, RN, CNOR: Director of Surgical Services Trinity Medical Center – Quad Cities Urine-8 Committee Members Michelle Blackmer, MSN, FNP-BC, RN Stan Buck, RN, RNFA Pam Elliott, MBA, BFA Chris Hansen, MS, RN Diane Laake, RN, CMSRN Paula Maddox, MSN, RN, CCRN Kathryn Marhoefer, MBA, RN Michelle Mathias, BSN, RN Mary A. Petersen, MSN, RN (Committee Chair) 2 CAUTI Statistics Nationwide 80% of HA UTIs are caused by urinary catheters 5% deaths from HAIs are urinary catheter associated Cost of a CAUTI is estimated at $500-1000, $2800 if bacteremia Source: Michigan Keystone Project, 2008 3 Trinity CAUTI Rates CAUTIs 2006-2009 Raw Rate /1000 pt days # 2006 103 1.1 Year 2007 77 0.87 2008 89 0.86 2009 69 0.82 Rate / 1000 Foley days 4.25 4 First Step Determine specific nursing opportunities 1. 2. to decrease foley related UTI’s Conducted a one-day prevalence study Primary aims of the study included Quantify the level of use of indwelling urinary catheters Determine the level of adherence to guidelines 5 Methods 2007, 2008 & 2010 all units on each campus surveyed List obtained identifying all patients with Foley and RN providing direct care Data collector directly observed the catheterized patients and interviewed RN Data was collected on a standardized form 2011 & 2012 implemented Adaptive Design methodology 6 Foley Practice Areas Reviewed Presence of a Foley catheter Catheter secured to the pt’s abdomen or leg Tamper Evident Seal intact (TES) Tubing extended to prevent the development of dependent loops of drainage tubing Tubing secured to patient bed or chair to prevent pulling on system Drainage system not touching the floor Urine bag not over filled with urine 7 Percentage % Percentage (%) of Compliance with Total Foley Practice Areas 2007 2008 2010 8 9 10 SBAR 11 Catheter Associated Urinary Tract Infection (CAUTI) Prevention URINE-8 1 2 Good hand hygiene 3 Proper peri care: Daily with bath, fecal incontinence, presence of discharge or drainage and at bedtime Document peri-care 4 Secure catheter to patient with a Stat Lock Change Stat Lock every 7 days Do not use Stat Lock on edematous patient 5 U/A upon catheter insertion when symptoms present ▪ Document symptoms in Care cast 6 7 Do not break the red seal 8 Remove as soon as medically able *SCIP – Remove by the end of post-op day 2 Inserted by qualified staff Sterile technique when inserting catheter Unobstructed urine flow No kinks, bends, or dependent loops Keep urine bag off the floor 12 Trinity CAUTI Rates CAUTIs 2006-2011 Raw Rate /1000 pt days # 2006 103 1.1 Year Rate / 1000 Foley days 2007 77 0.87 2008 89 0.86 2009 69 0.82 4.25 2010 18 0.18 0.97 2011 18 0.19 0.9 13 Trinity SCIP Data 2009 & Today 14 15 Nurse Driven Urinary Catheter Removal Protocol 16 17 18 Lessons Learned Nurse to Nurse Collaboration is a practiced skill Physician collaboration is key Physician and Nurse communication / education is paramount Adaptive Design and daily monitoring drives successful implementation 19 Conclusion: HAI’s represent a direct threat to patient safety, healthcare quality and they are costly. The Urine-8 project has consistently decreased the infection rate and identified the positive financial impact directly attributed to evidence-based nursing practice. The next step of adding the nurse driven catheter removal protocol will continue to decrease unnecessary Foley days and serve as a tool to meet SCIP criteria and avoid CAUTI. 20