Plasmid-Mediated Quinolone Resistance in Australia
advertisement

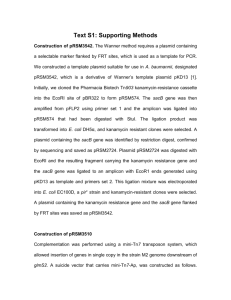
MICROBIAL DRUG RESISTANCE Volume 12, Number 2, 2006 © Mary Ann Liebert, Inc. Plasmid-Mediated Quinolone Resistance in Australia JOSE-MANUEL RODRIGUEZ-MARTINEZ,1,2 LAURENT POIREL,1 ALVARO PASCUAL,2 and PATRICE NORDMANN1 ABSTRACT The aim of this study was to search for plasmid-encoded quinolone resistance determinants QnrA and QnrS in fluoroquinolone-resistant and extended-spectrum -lactamase (ESBL)-producing enterobacterial isolates recovered in Sydney, Australia, in 2002. Twenty-three fluoroquinolone-resistant, of which 16 were also ESBL-positive, enterobacterial and nonrelated isolates were studied. PCR with primers specific for qnrA and qnrS genes and primers specific for a series of ESBL genes were used. A qnrA gene was identified in two ESBL-positive isolates, whereas no qnrS-positive strain was found. The QnrA1 determinant was identified in an Enterobacter cloacae isolate and in a carbapenem-resistant Klebsiella pneumoniae isolate, both of which expressed the same ESBL SHV12. Whereas no plasmid was identified in the E. cloacae isolate, K. pneumoniae K149 possessed two conjugative plasmids, one that harbored the qnrA and blaSHV-12 genes whereas the other expressed the carbapenemase gene blaIMP-4. The qnrA gene, was located in both cases downstream of the orf513 recombinase gene and upstream of the qnrA1 gene, a structure identical to that found in sul1-type integron In36 and qnrA-positive strains from Shanghai, China. However, the gene cassettes of the sul1-type integrons were different. This study identified the first plasmid-mediated quinolone resistance determinant in Enterobacteriaceae in Australia. INTRODUCTION of the QnrA determinant has been identified recently as being the water-borne environmental species Shewanella algae.11 The aim of this study was to determine the prevalence of the qnrA and qnrS genes in clinical isolates recovered in Sydney, Australia, to evaluate further the dissemination of these novel plasmid-mediated quinolone resistance determinants. Q usually results in Enterobacteriaceae from mutations in genes coding for chromosomally encoded type II topoisomerases or for efflux pumps and porins.2,3 However, recent reports indicate that quinolone resistance may be also plasmid mediated.3,9,13 The first plasmid-mediated quinolone resistance protein Qnr (termed recently QnrA) was identified from urine in a Klebsiella pneumoniae isolate from Birmingham, Alabama by L. Martinez-Martinez and G. Jacoby.7 The plasmid-mediated quinolone resistance gene qnrA encodes a 218-amino-acid protein of the pentapeptide family that protects gyrase from quinolone inhibition.14 Recently, another plasmid-mediated quinolone resistance determinant, QnrS, has been reported from Japan.1 Molecular studies showed that the qnrA gene was located with other resistance determinants in sul1-type integrons harboring a duplication of the 3-conserved sequence of integrons and orf513 gene,12,13 this latter gene encoding a putative recombinase involved in site-specific acquisition of resistance genes. Plasmid-mediated determinant QnrA has been identified from remotely related areas, such as the United States, China, Thailand, Korea, Turkey, Germany, and France.9,16 The origin UINOLONE RESISTANCE MATERIALS AND METHODS Bacterial strains Twenty-three ciprofloxacin-resistant nonduplicate enterobacterial strains isolated in 2002 in the metropolitan area of Sydney, Australia, and recovered during a 2-month period from urine samples were studied, including 11 Klebsiella pneumoniae, 8 Escherichia coli, 1 Enterobacter cloacae, 1 Enterobacter agglomerans, 1 Proteus mirabilis and 1 Citrobacter youngae strain. They were randomly taken from the strain collection of the Antibiotic Reference Laboratory, Department of Microbiology, The Prince of Wales Hospital, Randwick, Australia. In addition, previously studied E. coli EC158 and K. pneumoniae K149 strains isolated 1Service de Bactériologie-Virologie, Hôpital de Bicêtre, Assistance Publique/Hôpitaux de Paris, Faculté de Médecine Paris-Sud, Université Paris XI, K.-Bicêtre, France. 2University Hospital Virgen Macarena, University of Sevilla, Sevilla, Spain. 99 100 RODRIGUEZ-MARTINEZ ET AL. in Melbourne in September, 2002, that both produce metallo-lactamase IMP-4 were included in this study.10 Sixteen isolates (69.5%) produced extended-spectrum -lactamases (ESBLs) and were detected as reported.4 E. coli NCTC50192 harboring four plasmids of 154, 66, 38, and 7 kb was used as size marker for plasmids. E. coli J53 AzR was used as the host in the conjugation experiments and E. coli DH10B in the transformation experiments.6 E. coli LO was used as a qnrA1-positive5 and E. coli (pBCH2.6) as qnrS-positive control strains.1 Susceptibility testing MICs for nalidixic acid and fluoroquinolones were determined by an agar dilution technique and interpreted, when available, according to the guidelines of the CLST.8 MICs of -lactams, chloramphenicol, tetracycline, tobramycin, and gentamicin were determined by an agar dilution technique with Mueller-Hinton agar (Sanofi-Diagnostic Pasteur), as described previously.5 PCR amplification Genomic DNAs of bacterial isolates were obtained as described previously.6 PCR experiments were carried out using TABLE 1. specific primers for the qnrA and qnrS genes. Primers QnrAA and QnrA-B5 for the qnrA gene and QnrS-A2 (5-AGT GAT CTC ACC TTC ACC GC-3) and QnrS-B2 (5-CAG GCT GCA ATT TTG ATA CC-3) for the qnrS gene amplifying internal fragments of 661 and 550 bp, respectively, were used. Once the corresponding gene was identified using a series of primers for genes coding for ESBLs,6 primers specific for lactamase gene blaSHV (SHV-A, 5-ATG CGT TAT WTT CGC CTG TGT-3, and SHV-B, 5-TTA GCG TTG CCA GTG CTC G-3) were used in combination with qnrA-specific primers to evaluate a putative colinearity between those genes. The PCR products were sequenced with an Applied Biosystems sequencer (ABI 377). Plasmid and Southern blot analyses Plasmid analysis of the clinical isolates, transconjugants, and transformants was performed by using the Kieser technique,5 followed by an agarose gel electrophoresis analysis. Southern blot analysis was performed using whole-cell DNA restricted with BamHI and NdeI restriction enzymes, agarose gel electrophoresis, and membrane transfer, followed by hybridization using qnrA and blaSHV-12-specific probes.6 QUINOLONE SUSCEPTIBILITY PROFILES OF CLINICAL ISOLATES, TRANSCONJUGANT RECOMBINANT CLONE IN E. coli REFERENCE STRAINS FROM K. pneumoniae K149, AND MICs in mg/L for strainsb Antibioticsa E. cloacae Qn17 qnrA K. pneumoniae K149 (p149) qnrA NAL CIP OFX NFX MFX SPX AMX AMC PIP TZP CAZ CTX FEP IMP TM GM C TET 256 16 32 32 32 32 512 512 64 8 256 32 0.5 0.25 128 128 128 128 32 1 4 2 2 2 512 512 512 128 512 256 64 8 128 128 128 128 E. coli J53 transconjugant (p149)b qnrA 32 0.25 1 1 1 1 512 8 256 4 8 4 2 0.12 4 8 128 128 E. coli J53 AzR E. coli DH10B (p149SN12)c qnrA E. coli DH10B 4 0.12 0.01 0.01 0.03 0.01 4 4 2 1 0.06 0.06 0.01 0.06 NDd ND ND ND 8 0.25 0.5 1 0.5 0.5 512 128 512 128 512 128 32 0.12 ND ND ND ND 2 0.002 0.01 0.01 0.002 0.005 4 4 2 2 0.06 0.06 0.06 0.06 ND ND ND ND aNAL, nalidixic acid; CIP, ciprofloxacin; OFX, ofloxacin; NFX, norfloxacin; MFX, moxifloxacin; SPX, sparfloxacin, AMX, amoxicillin; AMC, amoxicillin-clavulanic acid; PIP, piperacillin; TZP, piperacillin-tazobactam; CAZ, ceftazidime; CTX, cefotaxime; FEP, cefepime; IMP, imipenem; TM, tobramycin; GM, gentamicin; C, chloramphenicol; TET, tetracycline. Breakpoints used for quinolone and fluoroquinolone susceptibility testing were the following: for nalidixic acid, susceptible if MIC 16 mg/L and resistant if MIC 32 mg/L; for ciprofloxacin, moxifloxacin, and sparfloxacin, susceptible if MIC 1 mg/L and resistant if MIC 4 mg/L; for ofloxacin, susceptible if MIC 2 mg/L and resistant if MIC 8 mg/L; for norfloxacin, susceptible if MIC 4 mg/L and resistant if MIC 16 mg/L. bE. coli J53 (p149) transconjugant was obtained from K. pneumoniae K149. cE. coli DH10B (p149SN12) recombinant strain contained a SacI insert expressing the QnrA determinant. dND, Not determined. QNRA DETERMINANT IN AUSTRALIA Conjugation and transformation experiments Transfer of the qnrA1 gene into reference strain E. coli J53 AzR by conjugation was attempted by liquid and solid matingout assays. Transconjugants were selected on trypticase soy (TS) agar plates containing sodium azide (100 mg/L) and amoxicillin (100 mg/L) or chloramphenicol (30 mg/L). In addition, plasmid extracts of qnrA1-positive strains were used for transformation assays in E. coli DH10B, as described, giving rise to transformants selected on plates containing amoxicillin (100 mg/L) or chloramphenicol (30 mg/L).6 Cloning experiments and sequence analysis Cloning experiments were performed with the restriction enzymes SacI or BamHI from whole-cell DNAs extracted as previously described using the vector pBK-CMV, followed by expression of recombinant plasmids in E. coli DH10B and selection on TS agar containing kanamicin (30 mg/L) and nalidixic acid (4 mg/L), gentamicin (8 mg/L), or chloramphenicol (30 mg/L). Antibiograms obtained by disk diffusion were performed with E. coli DH10B harboring recombinant plasmids, and sizes of the plasmid inserts were determined by restriction analysis. Both strands of each recombinant plasmid were sequenced. The nucleotide sequences were analyzed with software available over the internet at the National Center for Biotechnology Information Web site (http://www.ncbi.nlm. nih.gov). RESULTS AND DISCUSSION Retrospective analysis of the antibiotic resistance profile of the SHV-12-positive E. coli transconjugant obtained from K. 101 pneumoniae isolate K149 (IMP-4 and SHV-12 positive) recovered in Australia10 indicated that the transferred plasmid p149 conferred reduced susceptibility to several quinolones whereas the IMP-4-positive plasmid did not. Thus, PCR experiments were performed to screen for the putative qnrA gene that gave a positive result for the K. pneumoniae K149 isolate but not for the IMP-4-positive E. coli EC158 strain recovered during the same period of time. Consequently, a survey was conducted to evaluate prevalence of QnrA and QnrS determinants among a collection of ciprofloxacin-resistant enterobacterial isolates recovered in Melbourne over a 2-month period. This screening gave negative results for the qnrS gene (the first survey of that type), whereas one of the 23 clinical strains analyzed was positive for the qnrA gene (8.7%). This isolate, E. cloacae strain Qn17, was also positive for the blaSHV-12 gene. The nucleotide sequences of the two qnrA-like genes were identical to that of the known qnrA, latter termed qnrA1.9 K. pneumoniae K149 was resistant to ampicillin, ceftazidime, ticarcillin, ticarcillin plus clavulanic acid, imipenem, fosfomycin, tetracycline, chloramphenicol, trimethoprim-sulfamethoxazole, tobramycin, gentamicin, kanamycin, rifampin, and sulfonamides of intermediate susceptibility to nalidixic acid and resistant to fluoroquinolones (Table 1). E. cloacae Qn17 was resistant to amoxicillin, cefotaxime, ceftazidime, tetracycline, chloramphenicol, trimethoprim-sulfamethoxazole, aminoglycosides, rifampin, sulfonamides, nalidixic acid, and fluoroquinolones. Conjugation, plasmid analysis, and Southern hybridization experiments (data not shown) did not identify any plasmid in E. cloacae Qn17, whereas a 160-kb conjugative plasmid was identified in K. pneumoniae K149 that possessed both the qnrA and blaSHV-12 genes. However, PCR mapping did not reveal any co-linearity between those two genes. In addition, PCR combinations with primers specific for a class 1 integron did FIG. 1. Comparison of sul1-type integrons that contain a qnrA gene. The identical structure identified in K. pneumoniae K149 and in E. cloacae Qn17 isolates is indicated in comparison with those of In36 and In37 from Shanghai.14 pMG252 is from the QnrA-positive E. coli strain from Alabama.12 102 RODRIGUEZ-MARTINEZ ET AL. not identify any gene cassette upstream of orf513. Another 150kb plasmid was identified in K. pneumoniae K149, which harbored the carbapenemase gene blaIMP-4 located inside a class 1 integron structure, as reported previously.16 Quinolone resistance was transferred with a conjugation frequency (the number of transconjugants divided by the number of the donor cells) of 5 105. Transconjugant E. coli J53 (p149) containing the qnrA gene displayed resistance to ampicillin, ceftazidime, tetracycline, chloramphenicol, trimethoprim-sulfamethoxazole, tobramycin, and gentamicin. It showed reduced susceptibility to nalidixic acid and fluoroquinolones (Table 1), but susceptibility to sulfonamides. Cloning experiments using DNA from K. pneumoniae K149 gave rise to an E. coli (p149SN12) recombinant strain that showed reduced susceptibility to quinolones (Table 1). Analysis of the sequence of the 3,495-bp insert indicated that qnrA1 was located in a complex In4 family class 1 integron similar to In36,15 with the presence of an ampR gene downstream of qnrA (Fig. 1). The identical fragment was detected in E. cloacae Qn17. However, further PCR mapping did not identify the overall structure of In36 or In37 in both isolates. In particular, PCR failed to detect IS6100 downstream of qnrA, whereas it has been detected in the qnrA-positive integrons In36 and In37.15 This study emphasizes that the QnrA determinants are also found in enterobacterial isolates in the Australian continent. QnrA-like determinants were identified in ESBL-producing enterobacterial isolates, as reported previously.9 It is noteworthy that it has been detected in a carbapenem-resistant K. pneumoniae isolate, emphasizing that some strains may harbor a large pool of resistance genes leading to panresistance. Another interesting feature observed in that study is the possible chromosomal location of the qnrA1 gene in E. cloacae Qn17, suggesting that the qnrA-structure could have integrated into the chromosome of that isolate, possibly by a transposition process, as already suggested.15 ACKNOWLEDGMENTS This work was funded by a grant from the Ministère de l’Education Nationale et de la Recherche (UPRES-EA3539), Université Paris XI, France, and by a grant from the European Community (6th PCRD, LSHM-CT-2003-503335). Strains were kindly provided by the Antibiotic Reference Laboratory, Department of Microbiology, The Prince of Wales Hospital, Randwick NSW. L.P. is a researcher from the INSERM (Paris, France) and J.M.R.M. was a recipient of a travel grant from the Spanish Society for Clinical Microbiology and Infectious Diseases in 2004. REFERENCES 1. Hata, M., M. Suzuki, M. Matsumoto, M. Takahashi, K. Sato, S. Ibe, and K. Sakae. 2005. Cloning of a novel gene for quinolone resistance from a transferable plasmid in Shigella flexneri 2b. Antimicrob. Agents Chemother. 49:801–803. 2. Hooper, D.C. Emerging mechanisms of fluoroquinolone resistance. 2001. Emerg. Infect. Dis. 7:337–341. 3. Jacoby, G.A. 2005. Mechanisms of resistance to quinolones. Clin. Infect. Dis. 41(Suppl. 2):S120–S126. 4. Jarlier, V., M.-H. Nicolas, G. Fournier, and A. Philippon. 1988. Extended broad-spectrum -lactamases conferring transferable resistance to newer -lactam agents in Enterobacteriaceae: hospital prevalence and susceptibility patterns. Rev. Infect. Dis. 10:867– 878. 5. Kieser, T. 1984. Factors affecting the isolation of CCC DNA from Streptomyces lividans and Escherichia coli. Plasmid 12:19–36. 6. Mammeri, H., M. Van De Loo M, L. Poirel, L. Martinez-Martinez, and P. Nordmann. 2005. Emergence of plasmid-mediated quinolone resistance in Escherichia coli in Europe. Antimicrob. Agents Chemother. 49:71–76. 7. Martinez-Martinez, L., A. Pascual, and G.A. Jacoby. 1998. Quinolone resistance from a transferable plasmid. Lancet 351:797–799. 8. National Committee for Clinical Laboratory Standards. 2005. Performance standards for antimicrobial susceptibility testing; fourteenth informational supplement M100–S15. National Committee for Clinical Laboratory Standards, Wayne, PA. 9. Nordmann, P., and L. Poirel. 2005. Emergence of plasmid-mediated quinolone resistance in Enterobacteriaceae. J. Antimicrob. Chemother. 56:52–59. 10. Poirel, L., J.N. Pham, L. Cabanne, B.J. Gatus, S.M. Bell, and P. Nordmann. 2004. Carbapenem-hydrolysing metallo--lactamases from Klebsiella pneumoniae and Escherichia coli isolated in Australia. Pathology 36:366–367. 11. Poirel, L., J.M. Rodriguez-Martinez, H. Mammeri, A. Liard, and P. Nordmann. 2005. Origin of plasmid-mediated quinolone resistance determinant QnrA. Antimicrob. Agents Chemother. 49:3523–3525. 12. Poirel, L., M. Van De Loo, H. Mammeri, and P. Nordmann. 2005. Association of plasmid-mediated resistance with extendedspectrum -lactamase VEB-1. Antimicrob. Agents Chemother. 49:3091–3094. 13. Tran, J.H., and G.A. Jacoby. 2002. Mechanism of plasmid-mediated quinolone resistance. Proc. Natl. Acad. Sci. USA 99:5638– 5642. 14. Tran, J.H., G.A. Jacoby, and D.C. Hooper. 2005. Interaction of the plasmid-encoded quinolone resistance protein Qnr with Escherichia coli DNA gyrase. Antimicrob. Agents Chemother. 49:118–125. 15. Wang, M., D.F. Sahm, G.A. Jacoby, and D.C. Hooper. 2004. Emerging plasmid-mediated quinolone resistance associated with the qnr gene in Klebsiella pneumoniae clinical isolates in the United States. Antimicrob. Agents Chemother. 48:1295–1299. 16. Wang, M., J.H. Tran, G.A. Jacoby, Y. Zhang, F. Wang, and D.C. Hooper. 2003. Plasmid-mediated quinolone resistance in clinical isolates of Escherichia coli from Shanghai, China. Antimicrob. Agents Chemother. 47:2242–2248. Address reprint requests to: Dr. Patrice Nordmann Service de Bactériologie-Virologie Hôpital de Bicêtre 78, rue du Général Leclerc 94275 Le Kremlin-Bicêtre, France E-mail: nordmann.patrice@bct.ap-hop-paris.fr This article has been cited by: 1. Haeng Soon Jeong , Il Kwon Bae , Jeong Hwan Shin , Si Hyun Kim , Chulhun L. Chang , Joseph Jeong , Sunjoo Kim , Chae Hoon Lee , Nam Hee Ryoo , Jeong Nyeo Lee . 2011. Fecal Colonization of Enterobacteriaceae Carrying Plasmid-Mediated Quinolone Resistance Determinants in Korea. Microbial Drug Resistance 17:4, 507-512. [Abstract] [Full Text] [PDF] [PDF Plus] 2. José Manuel Rodríguez-Martínez, María Eliecer Cano, Carmen Velasco, Luis Martínez-Martínez, Álvaro Pascual. 2011. Plasmid-mediated quinolone resistance: an update. Journal of Infection and Chemotherapy 17:2, 149-182. [CrossRef] 3. Justine S. Gibson, Rowland N. Cobbold, Peter Heisig, Hanna E. Sidjabat, Myat T. Kyaw-Tanner, Darren J. Trott. 2010. Identification of Qnr and AAC(6#)-1b-cr plasmid-mediated fluoroquinolone resistance determinants in multidrug-resistant Enterobacter spp. isolated from extraintestinal infections in companion animals. Veterinary Microbiology 143:2-4, 329-336. [CrossRef] 4. J. Sanchez-Cespedes, S. Marti, S. M. Soto, V. Alba, C. Melci##n, M. Almela, F. Marco, J. Vila. 2009. Two chromosomally located qnrB variants, qnrB 6 and the new qnrB 16, in Citrobacter spp . isolates causing bacteraemia. Clinical Microbiology and Infection 15:12, 1132-1138. [CrossRef] 5. L. Meradi, A. Djahoudi, A. Abdi, M. Bouchakour, J.-D. Perrier Gros Claude, M. Timinouni. 2009. Résistance aux quinolones de types qnr, aac (6#)-Ib-cr chez les entérobactéries isolées à Annaba en Algérie. Pathologie Biologie . [CrossRef] 6. Johann DD Pitout. 2008. Multiresistant Enterobacteriaceae: new threat of an old problem. Expert Review of Anti-infective Therapy 6:5, 657-669. [CrossRef] 7. Luis Martínez-Martínez, María Eliecer Cano, José Manuel Rodríguez-Martínez, Jorge Calvo, Álvaro Pascual. 2008. Plasmidmediated quinolone resistance. Expert Review of Anti-infective Therapy 6:5, 685-711. [CrossRef] 8. P. Nordmann, H. Mammeri. 2007. Résistance plasmidique aux quinolones. Antibiotiques 9:4, 246-253. [CrossRef] 9. T SAGA, T AKASAKA, H TAKASE, M TANAKA, K SATO, M KAKU. 2007. First detection of the plasmid-mediated quinolone resistance determinant qnrA in Enterobacteriaceae clinical isolates in Japan. International Journal of Antimicrobial Agents 29:6, 738-739. [CrossRef] 10. Ari Robicsek, George A Jacoby, David C Hooper. 2006. The worldwide emergence of plasmid-mediated quinolone resistance. The Lancet Infectious Diseases 6:10, 629-640. [CrossRef]