Still Thinking Research
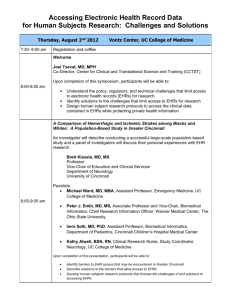
advertisement
0 1 0 0 1 1 1 0 0 0 0 1 1 1 1 0 0 0 0 10 1 0 0 0 0 1 1 0 010 10 10 0 10 0 FasterCures Still Thinking Research Strategies to Advance the Use of Electronic Health Records to Bridge Patient Care and Research Preface FasterCures is not just our name—it's our mission. We are an “action tank” that works to improve the medical research system so that we can speed up the time it takes to get important new medicines from discovery to patients. One of our key strategic objectives is to increase patient engagement in research and optimize use of patient data. For the medical research system to work, it has to be patient-focused, and patient-driven. In fighting disease, patience is not a virtue—patients are. Through our Patients Helping Doctors (PHD) program, we focus our efforts on unlocking patient information—medical records and biological material such as tissue, blood, and DNA—and making it available to clinical researchers in a meaningful way. This report is a central component of the PHD. An update to the 2005 FasterCures Think Research analysis, it continues to call for integrating research into the health information technology framework to achieve earlier and better diagnosis and more effective prevention strategies and cures. This report examines current policies and existing practices, presents a platform for discussion, and provides clear-cut recommendations for action. We thank the team who developed this report—Adam Clark, Ph.D., Kathi E. Hanna, M.S., Ph.D., and Gillian Parrish. And we thank everyone who agreed to be interviewed for their time and, more importantly, for their leadership and contributions to improving the medical research system. TABLE OF CONTENTS 01 06 09 16 Introduction New Developments in Federal Health IT Leveraging Health IT for Networked Research Opportunities Meeting the Challenges: Institutional Pioneers, Innovators, and Transformational Models 27 28 29 36 37 38 Lessons Learned What’s Next: Actions and Opportunities Recommendations for Action In Sum Acknowledgments References Introduction FasterCures has perceived an enormous opportunity emerging from the confluence of three transformative breakthroughs— the completion of the Human Genome Project in 2003, the slow but steady rise in the use of EHRs, and the expansion of health information technology (health IT). But how do we make the most of these developments? How can scientists and clinicians possibly begin to make sense of all the new data from the human genome, for example, without more efficient means of linking these molecular data to other types of data about medicine and health status? The relative effects of single genes on complex diseases, such as cancer, diabetes, mental illness, and heart disease, are often weak. In every clinical encounter between a patient and a healthcare provider, valuable information—personal medical histories, unique genetic backgrounds, lifestyle factors, responses to different treatments—is collected and stored. This information not only improves the quality and coordination of a patient's care, but, when applied appropriately, also holds the key to understanding and managing disease across groups of patients and populations. When clinical information is digitized in the form of an electronic health record (EHR) it becomes more valuable because it can be compared, “It is unacceptable and counter-intuitive that we should not be learning more of medicine, and amassing the state of art of medicine, with every patient encounter. Every clinical encounter is extensive enough so that to ignore what we learn and not apply it to advancing medicine seems to be a wasteful and harmful state. What we need is buy-in so that the default position is that research is run hand-in-hand with every [patient] encounter.” searched, and queried in ways that can benefit the patient, other patients with the same disease or disorder, and the research enterprise, which is aiming to develop better diagnostics and therapies. ISAAC S. KOHANE, M.D., PH.D., PROFESSOR OF PEDIATRICS, HARVARD MEDICAL SCHOOL (MAY 2010) Thus, data from many thousands of people (as many as half a million) may be needed to nail down the size and nature of the effect of certain genes on the development of disease.1 Moreover, as we begin to sort out the relative effects of genes and the environment on health, we need standardized means for comparing and testing hypotheses about disease initiation and progression. This requires researchers to have access to clinical data from large cohorts of patients. The EHR can be the vehicle for capturing these vital data. 1 THINK RESEARCH In 2005, FasterCures urged health systems to “think research” when developing or implementing EHR systems so as not to foreclose a golden opportunity to connect clinical data with research needs.2 To understand the relationships between molecular information and human health, population-based and clinical studies are needed, requiring the generation, storage, and analysis of enormous quantities of epidemiologic, genotypic, and phenotypic data. To understand the connections between genes, proteins, and the environment, sophisticated comparisons must be conducted, and these comparisons cannot be done by hand or by eye or patient by patient. It is the collective observations of hundreds, even thousands, of patients that will shine a light on these associations. In 2005, FasterCures urged health systems to “think research” when developing or implementing EHR systems so as not to foreclose a golden opportunity to connect clinical data with research needs. “Think” “Think” is the motto chosen by Thomas J. Watson while heading the sales and advertising departments at National Cash Register. Watson said, “Thought has been the father of every advance since time began. 'I didn't think' has cost the world millions of dollars.” Watson would bring the motto with him as founder of IBM, where it became the company's philosophy and motto. At the time, FasterCures saw the opportunity for EHRs to not only provide a link between genes and disease, but also to: • Monitor the health of the populations and detect emerging health problems. • Identify populations at risk of disease, or those who might benefit most from therapies. • Assess the usefulness of diagnostic tests and screening programs. • Form hypotheses about disease initiation and progression. • Conduct post-marketing surveillance studies of new drugs to identify adverse events, improve prescribing practices, or make labeling more accurate and complete. • Identify potential study participants for clinical research. 2 STILL THINKING RESEARCH Strategies to Advance the Use of Electronic Health Records to Bridge Patient Care and Research The last item in this list seemed the most immediately promising and feasible in 2005. Recruiting patients to clinical trials is often time consuming and restricted to the site participating in the research study, effectively eliminating many community clinics from enrolling patients in clinical trials. Fewer than one-third of clinical trial sites are able to recruit their original target population within the time specified.3 In fact, a review of cancer clinical trials sponsored by the National Cancer Institute of the National Institutes of Health (NIH) showed that nearly 40 percent of these trials failed to accrue enough patients and, thus, closed without completing the study.4 This not only wastes the time, money, and effort of researchers and drug sponsors, but it also is a disservice to the patients who did enroll in the trial, but whose participation will not advance cancer science or care.5 Information contained in a patient's EHR contains much of the information needed to screen and match a patient to a trial. Relying on clinical information derived from a paper-based research environment is inefficient and impractical in the 21st century. Theoretically, the increasingly widespread development and implementation of EHR systems over the past several years provide an avenue to speed data acquisition and searching, conduct mass computing and sampling, and carry out more Relying on clinical information derived from a paper-based research environment is inefficient and impractical in the 21st century. efficient, effective, and economical clinical trials. In 2005, FasterCures located several pioneers and innovators in the use of EHRs in research. We also identified barriers they had overcome to some extent, but that were still faced by others. Beyond the problem of overall low adoption rates of EHRs across health systems, challenges included: • The art and practice of medicine, which is not uniform. • Reliability and completeness of the EHR. • Limits of administrative and claims databases, which are not responsive to research needs. • Unstructured text. • Integration of practice databases for data mining. • Research regulations governing human subjects research and patient privacy. 3 FasterCures recommended several possible solutions for moving the field forward, such as: • Integrating practice databases for data mining. • Developing more sophisticated abstraction and encryption systems to protect privacy. • Developing database connection tools. • Creating translational systems. • Formulating online informed consent procedures. • Evolving data mining and pattern recognition systems. • Developing interactive patient query programs. • Creating patient databases/warehouses/registries. • Creating directories of clinical databases. Although the horizon has some bright spots, and there is more activity in this area than in 2005, the health IT infrastructure as it exists today is still falling short of its potential to increase understanding of disease progression and advance biomedical innovation. STILL THINKING RESEARCH: ABOUT THIS REPORT In 2010, five years after Think Research, FasterCures decided to check in on the status of the use of EHRs in research to assess whether anyone was, in fact, thinking about and exploiting the research potential of EHRs. FasterCures conducted a number of informational discussions with technology and research experts from across the public, private, government, and academic sectors, and conducted a media and literature review of related material that has appeared over the past five years. We also studied organizations that have developed innovative approaches to gathering, capturing, and using digital clinical data for research purposes. Although the horizon has some bright spots, and there is more activity in this area than in 2005, the health IT infrastructure as it exists today is still falling short of its potential to increase understanding of disease progression and advance biomedical innovation. As the volume of digitized patient data grows, a lack of functionality and user interfaces that allow investigators to interact with and study those data are leading to a host of missed research opportunities. Unless electronic health information systems are set up to behave as integrated laboratories, with the power to collect and analyze research-quality data across systems, this potential will not be met. And as more EHR systems are rolled out, not thinking about how to enable research will cost not millions, but possibly billions of dollars in opportunity costs, not to mention lives lost or shortened by disease. 4 STILL THINKING RESEARCH Strategies to Advance the Use of Electronic Health Records to Bridge Patient Care and Research Responsible access to clinical data by researchers stands to accelerate the discovery and development of new interventions and therapies in ways previously unimaginable.6 Moreover, since 2005, a new trend has emerged that highlights even more the need to use EHRs to bridge patient care and research— the growing recognition of the critical role of translational research. Translational research is the process of applying ideas, insights, and discoveries generated through basic scientific inquiry to the treatment and prevention of human disease—the critical bridge between basic and clinical research. This phase encompasses the bidirectional steps taken between basic and clinical studies to understand how fundamental biology can lead to better understanding of disease and health, and how manifestations of disease and health can inform fundamental understanding of human biology. EHRs can be a critical tool for making these connections in many types of research. This report updates the status of existing and new activities in the realm of EHRs and research, again shines a spotlight on some star performers in the field, and makes several recommendations for the future. It finds that much progress has been made in pushing greater adoption of EHRs in clinical care. Publicly-funded efforts Responsible access to clinical data by researchers stands to accelerate the discovery and development of new interventions and therapies in ways previously unimaginable. are aiming to capitalize on digitized health data and several institutions are pushing the frontiers in this important approach to research; yet there is more work to be done. In developing this report, we found that: • Vendors of new EHR systems are not building research capacity into the architecture. • The clinical research community is not actively involved in or does not have incentives to push for research-friendly EHR systems. • Standards and universal exchange systems still challenge the actual transfer and translation of research-relevant data. • Existing EHR systems are not being leveraged to screen, match, and enroll patients in clinical trials. • The patient community is not fully engaged in or aware of the need to share their clinical data to advance research. 5 We end this report with four recommendations for action: • Clinical trial screening and matching should be included as a measure for “Meaningful Use” of electronic health record systems. • The National Institutes of Health (NIH) should articulate a strategy that will align its programs with the recommendations of the Office of the National Coordinator (ONC) Federal Health IT Strategic Plan. • The ONC should develop an initiative with pilot projects that would create medical research IT modules. “In 2005, there was hope that people would use good information tools and systems to deliver care and advance medicine, and there were— and are—islands of excellence in the use of those tools. With the passage of the HITECH Act, this is no longer just considered a good thing that we should do, but it is expected that within five to ten years, this will become the standard.” • Nationwide Health Information Network (NwHIN) should expand its standards and policies to include clinical research and research centers in the network of information exchange. When implemented, we believe these will provide us with opportunities to create a medical research system that will be able to meet and respond to the needs of patients, and accelerate the process of turning a scientific breakthrough into a life-saving therapy. New Developments in Federal Health IT There has been incredible progress in the adoption of EHRs in the clinical setting from 2005 to 2011. The primary purpose of EHR systems—improved healthcare—is better served as more providers come online. Ideally, patients will JONATHAN WHITE, DIRECTOR OF THE AGENCY FOR HEALTHCARE RESEARCH AND QUALITY'S HIT PORTFOLIO (MAY 2010) benefit from a healthcare system that is integrated across time, professionals, and institutions. The EHR has the potential to recognize the interdependence of the many working parts of the healthcare system to effectively manage the entire continuum of care. These systems, able to communicate across providers, can allow patient information to flow across all components of care, across geographic sites, and across discrete patient care incidents. At the federal level, a number of activities have been under way to promote and facilitate clinical adoption of EHRs, which was advancing slowly in the early part of the last decade. 6 STILL THINKING RESEARCH Strategies to Advance the Use of Electronic Health Records to Bridge Patient Care and Research THE HEALTH INFORMATION TECHNOLOGY FOR ECONOMIC AND CLINICAL HEALTH (HITECH) ACT In 2004, the Office of the National Coordinator for Health Information Technology (ONC) was established to promote the development of a national health IT infrastructure. As a result of the 2009 passage of the HITECH Act—part of the American Recovery and Reinvestment (ARRA) Act—the Department of Health and Human Services (HHS) committed to investing $27 billion in EHR adoption in medical practices across the nation with the goal of having an EHR for every American by 2014. 7 HITECH allows hospitals and healthcare providers to qualify for reimbursements from the Centers for Medicare and Medicaid Services if they adopt EHR systems deemed capable of achieving “meaningful use.” This set of standards and certification criteria, determined by ONC with help from external stakeholders and released in 2010, ensures that EHR systems are capable of performing certain required functions. HHS has instituted incentives to encourage adoption of these EHR systems. For example, physicians and other eligible professionals can qualify for incentive payments totaling as much as $44,000 through Medicare or $63,750 through Medicaid. Hospitals can qualify for millions of dollars of incentive payments for implementing and becoming meaningful users of EHR technology. HITECH included a number of other programs intended to accelerate the adoption of electronic health systems.8 The Beacon Community Cooperative Agreement Program The Beacon Community program provided grants to create demonstration communities that use health IT to achieve measurable improvements in quality and health outcomes so as to demonstrate the ability of health IT to transform the healthcare system. The program funds communities that support the development of secure, private, and accurate EHR systems and health information exchanges to improve care coordination, increase the quality of care, and slow the growth of healthcare spending. health information—for example, medical history, physician notes, laboratory data—is stored in multiple locations making it difficult to consolidate and use for other applications, including research. The Mayo SHARP project is attempting to create a unified EHR that will allow for the exchange of patient information among care providers, government agencies, insurers, and other stakeholders. The Nationwide Health Information Network (NwHIN) The 2005 FasterCures report recommended that the needs of medical researchers be built into individual EHR system architecture, as well as that of the NwHIN. NwHIN, still in development, will create a national common platform for health information exchange across diverse entities to promote a more effective network marketplace. It will be the foundation to build standards, services, and policies to ensure secure health information exchange over the Internet. A group of government agencies along with information exchange organizations are currently establishing exchange networks to test the processes involved in securely exchanging health information among the various participating organizations. The Direct Project, a part of NwHIN, was launched in 2010 as a pilot to demonstrate the successful delivery of specific electronic clinical information through the network across different settings, including primary care providers, specialists, medical centers and hospitals, public health departments, and laboratories. The Nationwide Health Information Network Exchange pilot initiative is demonstrating secure information exchange through specific standards, services, and policies. The exchange network is composed of federal agencies and private organizations with capabilities to exchange such information as: • Summary patient records to gather disability informa- tion through the Social Security Administration. The Strategic Health IT Advanced Research Program (SHARP) SHARP supports research projects on breakthrough advances in health IT that foster adoption, including security, patient support, healthcare applications, and network design, and secondary use of EHR data, for example, for research purposes. One of the signature programs funded through SHARP is a project on the secondary use of health data at the Mayo Clinic. Traditionally, patient electronic • Streamlined transition of health records from active duty personnel in the Department of Defense to veteran status covered by the Veterans Administration (a project called the Joint Lifetime Electronic Health Record Program). • Submission of de-identified quality assessment data to Medicare and Medicaid. • Biosurveillance and reporting to the Centers for Disease Control and Prevention (CDC).9 7 “I was invited to a meeting about building a learning healthcare system for cancer, and was asked to speak about how the ONC's activities are going to create a learning healthcare system. So as more and more data, maybe even information, is available in EHR systems, what are we doing to make that data useful for research? After a few hours of working on my speech it hit me— we aren't; ONC is going to fall short of that goal. So I changed my way of thinking. Everybody is focused right now on getting eligible professionals and hospitals to the state of meaningful use and many can't fathom dealing with other uses of the data on top of that, at least not yet. But my answer is we can't afford not to do this. We are so sub-optimizing and failing to take full advantage of our investment.” DR. CHARLES FRIEDMAN, OFFICE OF THE NATIONAL COORDINATOR FOR HEALTH INFORMATION TECHNOLOGY, HHS (JUNE 2010) 8 STILL THINKING RESEARCH Other federal efforts besides those within the HITECH programs include the CDC's Public Health Informatics and Technology Program. This program is developing a public health standard to align with certified EHR technologies. The standard will allow for the exchange of information among providers, public health agencies, and laboratories for public health reporting and awareness.10 The program also aims to advance the field of public health informatics through applied research and innovation, and program managers are working to create a Public Health Information Network to support exchange and harmonize public health information with the broader national health information network so that electronic health information can be exchanged seamlessly among public health agencies.11 Despite these enormous federal efforts to promote EHR adoption, overall rates of uptake are still low. The estimates on physician adoption vary depending on how the electronic health system is defined, but substantial improvements in the widespread use of EHR systems by the medical community are yet to be achieved. According to recent estimates, approximately four percent of physicians have a comprehensive EHR system and 13 percent have a basic system.12 Similarly, about two percent of hospitals have a comprehensive system and eight percent have a basic system.13 The adoption rates have been slow for a variety of reasons, such as high cost of purchasing an EHR system, change to clinical workflow, lack of incentives or reimbursements, and uncertainty about the features needed for a certified, comprehensive system. As mentioned, the passage of HITECH in 2009 requires EHR systems to meet minimal functionalities in order to be certified, and physicians will receive reimbursements through Medicare and Medicaid to encourage their adoption. Early indications show that this lever to create adoption incentives may be working, as 81 percent of hospitals and 41 percent of office-based physicians have said that they plan to adopt the systems and qualify for the incentive payments.14 * Dr. Friedman was Chief Science Officer at the Office of the National Coordinator for Health Information Technology, HHS from 2009-Summer 2011. He now heads a graduate program in health informatics at the University of Michigan. Strategies to Advance the Use of Electronic Health Records to Bridge Patient Care and Research The value of these efforts to improved health is obvious. However, it is shortsighted if we do not also consider the potential vast benefits such systems could provide clinical researchers. With the majority of systems to date built to focus on reimbursement claims, clinical workflow improvement, and outcomes reporting, their potential use for research continues to be overlooked. As institutions struggle to adopt and implement EHR systems, it is crucial that they consider the needs and seek the advice of the research community and that the research community advocate on its behalf and force its needs into ongoing plans to develop EHR systems. As the political and technological architecture for EHRs continues to solidify, the window of opportunity to capitalize on health IT's promise for research could be getting smaller. If we don't go the extra distance to harness EHRs effectively for learning and research purposes before standards, incentives, and norms are institutionalized, vast stores of information that could be mapped to biology, medicine, and health will remain unconnected and untapped. Leveraging Health IT for Networked Research Opportunities As institutions struggle to adopt and implement EHR systems, it is crucial that they consider the needs and seek the advice of the research community and that the research community advocate on its behalf and force its needs into ongoing plans to develop EHR systems. Fortunately, some people in the public sector have been thinking a lot about how to create national opportunities to link researchers and patients through the EHR and digital databases. Many other possibilities also are on the horizon. A sampling of federally supported efforts and opportunities to use digital health information for research are described below. > THE HEALTH MAINTENANCE ORGANIZATION RESEARCH NETWORK (HMORN) HMORN is a consortium of 16 HMOs with the goal of improving healthcare through various partnerships covering health services, epidemiology, clinical, and behavioral research.15 Funded by NIH, HMORN has developed the Virtual Data Warehouse to connect the 9 network sites and support multi-center research activities. The warehouse uses a federated model to transform data captured in patient EHRs and medical claims databases (such as diagnoses, demographics, medical procedures, tumor grade, and laboratory results) from individual healthcare systems into a standard format available to researchers in the network. This federated model offers an effective mechanism to protect the identity of patients, providers, and health plans while allowing researchers to access relevant medical information through the network.16 For example, the Cancer Research Network, a consortium of collaborators within HMORN, is work- With patient consent, researchers will investigate genetic variants associated with 40 more disease characteristics and symptoms and aim to develop strategies to apply this information to adjust patient treatment strategies. ing on a pilot project in Hawaii that would extract electronic data from the Virtual Data Warehouse and transmit it to the central cancer registry. This will allow investigators to conduct analyses on diagnosis, treatment, comorbidities, and other outcomes associated with cancer.17 > THE DEcIDE (DEVELOPING EVIDENCE TO INFORM DECISIONS ABOUT EFFECTIVENESS) NETWORK The DEcIDE Network is a collection of research centers supported by the Agency for Healthcare Research and Quality (AHRQ) to conduct studies on the outcomes, effectiveness, safety, and usefulness of medical treatments and services. The DEcIDE Network connects research-based health organizations with electronic access to health information databases, thereby enhancing the ability to conduct comparative effectiveness research. In one program within the network, researchers are using a distributed research network (DRN) model to generate evidence on the effects of new treatments and other medical technologies. A DRN model allows observation and study of large populations of patients through routine collection of patient data (demographic, eligibility, and claims) available through EHRs and processed for researcher access and use. One of the groups within the DEcIDE Network is applying this model in a pilot project to assess the comparative effectiveness and safety of various second line anti-hypertensive therapies.18 For example, through this pilot, a researcher may query data 10 STILL THINKING RESEARCH Strategies to Advance the Use of Electronic Health Records to Bridge Patient Care and Research for patients with a diagnosis of hypertension who are given at least one of several anti-hypertensive medications. The researcher could then compare diagnoses with treatments and follow-up occurrences to determine response outcomes and ENHANCING PRIVACY, IMPROVING HEALTH THROUGH RESEARCH assess if there were comparative differences in the medications without knowing the location of the data, how the data are stored, or how the query is distributed. > THE eMERGE (ELECTRONIC MEDICAL RECORDS AND GENOMICS) NETWORK One visionary goal of advanced use of electronic health information is the capability to align de-identified personal health information with genetic information. The eMERGE Network, supported by NIH's National Human Genome Research Institute, aims to develop approaches to linking biorepositories to EHR systems for large-scale genomic sequencing.19 This network is composed of five sites and supported through an administrative coordinating center. Each site has its own biorepository and uses a common genotyping platform to sequence the DNA samples from the specimens. The first phase of the project demonstrated that data contained in patient EHRs can be used with patients’ genetic information in large scale studies. The eMERGE Network has already identified genetic variants associated with dementia, cataracts, high-density lipoprotein (HDL) cholesterol, peripheral arterial disease, white blood cell count, type 2 diabetes and cardiac conduction defects.20 The eMERGE Network is now moving into its second phase of development by expanding the use of genomic information in clinical research and care. With patient consent, researchers will investigate genetic variants associated with 40 more disease characteristics and symptoms and aim to develop strategies to apply this information to adjust patient treatment strategies. Although the network is still learning the challenges of sharing information in a research network, particularly with regard to the quality of data captured in an EHR versus the quality needed for “researchgrade” analyses, it has developed approaches to share de-identified genetic and patient medical information through the net- In 2009, the Institute of Medicine (IOM) released a report evaluating the impact of the Health Insurance Portability and Accountability Act of 1996 Privacy Rule on research. The purpose of the HIPAA Privacy Rule is to protect an individual's personally identifiable health information and ensure that health insurance is portable, that is, not necessarily linked to or dependent on employment. The IOM committee responsible for the review concluded that the Privacy Rule not only does not protect privacy as well as it should, but also, as currently implemented, impedes important health research. The report called for a new approach to protecting privacy that would harmonize existing regulations and apply them uniformly to all health research. IOM supported making distinctions between information-based research (such as electronic medical data or stored biological specimens) and interventional research involving active patient participation in an experimental treatment setting. In arguing for the need to improve researcher access to medical and health information, the report stated that “If society seeks to derive the benefits of medical research in the form of improved health and healthcare, information should be shared to achieve the greater good, and governing regulations should support the use of such information, with appropriate oversight.” 21 work and are leading efforts to ensure privacy and address public concerns regarding the use of genomic information. 11 > THE INFORMATICS FOR INTEGRATING BIOLOGY AND THE BEDSIDE (I2B2) PROGRAM i2b2, based out of the Partners HealthCare System in Boston, was funded by NIH as part of its 2004 Roadmap Initiative to provide researchers access to medical and research databases through a public portal.22 The goal of i2b2 is to support exchange of clinical and research information among participating organizations and entities to drive research studies and hypothesis generation. The goal of i2b2 is to support exchange of clinical and research information among participating organizations and entities to drive research studies and hypothesis generation. The i2b2 platform bridges clinical data with research data, such as genomics databases,23 across institutions into an integrated database. i2b2 uses computational tools to de-identify electronic patient records by removing private health information while still preserving clinical information. This enables clinical researchers to use existing patient records for discovery research and hypotheses generation and testing. It allows researchers to query the database to find smaller subsets of patients of interest (e.g., patients who did not respond to a standard line of therapy) for further research studies. It also can allow a researcher to investigate deeper into the phenotype of certain sets of patients to support genomic, outcome, or environmental studies. I2B2 SUCCESS STORIES 12 • Partners HealthCare researchers used data extracted from 9,000 patient EHRs in i2b2 to create a model for predicting chronic obstructive pulmonary disease in certain asthma patients.24 • Partners HealthCare's Driving Biology Projects is using i2b2 to look for genotypes from asthma patients who are unresponsive to conventional medication to determine whether they have a different genetic background resulting in the lack of response. STILL THINKING RESEARCH • Researchers at the University of Utah are testing capabilities of i2b2 as an open source tool for bench-to-bed-side research conducted outside the Partners HealthCare network. They tested the i2b2 platform to see if it was suitable for identifying potential patient cohorts based on clinical information contained in the EHR, for example, demographics, laboratory test results, medication lists, and diagnostic data. The researchers found that 44 percent of research data requests could be captured through the i2b2, providing a useful patient cohort selection tool.25 Strategies to Advance the Use of Electronic Health Records to Bridge Patient Care and Research > NIH'S BIOMEDICAL TRANSLATIONAL RESEARCH INFORMATION SYSTEM (BTRIS) BTRIS is a repository developed from a complex network of information systems supporting clinical care and research data collection from NIH-sponsored clinical trials conducted by the NIH Clinical Center and the agency's intramural research program. BTRIS functionality is twofold. It can provide an individual clinical investigator with access to identifiable data for patients on his or her own study protocols, and it can also provide all NIH investigators with access to de-identified data across all protocols. BTRIS will give investigators easy access to vast amounts of data, such as demographics, vital signs, laboratory test results, and medication history and allow researchers to generate reports across clinical trials. > THE BIOMEDICAL RESEARCH INTEGRATED DOMAIN GROUP (BRIDG) The BRIDG project is a collaborative public-private initiative to develop a shared model that supports clinical research across IT platforms. The BRIDG model was first released in 2007 and has been used to support interoperability across applications developed by By harmonizing existing standards, the BRIDG model can remove barriers that limit clinical and translational research. It demonstrated practical success in its early implementation with the Clinical Trials Management System interoperability project. the National Cancer Institute's Cancer Bioinformatics Grid (caBIG). By harmonizing existing standards, the BRIDG model can remove barriers that limit clinical and translational research. It demonstrated practical success in its early implementation with the Clinical Trials Management System interoperability project. In this demonstration, data were successfully exchanged across clinical trials management systems that supported the registration of a patient to the trial, the import of laboratory data related to that patient, and evaluation of the laboratory data to report any potential adverse events related to the trial.26 > THE FDA SENTINEL INITIATIVE The U.S. Food and Drug Administration (FDA) Sentinel Initiative was launched in 2008 as a surveillance system to monitor FDA-regulated products through electronic healthcare data.27 The Sentinel System allows FDA to monitor the safety of drugs and medical products 13 through data captured at academic medical centers, healthcare systems, federal agencies, and insurance companies. Sentinel uses a “distributed data system” in which the initial electronic patient data are housed at their existing secure environments—not in one database. In this system, the data are processed and sent to an FDA coordinating center to answer specific safety questions. By July 2010, FDA had built the framework for active, near real-time safety surveillance to monitor data from electronic healthcare systems for 25 million people, with a goal of 100 million people by 2012. Because the system is built on EHR platforms, it also will be able to identify health events that occur For many academic investigators involved in clinical research, electronic data capture system setup for case report forms and clinical data management may be expensive and possibly prohibitive to conducting research. commonly in the general population (e.g., heart attacks) but that are not normally reported to FDA as an adverse event, when, in fact, the event may actually be related to the drug. > NIH'S CLINICAL AND TRANSLATIONAL SCIENCE AWARDS Within the clinical research spectrum, a promising translational research network, called the Clinical and Translational Science Awards (CTSA), is underway. Adoption of a nationwide information exchange platform aligned with research standards stands to benefit this network greatly. Begun in 2006 as part of the NIH Roadmap, the CTSA program now funds nearly 60 centers, each with its own program, but with an agreement to bridge the gap between basic and clinical research by partnering as a network of networks. Collecting, submitting, and securely sharing research data across sites and within collaborations is a difficult but important functionality for research systems. Among the strategic priorities outlined by the CTSA centers is a goal to enhance collaborations by creating a data-sharing network among the sites.28 Compatible and interoperable EHR systems could assist with research collaboration, patient recruitment into clinical trials, and retrospective studies across the network of CTSA sites.29 However, the lack of common standards, data elements, and application interfaces make networked research studies a challenge. A number of CTSA sites are developing platforms to overcome some of these barriers and transform the goal into a reality. 14 STILL THINKING RESEARCH Strategies to Advance the Use of Electronic Health Records to Bridge Patient Care and Research Although the CTSA sites are not connected tion of EHRs and health IT within the CTSA net- through an integrated and interoperable infor- work would allow for nationwide comparative mation exchange network, a number of sites effectiveness research to be conducted, and also have deployed technologies to improve such allow findings from such studies to be embedded research collaborations. and efficiently disseminated through EHR-based clinical decision support to improve care.32 For example, The Ohio State University CTSA is developing the Translational Informatics and Data Additionally, a Research Electronic Data Capture Management Grid (TRIAD), a “middleware” grid (REDCap) Web-based software application has system. In this grid system, TRIAD provides an been adopted by a number of sites within the interoperable service infrastructure to allow CTSA network. Vanderbilt University initially different researchers using different applications developed REDCap to support data capture to interact with the grid. If successfully adopted, for clinical and translational research studies.33 TRIAD would provide a platform capable of sup- For many academic investigators involved in porting exchange, management, and integration clinical research, electronic data capture system of research data across participating CTSAs. setup for case report forms and clinical data 30 management may be expensive and possibly Another collaborative effort of the CTSA network prohibitive to conducting research. REDCap is a Web-based portal called ResearchMatch. This was designed to support workflow methods tool allows patients interested in medical research for electronic data capture tools needed for to register for studies and matches them to appro- collecting, storing, and disseminating project- priate investigators involved in clinical research. specific research data to enable collaborative 31 studies. Since its pilot launch for collaborative The CTSAs also have a rare capability to leverage network research projects in 2006, REDCap has health IT for national comparative effectiveness grown to support more than 15,000 research research efforts. The proper adoption and applica- projects across the world.34 CTSA SUCCESS STORY: CAPTURING RADIOLOGY IMAGES TO IMPROVE BREAST CANCER DIAGNOSIS Researchers at the University of Pittsburgh's Clinical and Translational Science Institute built an open source software program called Diamond that could rapidly scan large volumes of clinical data to identify and filter specific items within a patient record, such as clinical radiology images.35 In pilot testing, this program was able to assemble a mammogram reference database of more than 4,000 suspected breast mass regions using an interactive search-assisted diagnosis system. The program separated the images into histologically confirmed malignances, benign masses, and false positive mass regions. The program can efficiently acompare mammograms with the reference database and intelligently structure the search to improve accuracy of breast cancer diagnosis. 15 Meeting the Challenges: Institutional Pioneers, Innovators, and Transformational Models We would accomplish many more things if we did not think of them as impossible. In the 2005 Think Research report, FasterCures profiled a number of public and private systems that were at the forefront of EHR implementation at the time. In many cases, these systems also were spearheading attempts to integrate clinical practice data with research goals. In 2005, forwardthinking clinical investigators from the profiled organizations— VINCE LOMBARDI ranging from private systems such as the Mayo Clinic and the Geisinger Health System to public systems such as the Indian Health Service and the Veterans Health Administration— already were pioneering ways to safely use the information stored in early stage EHRs and patient data warehouses for relevant clinical studies. 85 percent Since then, technology has improved and become more widespread, incentives to implement EHRs have been established and applied, and patients have begun to take a more active Patients understand the value of health data in clinical research to discover and develop new treatments and improve care. A 2009 national opinion poll found that 85 percent of respondents felt that it was important that a nationally coordinated health IT system allow investigators to learn from data to facilitate research and track disease. 36 Most recent surveys have shown strong public support for patients to share their anonymized personal health information with researchers. The survey responses ranged from 63 to 80 percent in support of sharing this information. 37, 38 role in tracking and managing their data. These developments have opened the doors to new means for using clinical and health data in research. The following case studies were selected because each model demonstrates the value of the EHR to research. HEALTHCARE SYSTEM MODELS In many senses, Geisinger Health System, Kaiser Permanente, and the Mayo Clinic are the grandparents of health IT and its use in clinical and research practice. All three systems have been at the leading edge of EHR adoption and, early on, found ways to integrate clinical and research use of electronic data. Each has the benefit of having a “captive patient population” or closed system in which loyalty can be built, trust established, and concerns about privacy and confidentiality averted. 16 STILL THINKING RESEARCH Strategies to Advance the Use of Electronic Health Records to Bridge Patient Care and Research GEISINGER HEALTH SYSTEM: Longevity and Loyalty of the Patient Population is Key Geisinger Health System, an integrated health services organization comprised of three medical center campuses, a 700-member group practice, a nonprofit health insurance company, and a Center for Health Research, was an early pioneer in the emerging EHR movement. The 2005 report, Think Research, highlighted two interactive software programs being piloted by Geisinger that aimed to use the organization's EHR to improve care for patients with chronic heart disease and autism. What started out as a system primarily designed to improve the delivery of care has since extended its reach to empower clinical research as well. Today, Geisinger's EHR database contains information on more than three million patients spread across central and northeastern Pennsylvania—nearly 70,000 of whom also use the patient portal, MyGeisinger, to securely access their problem list, medications, allergies, immunizations, and test results. Patients' EHR records are accessed by clinicians for inpatient and outpatient care management, as well as by investigators who identify and enroll thousands of outpatients with common chronic conditions (e.g., diabetes, arthritis, vascular disease) in clinical trials. The typical recruitment process involves writing unsolicited letters to patients who appear to meet broad inclusion/exclusion criteria based on a preliminary review of their EHR—usually from a doctor or nurse who has been involved in that patient's care—and urging interested respondents to opt in to the project. “The challenge for us today is that most industry sponsors are ill-equipped to take advantage of the unique research opportunities a system like Geisinger's can offer,” says Dr. Peter Berger, director of Geisinger's Center for Clinical Studies. “We have a fairly benevolent patient population in Pennsylvania, and typically see response rates in the neighborhood of 30 to 50 percent, which is incredibly high for industry standards.” Another unique aspect of Geisinger's system is the low inward and outward migration rate among its patients. In the more than 14 years that the system has had automated records, Geisinger researchers have been able to keep and track a significant amount of longitudinal data, allowing for the discovery of trends and the measurement of disease impact on various patient populations. “We know, for example, that patients who are very overweight are at risk of developing sleep apnea,” said Berger, “because we reached out to patients via our EHR who we knew had a high BMI and asked them to voluntarily answer four questions related to assessing the symptoms of sleep apnea. Respondents were then invited to undergo a sleep study, and a high percentage were diagnosed with the disease who may not have otherwise known about it until symptoms began to appear.” Efforts also are currently underway at Geisinger to build a repository of blood samples (DNA and serum) called Geisinger MyCode™. According to the Web site, sample collection focuses on primary care patients. MyCode™ is intended to serve as a resource for research that combines information obtained from DNA and serum with health information from the EHR and other sources intended to improve the prevention, diagnosis, and treatment of disease. The blood samples—5,500 of which have already been banked—will be stored so that they can be used for a wide range of biochemical and genetic research for many years in the future. Another 14,520 consents for blood to be drawn have been collected, and additional samples are being gathered. 17 KAISER PERMANENTE HEALTHCONNECT ® : Taking Advantage of a Large, Integrated Clinical Network When FasterCures first profiled Kaiser Permanente (KP) HealthConnect® in 2005, it was already two years into development, with several billion dollars invested in automating records for the organization's then 8.4 million members across the country. At the time, Dean Sittig of the Applied Research in Medical Informatics Group said that Kaiser Permanente planned to use Epic Systems' software and technology services to not only integrate patient clinical records with appointment, scheduling, registration, and billing systems across all of the healthcare system's eight regions, but also to capture unstructured data for research exercises such as planning studies, patient care modeling, outcomes tracking, disease management, post-marketing surveillance, identification of genetic factors, and testing of exploratory data analyses. Five years later KP HealthConnect® is living up to its vision. In March 2010, Kaiser Permanente completed the implementation of what is now the largest private deployment of an EHR system in the world. It securely connects 8.8 million members to their healthcare teams, including more than 100,000 physicians, nurses, and care administrators in 431 medical facilities and 35 hospitals across the country. It is also deploying its system for research purposes. disease, cancer, diabetes, high blood pressure, Alzheimer's disease, asthma, and many others. Based on the 3.3 million-member Kaiser Permanente Medical Care Plan of Northern California, the completed resource will link together comprehensive EHRs, data on relevant behavioral and environmental factors, and biobank data (genetic information from saliva and blood) from 500,000 consenting health plan members. KP HealthConnect is the foundation for the RPGEH. • All of Kaiser Permanente's eight regions currently maintain disease registries (mainly for chronic conditions such as diabetes, hypertension, heart disease, asthma) which collect de-identified information from KP HealthConnect® and use it to generate information about population health that can be applied on a reliable basis. For example: • Kaiser Permanente is building one of the world's largest DNA databases to advance clinical research, the Research Program on Genes, Environment, and Health (RPGEH)—which allows scientists to study the genetic and environmental factors that influence common conditions such as heart 18 STILL THINKING RESEARCH Strategies to Advance the Use of Electronic Health Records to Bridge Patient Care and Research MAYO CLINIC: Setting Data Standards Long a pioneer in the use of automated records, Mayo's medical records are among the most comprehensive in the world, providing the depth necessary to enable a wide range of medical studies. The EHR system is designed to allow Mayo's researchers to efficiently search more than 6.5 million patient records by condition, date of treatment, physician name, and test category, in order to quickly find and leverage information that supports research efforts. What started as a data-warehousing model in collaboration with IBM has evolved into a complex system that incorporates new techniques for harnessing patient data to improve diagnoses, find cures, and individualize care. To address the need for shared vocabulary and systematic capturing of meta-data for complicated research queries, Mayo created the Enterprise Data Trust (EDT), a repository built using the HL7 Reference Information Model and CDISC's BRIDG project. “What differentiates the Mayo EDT from similar clinical data repositories at peer academic health centers is our focus on data governance,” said Dr. Christopher Chute, head of the Division of Biomedical Informatics at the Mayo Clinic. “We established a political process within the organization which aligned with extramural standards.” • Mayo will use NIH's eMERGE Network to identify novel genetic determinants of atherosclerotic vascular disease in order to help identify high-risk subjects who would benefit from aggressive intervention to prevent peripheral arterial disease (PAD). Using data captured in the Mayo EHR, researchers will investigate how gene-environment interactions influence susceptibility to PAD (for example, does/how does smoking modify the observation between genotype and atherosclerotic vascular disease phenotypes), and look for pathways that may serve as targets for new therapies. • Through HHS's SHARP program, and collaborating with Harvard University, the University of Texas Health Science Center at Houston, and the University of Illinois at Urbana-Champaign, Mayo is working to identify short- and long-term solutions to key challenges in health information exchange. Mayo's role focuses on promoting the secondary use of EHR data while maintaining privacy and security, including developing strategies to address natural language processing and data normalization pipelines; improving clinical notes; and expanding high-throughput phenotyping (by compiling a library of standard phenotyping). The goal is to integrate findings into medical practice quickly across the nation. 19 PACeR: A State-Level, Integrated Business Model for Electronic Research THE PARTNERSHIP TO ADVANCE CLINICAL ELECTRONIC RESEARCH (PACeR) was launched as an electronic clinical research data network in New York State to more efficiently identify candidates for clinical research studies and manage their care.39 PACeR sought to build a model that recommends solutions to technical, legal, regulatory, economic, and operational issues in recruiting patients for clinical research studies in the state. The goal of PACeR is to improve patient care and the research missions of participating institutions while improving the efficiency and integrity of clinical research across the network. The PACeR network includes academic medical centers, community hospitals, pharmaceutical companies, researchers, technology developers, state entities, and patient representatives. The Healthcare Association of New York State serves as the neutral partner and coordinator, bringing multiple entities together to drive a “market-based” approach to clinical research networks. In doing so, PACeR aligned its objectives to match investments and programs developing under the HITECH Act as well as FDA initiatives for safety surveillance and monitoring of adverse events. PACeR aligned its objectives to match investments and programs developing under the HITECH Act as well as FDA initiatives for safety surveillance and monitoring of adverse events. groups are currently under way establishing process flows for querying research protocols for patient identification for trial eligibility and closing the “data gap” across institutions. PACeR is designing demonstration projects to address many of these barriers and develop an infrastructure for a clinical research data network in New York. Initial estimates suggest that PACeR's protocol modeling alone may produce more than $50 million annually in revenue by providing one-stop access to higher quality clinical data, a large statewide population of eligible patients, and institution-specific understanding of patient availability. In addition, due to the efficiencies in patient enrollment and earlier product launch, the program estimates millions in potential savings for clinical trial sponsors using the network. In its initial phase, PACeR identified barriers to the secondary use of electronic health data for clinical research capabilities and developed recommendations to address those barriers. For example, the organization found that there are significant gaps in the design of current EHR systems to support clinical research that meets FDA requirements for data submission. These systems also lacked standard terminology within software applications across providers, making data collection and exchange inconsistent. PACeR working 20 STILL THINKING RESEARCH Strategies to Advance the Use of Electronic Health Records to Bridge Patient Care and Research PATIENT-CENTERED AND DIRECTED EFFORTS plans and the desire to have some measure of New models are emerging in health IT, taking control over not only one's personal health advantage of growing consumer savvy about and information but also how it can be used to comfort with Web-based, self-managed health promote research. MICROSOFT HEALTHVAULT Launched in October 2008, MICROSOFT HEALTHVAULT is a privacy- and security-enhanced online service designed to give patients access to and control over their health information and allow them to share it with trusted entities. HealthVault can be used to store copies of individual and family health records obtained from providers, laboratories, health plans, and pharmacies; exchange data with health and fitness applications; and upload data from medical devices. Account holders may also be authorized to access records for multiple individuals, so that a woman, for example, could manage records for each of her children as well as an ailing parent. Users are typically introduced to HealthVault through one of the many applications that talk to the HealthVault platform. These applications are built in collaboration with healthcare companies, nonprofit patient organizations, and device manufacturers. They address everything from managing chronic conditions such as obesity, asthma, and diabetes; understanding and addressing diagnoses such as cancer and heart disease; and tracking lifestyle and fitness choices. formats, including industry standards such as the Continuity of Care Document and the Continuity of Care Record. Although HealthVault is primarily a tool for coordinating and informing prevention and disease management information based on consolidated, personalized health data, it also can be used as a clinical research resource through applications that offer opportunities for account holders to voluntarily engage in research initiatives. For example, TrialX (from Applied Informatics, Inc.) automatically matches participants to clinical trials based on their personal health information. TrialX uses an up-to-date database of more than 25,000 trials approved by FDA. When an individual first uses a HealthVault application, he or she is asked to authorize the application to access a specific set of data types, and those data types are the only ones the application can use. HealthVault supports a number of data exchange 21 THE LOVE/AVON ARMY OF WOMEN In 2008, the DR. SUSAN LOVE RESEARCH FOUNDATION partnered with the AVON FOUNDATION FOR WOMEN to launch the Love/Avon Army of Women, an online initiative that aims to recruit one million women of every age, ethnicity, and breast cancer history to take part in breast cancer research. As of October 2010, more than 340,000 women had signed up, 44,000 of whom already have participated in more than 35 studies. study undergoes a rigorous scientific, safety, and ethical review. Investigators agree to follow Health Insurance Portability and Accountability Act (HIPAA) guidelines to protect the confidentiality of study participants. Investigators also agree to create two Webcasts, blogs, or videos for the Web site's Town Hall feature, which explain the rationale of their research and summarize findings after the study is completed. Women who are interested in participating register on the Love/Avon Army of Women Web site, providing basic information. They then receive email updates announcing new research studies and if they fit the criteria and want to participate, can click on a “sign me up” button that connects them to study investigators for screening. Though not a traditional EHR-based initiative, the Army of Women has found a simple and elegant way of using technology to collect data and advance research. “In terms of research and medical care, we are very behind in utilizing the latest technology that is otherwise available in other enterprises,” says Naz Sykes, executive director of the Dr. Susan Love Research Foundation. “We need to make technology an accessible partner in our quest to find the cause of many diseases.” Scientists (academic, industry, nonprofit, and others) must apply for the opportunity to recruit volunteers, and each PATIENTSLIKEME.COM PATIENTSLIKEME is a privately funded company dedi- cated to providing patients who have life-changing illnesses with access to tools, information, and experiences to take control of their disease. Co-founded in 2004 by MIT engineer Jamie Heywood after his brother Stephen was diagnosed with amyotrophic lateral sclerosis (ALS), this unique platform enables patients to see and share outcomes-based data about their diseases in real time with individuals who have similar conditions and with scientists working to find cures for those conditions. The architecture creates a systems model that helps: • Clinical researchers know whether their work has modified outcomes • Clinicians know what is wrong with a patient and how to approach treatment • Patients know what information is collected about them and why Today, tens of thousands of patients with a wide variety of conditions use PatientsLikeMe to better manage their over- 22 STILL THINKING RESEARCH all health, treatments, and symptoms, and to contribute to the overall research effort. PatientsLikeMe's technology creates the equivalent of tags from patients to structure phenotypes in much the same way that the Web creates hyperlinks between documents. This allows the relationships between tags to be studied and a holistic picture of the impact of a disease to be assembled. Patients who willingly share their experiences and data through the site do so with the knowledge that it will be available in de-identified, aggregated, and individual formats to investigators and scientists studying their disease. “The reason traditional electronic health records are not advancing research in the way they could be is that we're essentially asking monopolistic, private systems to generate information sharing tools that will undercut their own value,” says Heywood. “What we need to do is find a way to create a viable competitive market for information.” Strategies to Advance the Use of Electronic Health Records to Bridge Patient Care and Research RESEARCH REGISTRIES Research registries can provide a warehouse of information that can be queried, tapped, and analyzed by researchers looking for associations among events, conditions, treatments, or genes that might contribute to the development and progression of disease. They can be established retrospectively (i.e., drawing off existing records) or established prospectively and in real time. Some 66 percent A recent survey from the Genetics and Public Policy Center found that 93 percent of respondents support the use of genetic testing by doctors to identify a patient's risk of “having a bad reaction to a particular drug” and an equal percentage support use of genetic data by researchers “to find new ways to diagnose, prevent, or treat disease.” In this same survey, 66 percent of respondents would trust researchers to have access to the genetic test results. These results suggest a growing consumer/patient awareness of the use of genetic information to improve care and discover new treatments, the hallmark of bench-to-bedside-to-bench research. Since the publication of Think Research in 2005, the Genetic Information Non-Discrimination Act of 2008 was passed, providing protection for most individuals to have the results of genetic testing included as part of their medical record without fear that such information could be used against them by employers or insurers. examples appear below. GENE PARTNERSHIP PROJECT: Children's Hospital Boston THE GENE PARTNERSHIP PROJECT (GPP) , a new model for recruiting patients into genomics research, was launched in 2009 in the Developmental Medicine Center and the Manton Center for Orphan Disease Research at Children's Hospital Boston. Though still in its pilot phase, the project's goal is to eventually provide an opportunity for all patients entering the hospital and their families to take part in genetic research as an active participant. Patients who opt in will get a lifelong EHR, called Indivo, that is under their personal control (or, if younger than age 18 years, that of a guardian). They will be asked to provide a DNA sample, which will be entered into a central repository, and to enroll in a registry, giving researchers permission to include them in studies. According to GPP's principal investigator and director of the Children's Hospital Informatics Program, Dr. Isaac Kohane, this approach will maximize the significance of research findings by studying large populations of patients, capturing all available phenotype and environmental information and, most importantly, giving relevant findings back to patients as they become available. The GPP currently has more than 600 participants enrolled in the pilot program, including patients, their siblings, and their guardians. Rather than asking participants to donate DNA samples through a blanket consent form, the project seeks to build “informed cohorts”— large groups of subjects who are engaged and informed about the research in which they are participating. “Starting in childhood gives us a unique opportunity to identify the effects of genetic variants before environmental exposures and lifestyle habits alter the picture,” says Kohane. “By demystifying the research process and increasing trust, we hope to improve patient willingness to volunteer for studies.” 23 RESEARCH PATIENT DATA REGISTRY (RPDR): Partners HealthCare RPDR AT PARTNERS HEALTHCARE is a centralized clinical data registry that gathers data from various hospital legacy systems and stores it in one place. Researchers are able to access these data using an online query tool that provides access to aggregate totals of patients with user-defined characteristics (such as diagnoses, procedures, and/or laboratory results) and, with proper Institutional Review Board (IRB) approval, medical record data as well. Many people view the RPDR as one of the first bestpractice models in medical informatics and research data mining. Its operations are tightly integrated with an IRB, and the data available to researchers are filtered with two-way anonymization as they are included in the system, so that records can be searched with identifiable patient data when necessary, pending IRB approval. Originally designed for the research community, the RPDR is technically and operationally compliant with HIPAA. According to Dr. Shawn Murphy, associate director of the Laboratory of Computer Science at Massachusetts General Hospital (MGH), MGH has conducted return on investment research based on current usage patterns and found that of the 600 to 700 studies conducted at the hospital each year, about 30 percent find the RPDR critical to their research. Murphy also noted that about half of the investigators using the RPDR do so primarily for recruiting patients into clinical trials, but that another handful of newer use cases have been tested and are beginning to take root. 24 STILL THINKING RESEARCH These include: • Data mining Using the data within the RPDR itself to establish data-mining paradigms (e.g., usage patterns of providers, medication recommendation frequency and context) and conduct cutting-edge comparative effectiveness research (e.g., does one treatment/device provide better pain relief?) • Surveillance applications Post-market analysis of whether or how an FDAapproved medication is causing untoward effects not demonstrated in a phase 3 study • Genomic research Repurposing samples collected in the course of clinical care for research purposes and de-identified for research use. In a paper published in 2010 by Arthritis Care & Research, Murphy and his research team reported that they were successfully able to use complete EHR data to define a rheumatoid arthritis cohort with a positive predictive value of 94 percent, which was superior to an algorithm using codified data alone. 40 Strategies to Advance the Use of Electronic Health Records to Bridge Patient Care and Research THE SHARED HEALTH RESEARCH INFORMATION NETWORK (SHRINE): A Prototype Federated Query Tool for Clinical Data Repositories Using NIH CTSA funds, Harvard Medical School has been developing a working prototype of a query tool that would be able to search the clinical data repositories of its three largest health centers—Beth Israel Deaconess Medical Center, Children's Hospital Boston, and Partners HealthCare System (PHS). The lessons learned in creating the SHRINE prototype are now being used as a road map for other institutions developing their own clinical data repositories, or integrating existing databases. The plan is ultimately to replace the system with a scalable peer-to-peer architecture and a streamlined IRB process. Given that each of these institutions operates independently—with its own financial organizations, databases, firewalls, access policies, and IRB— Harvard determined that a combined data warehouse would not be an effective solution. Instead, a federated model was developed through which each institution could manage and maintain control over its local databases, but still issue distributed queries through a standard Web service. Qualified investigators can use the SHRINE Web-based query tool to determine the aggregate total number of patients at participating hospitals who meet a given set of inclusion and exclusion criteria for clinical studies (e.g., demographics, diagnoses, medications, and selected laboratory values). Because counts are aggregate, patient privacy is protected. These data will be most useful for investigators interested in: • Generating new research hypotheses • Conducting research requiring large sample sizes not easily available at any single institution • Preparing grant applications that would benefit from pre-identification and/or characterization of a potential research cohort • Identifying potential cohorts for clinical trials 25 CLINICAL TRIAL ALERT (CTA) SYSTEMS For diseases such as cancer, the overwhelming majority of patients are treated in the community setting where 20 to 40 percent may be eligible for participation in a clinical trial.41 However, the National Cancer Institute has found that only approximately 3 percent of adult cancer patients participate in a trial.42 An Institute of Medicine study found that only 60 percent of National Cancer Institute-sponsored phase 3 trials are completed and published, with slow accrual or insufficient accrual of patients being a reason.43 In 2010, NIH spent an estimated $3.3 billion dollars on clinical trials. 44 This failure to complete a trial is a tremendous waste of clinical time, financial resources, and ultimately the patients' participation and contribution to advance medical research. A patient may not participate in a trial for a variety of reasons, including lack of physician awareness of the trial and the patient's eligibility. In order to overcome this barrier, the Institute of Medicine recommended that tools be developed to “cue” physicians through EHR systems that a patient may be eligible for a trial.45 A Clinical Trial Alert (CTA) is a tool used to query the EHR for matches to ongoing trials and notify the physician of a match at the point of care with the patient. Such systems have been shown to increase physician referrals to a trial by 10-fold and double the enrollment rate.46 Because these alert systems are activated at the point of care, they also may prevent the patient from undergoing initial therapies that may prevent them from qualifying for the trial. Upon enrollment in a clinical trial, an EHR also will have the ability to signal a patient's primary care team or other care coordinators of participation in the trial, accelerating identification of adverse events rather than identifying and reporting events only when the patient visits the clinical investigator. 26 STILL THINKING RESEARCH CLINICAL TRIAL ALERT SUCCESS STORIES • The Holston Medical Groups, a non-academic healthcare organization located in Tennessee, uses EHRs to speed the identification of patient candidates from its database as potential matches to a trial. EHR data also help them assess the candidate's eligibility for the trial, which results in lower “screen failures” and alerts physicians practicing with the groups of a patient's involvement in a trial, thereby decreasing protocol violations and accelerating reporting of adverse events. 47 The revenue generated from participating in clinical trials was able to cover the cost of the research department EHR system. • Researchers at the University of Michigan developed software called the Electronic Medical Record Search Engine (EMERSE) as a tool to extract research and clinical data from patient records more efficiently than manual review. They have applied this tool to screen EHRs from an administrative database for depression research studies and found significant time savings compared to manual review. 48 • Research conducted at the Cleveland Clinic compared traditional recruitment to clinical trials to an EHR-based CTA system. The study found that the CTA caused a 10-fold increase in the physicians' referral rate to clinical trials and a doubling of the enrollment rate. The physician alert is a critical process, because, while a small percentage of patients report being offered the opportunity to participate in a clinical research study, 63 percent of those asked report participating, emphasizing the importance of patient and physician awareness to a trial.49 Furthermore, most physicians feel that a CTA approach at point of care for trial recruitment is easy to use, and 77 percent of physicians appreciate being reminded about a clinical trial through a CTA.50 Strategies to Advance the Use of Electronic Health Records to Bridge Patient Care and Research Lessons Learned These examples of innovation illustrate that EHRs and digital clinical data can be incorporated into research in multiple and varied ways. These illustrations should serve to encourage those who might have been discouraged by the enormity of the challenges posed in FasterCures's 2005 report. Some of the highlights we've gleaned as we developed this report: • The traditional closed healthcare system EHR models are still growing and evolving, such as Geisinger Health System, Kaiser Permanente, and the Mayo Clinic. • Other models are emerging in which the patient is the central player. That is, he or she volunteers to provide information directly into a Web-based system for personal health and research purposes. Examples include HealthVault, The Love/Avon Army of Women, and PatientsLikeMe. • Still other efforts focus on building clinical data registries or databanks, where patient data can be stored and tracked over time, queried by investigators, and research results communicated back to participants. Examples include the Gene Partnership Project, the Research Patient Data Registry, Some institutions are using their EHR systems for clinical trial alerts, a tool used to query the EHR for matches to ongoing trials and notify the physician or other health provider of a match at the point of care with the patient. and the Shared Health Research Information Network. • Finally, some institutions are using their EHR systems for clinical trial alerts, a tool used to query the EHR for matches to ongoing trials and notify the physician or other health provider of a match at the point of care with the patient. 27 What's Next: Actions and Opportunities The potential to gather data on thousands—even millions—of patient encounters provides an unprecedented opportunity to make the connection between research and healthcare delivery. At a time of significant scientific and technological advances, we must continue to facilitate progress in the application of IT capabilities to better manage and harness clinical data. We are seeing more healthcare professionals and hospitals begin a process to adopt systems to digitize interactions with patients. As institutions move forward with adoption and implementation of health IT systems, it is critical that they consider the needs of and The potential to gather data on thousands— even millions—of patient encounters provides an unprecedented opportunity to make the connection between research and healthcare delivery. seek the advice of the research community. We need to build a solid connection between the bench and bedside. In this report, we found that the health IT infrastructure is still falling short of its potential to leverage research capabilities to increase our understanding of disease and accelerate therapies. However, we spotlight models that have integrated research capacity into the health IT framework and yielded favorable patient outcomes. These tangible examples, along with insights gleaned from leaders in healthcare, clinical research, and IT, provided us with a framework for presenting the below recommendations for action. • Clinical trial screening and matching should be included as a measure for “Meaningful Use” of electronic health record systems. • NIH should articulate a strategy that will align its programs with the recommendations of the ONC Federal Health IT Strategic Plan. • The Office of the National Coordinator should develop an initiative with pilot projects that would create medical research IT modules. • Nationwide Health Information Network (NwHIN) should expand its standards and policies to include clinical research and research centers in the network of information exchange. Each recommendation, implemented appropriately, is an opportunity to bring us closer to creating a medical research system that 28 STILL THINKING RESEARCH Strategies to Advance the Use of Electronic Health Records to Bridge Patient Care and Research will be able to meet and respond to the needs of patients, and accelerate the process of turning a scientific breakthrough into a life-saving therapy. Recommendations for Action > CLINICAL TRIAL SCREENING AND MATCHING SHOULD BE INCLUDED AS A MEASURE FOR “MEANINGFUL USE” OF ELECTRONIC HEALTH RECORD SYSTEMS. EHR systems for clinical research can improve the clinical trial process by finding patients who match specific trial criteria, thereby speeding up accrual. This will ultimately expedite the submission of trial data to the FDA in the format needed for review, while providing a system that will monitor a patient's care while on a trial. Clinical trial screening and matching is arguably the most readily adaptable functionality to expand into the “Meaningful Use” reimbursement requirements for clinical research. Currently, there are 11,000 clinical trials recruiting and enrolling three million patients.51 Integrating this recruitment function into electronic health systems will expedite patient accrual into trials, and connect the trial to patient records, ensuring that patients and their At a time of significant scientific and technological advances, we must continue to facilitate progress in the application of IT capabilities to better manage and harness clinical data. providers are kept abreast of trial information and treatment protocols in real time. This would also allow researchers and trial sponsors to shift resources previously dedicated for recruitment strategies to other critically important efforts needed for successfully completing the trial. To date, the Office of the National Coordinator for Health IT (ONC) has focused its initial EHR strategies on data capturing and sharing of a core set of variables such as vital signs, demographics, lab results, and medication lists to improve and coordinate patient care. As the ONC expands EHR functions to advanced processes, they should explore solutions to include clinical trial matching in the matrix of “meaningful use” requirements and invite input from the clinical research and patient and medical research advocacy communities on such an initiative. Without such a requirement building these capabilities will likely not be a priority for EHR developers. 29 The availability of $27 billion in HITECH funding for adoption of EHRs over the next few years provides a strong incentive to bring health IT into the clinic. By adopting clinical trial matching into the “meaningful use” framework, these incentives could also drive an increase in the number of patients and providers participating in clinical research. It is important to leverage this funding stream to ensure that clinical research can connect seamlessly with existing care systems. Clinical research and patient advocacy communities play an essential role in ensuring this requirement is brought to fruition. As the ultimate users and beneficiaries of an integrated and connected clinical trial matching system, researchers and patient advocates should actively monitor this issue diligently and create opportunities to provide input to ensure this becomes a priority. We believe the NIH can lead this two-way interaction by articulating a vision that will bring its researchers and communities into the national exchange network. > NIH SHOULD ARTICULATE A STRATEGY THAT WILL ALIGN ITS PROGRAMS WITH THE RECOMMENDATIONS OF THE ONC FEDERAL HEALTH IT STRATEGIC PLAN. In its 2011 Federal Health IT Strategic Plan, ONC specifically called for “information exchange in support of research and the translation of research findings back into clinical practice” listing the need for a two-way interaction between research and clinical care.52 As the nation's medical research agency and the largest source of funding for medical research in the world, the NIH is ideally poised to facilitate efforts that integrate research with clinical care. We believe the NIH can lead this two-way interaction by articulating a vision that will bring its researchers and communities into the national exchange network. There are numerous NIH programs that support networked research studies, yet there isn't a clearly defined strategy to bridge these programs with other federal health IT initiatives and ensure ongoing adoption of certified electronic health systems*. An NIH-driven strategy that would align research systems and certified electronic health systems could: * A certified electronic health system refers to systems that meet “meaningful use” requirements as established by the ONC. 30 STILL THINKING RESEARCH • improve workflow and reduce redundant data collection. In many clinical studies, data are required to be entered into Strategies to Advance the Use of Electronic Health Records to Bridge Patient Care and Research two different databases—one for the research team and one for the care team. This not only adds additional work for clinical and research staff, but studies evaluating dual database entry revealed error rates to be as high as 27 percent in some cases.53 Such errors in a clinical research study could have a significant impact on the research conclusions. • bridge the traditional gap between vertical integration of research and care within an institution and horizontal integration across institutions, particularly in community settings because community practitioners interact with all points along the continuum from discovery to care delivery.54 One reason for the lack of broad IT adoption and interoperability in clinical research is the absence of financial incentives.55 Individual research centers may see value in vertical alignment of their research information systems and their clinical records systems within their individual center, but the broader horizontal interoperability with other healthcare systems requires substantial resources and personnel that individual centers are unlikely to invest in and have little incentive to do so. • expand sharing of clinical data for research purposes across networks. For example, networks like the Clinical and Translational Science Award (CTSA) program at NIH would be a place to pilot initiatives that would align with certified “meaningful use” systems. As illustrated earlier in the report, a number of CTSA sites are developing novel There are numerous NIH programs that support networked research studies, yet there isn't a clearly defined strategy to bridge these programs with other federal health IT initiatives and ensure ongoing adoption of certified electronic health systems. technologies and many of them are already participating in collaborative research studies. The CTSAs could provide a test-bed for the federal strategic plan calling for the twoway interaction between research and care data systems. CTSAs, an established network of academic research centers, are also linked to community-based settings, an important consideration as majority of care delivered in the United States is in physician offices and community clinics and centers. Community practices refer patients, participate in research agendas, translate research results into practice, and communicate with and care for patients enrolled in a 31 clinical trial.56 NIH should include in its plan programs and incentives to connect the community centers and their patients with the research enterprise. The NIH strategy should incorporate the insights of patients and disease research organizations, and provide incentives to further connect the community centers and their patients with the research enterprise. Patient advocacy groups and disease research organizations are well-positioned to hold NIH accountable for ensuring its vision is carried through and actualized across existing efforts and networks. They also play a pivotal role in amplifying the impact of best practices, including those funded by the NIH, and ensure they are broadly adopted. One of the barriers standing in the way of research being integrated into an EHR system is the need for high-quality data that are annotated with patient outcomes and can be used for research purposes. > THE OFFICE OF THE NATIONAL COORDINATOR SHOULD DEVELOP AN INITIATIVE WITH PILOT PROJECTS THAT WOULD CREATE MEDICAL RESEARCH IT MODULES. One of the barriers standing in the way of research being integrated into an EHR system is the need for high-quality data that are annotated with patient outcomes and can be used for research purposes. However, as we cite in this report, a number of organizations are testing innovative models that link research and care through imaging records, biospecimens, and genomic databases with patients' EHRs. To facilitate these activities and ensure widespread use across a number of EHR platforms, ONC is well-positioned to fund pilot programs that will create research modules that can be “attached” (plug and play) or retrofitted to existing EHR systems that were built without the capacity to accommodate research. These pilot programs would allow connectivity to systems being developed to meet meaningful use requirements and encourage community practitioners to participate in clinical research. To ensure this initiative reaches full potential, the ONC should consider the need to harmonize standards for collecting genomic and molecular data and integrating these into an EHR. Genetic testing 32 STILL THINKING RESEARCH Strategies to Advance the Use of Electronic Health Records to Bridge Patient Care and Research is rapidly becoming part of routine medical care, and this will keep expanding. The earliest possible incorporation of genetic and molecular information into EHR exchange systems will accelerate the translation of research into practice. EHR systems could help to provide guidance to physicians on how best to interpret genetic test results and guide patients to new geneticallytargeted treatments. Patient and medical research advocates have an important role to play in the priority-setting and decision-making process necessary to develop meaningful research modules and harmonize standards. Often, external pressure from informed advocates can accelerate processes and ensure that efforts are designed to deliver on the ultimate goal: improving patient outcomes. They can also play a key role in developing tools to use electronic health information to improve their constituents' health. These groups should drive discussions with the ONC about mechanisms to improve patient engagement, and the ONC should provide funding opportunities to develop innovative tools for patient interaction with health IT. 9 of the top 10 Recent research has demonstrated the ability to link genetic variants in a DNA database associated with diseases like Crohn’s disease, multiple sclerosis, or atrial fibrillation to a clinical diagnosis of these diseases in a patient's EHR. 57 And for diseases like breast cancer, genetic and molecular testing is becoming standard practice in routine care, clinical decisionmaking, and clinical research. However, despite the fact that 9 of the top 10 causes of death in the United States have genetic components, there is no uniform and systematic effort to build capacity for incorporating genomic and molecular data in the EHR.58 As more individuals undergo genetic analyses and as more clinical information becomes linked to genomics, it will be critical to bridge this genetic information with clinical information collected in an EHR to improve our ability to understand the genetic underpinnings of disease. To ensure this initiative reaches full potential, the ONC should consider the need to harmonize standards for collecting genomic and molecular data and integrating these into an EHR. Genetic testing is rapidly becoming part of routine medical care, and this will keep expanding. 33 > NATIONWIDE HEALTH INFORMATION NETWORK (NwHIN) SHOULD EXPAND ITS STANDARDS AND POLICIES TO INCLUDE CLINICAL RESEARCH AND RESEARCH CENTERS IN THE NETWORK OF INFORMATION EXCHANGE. NwHIN was established to provide the infrastructure for the exchange of health information across diverse entities. Efforts are underway to standardize data, services, and policies in the delivery of healthcare using EHRs. However, the initial set of services does not include clinical research. If research systems are to effectively exchange information within and across the healthcare enterprise, there will need to be agreement on the standards and policies needed for interoperable data exchange. If research systems are to effectively exchange information within and across the healthcare enterprise, there will need to be agreement on the standards and policies needed for interoperable data exchange. Standards that could streamline data interchange between electronic source data in EHRs and systems used by clinical investigators (e.g., registries, distributed research networks, public health databases) could facilitate and improve collaboration and regulatory submission compliance. But there is much debate within the research community as to what standards are needed and how they are best implemented for research studies. NwHIN could serve as a convening entity to harmonize standards for clinical research and ensure that the research standards uniformly integrate with electronic care systems. For example, the Clinical Data Interchange Standards Consortium (CDISC) has developed vendor-neutral medical research standards to support data exchange for research studies and regulatory submission. Such standards provide NwHIN with existing models to look at to begin to bridge research into the larger network. As standards are developed, consideration must be given to research needs and research-quality data capture. Organizations that are involved in clinical research, like the NIH and academic medical centers, will need to provide input and direction to NwHIN to help define the specifications necessary for clinical research. The case studies mentioned earlier in this report illustrate the ability to proceed in some areas of clinical research without the tight and complete adherence to standards. There is an opportunity to learn from these models to build a balanced model for research standards that provides flexibility and innovation but 34 STILL THINKING RESEARCH Strategies to Advance the Use of Electronic Health Records to Bridge Patient Care and Research allows for a systemic exchange of information and data across databases and networks. Patient and medical research advocacy and disease research organizations have a critical role to play cultivating a culture of participation in research. Patients who are part of a healthcare system that uses EHRs already know the value of having a central record that can be the need for standards accessed by all healthcare providers. In addition, many consumers are learning the value of controlling and having access to their Standards experts argue that own health information through self-managed personal health common standards developed records. These patients could be effective advocates for ensuring for clinical use are necessary to such access to valuable information could also be utilized to provide the foundation for provide vital data needed for research purposes. research use.59 However, some in the research community counter that standards are secondary, are being developed at the wrong level, or need not be Ultimately, these recommendations are all designed to improve fully completed before research treatment options for patients. We urge policymakers to consider can proceed. For example, the the consequences of inaction and the real possibilities of lost idea is not to connect one opportunity to improve the way we search for treatments and cures. EHR or a biobank to another, But most importantly, we hope decisionmakers acknowledge the but rather to have them both tangible benefits of having a health IT system with integrated use a common language and research capabilities and seize opportunities to ensure we reap those feed through external interfaces benefits and translate them into better health outcomes for all. to aggregate specific pieces of information around an individual. The “don't wait for Patient groups play a unique role in bringing about change and standards” camp argues that ensuring accountability—they know the needs of their constituents too much time and money is and are trusted stewards in the interface with providers, being spent trying to foster researchers, and policymakers. They could develop educational system-to-system integration materials that help patients understand the value of clinical around every bit of information research, the importance of clinical trials, and the importance of collected, and that the medical aggregated clinical data to the research enterprise. community should instead agree on the need for a free-flow of information across systems to drive connectivity. 35 In Sum FasterCures said the following in 2005, and will continue to say it: As the healthcare system addresses the challenges of widespread adoption of electronic patient records, research capacity should be part of the architecture. The complexity of issues that affect human health—from the genomic and proteomic levels to the culture and locale of the institutions that provide healthcare services—requires that there be a more comprehensive and collaborative approach to connecting the worlds of science and the clinic. The path to a [health IT] system that also serves the needs of As the healthcare system addresses the challenges of widespread adoption of electronic patient records, research capacity should be part of the architecture. researchers is a long one, but is one that must be mapped so that no important opportunity is missed. Clinical and health services researchers have been working toward this goal for some time, with some impressive advances made in recent years. Each year, bright ideas and new tools in the form of information technology have arrived to help them. But we are far from where we need to be. As the clinical world continues to adopt health IT, the research and patient advocacy communities need to push them to think research. 36 STILL THINKING RESEARCH Strategies to Advance the Use of Electronic Health Records to Bridge Patient Care and Research Acknowledgments The authors would like the thank the following individuals who granted time for interviews, responded to email queries, and provided vital insights on the topics raised in this report. Aaron Abend Managing Director, Data Warehousing Recombinant Data Corp. Peter B. Berger, M.D. Associate Chief Research Officer; Director, Center for Clinical Studies Geisinger Health System Christopher G. Chute, M.D., Dr.P.H. Professor of Medical Informatics; Chair, Division of Biomedical Informatics Mayo Clinic College of Medicine James J. Cimino, M.D. Chief, Laboratory for Informatics Development National Institutes of Health Amy Compton-Phillips, M.D. Associate Executive Director, Quality The Permanente Federation, LLC Lou Diamond, M.D. Former Medical Director and Vice President, Healthcare Business Thomson Reuters Charles P. Friedman, Ph.D. University of Michigan Stephen H. Friend, M.D., Ph.D. President, Co-Founder, and Director Sage Bionetworks James “Jamie” Heywood Co-Founder, Chairman PatientsLikeMe Michael Kahn, M.D., Ph.D. Co-Director Colorado Clinical and Translational Sciences Institute Associate Professor, Department of Pediatrics University of Colorado, Denver William A. Knaus, M.D. Evelyn Troup Hobson Professor; Founding Chair, Department of Public Health Sciences University of Virginia School of Medicine Isaac S. Kohane, M.D., Ph.D. Director, Children's Hospital Informatics Program; Henderson Professor of Health Sciences and Technology; Harvard-MIT Division of Health Sciences and Technology; Professor of Pediatrics Harvard Medical School Shawn Murphy, M.D., PhD Associate Director, Laboratory of Computer Science—Clinical and Research Informatics Division Massachusetts General Hospital Assistant Professor, Neurology Harvard Medical School Naz Sykes Executive Director Dr. Susan Love Research Foundation James Walker, M.D., FACP Chief Health Information Officer Geisinger Health System Jon White, M.D. Director, Health Information Technology Portfolio Agency for Healthcare Research and Quality John Wilbanks Vice President, Science Creative Commons Susan Love, M.D. President and Medical Director Dr. Susan Love Research Foundation Deven McGraw Director, Health Privacy Project Center for Democracy and Technology 37 References 1 Kho, A.N. et al. 2011. Electronic medical records for genetic research: results of the emerge consortium, Science Translational Medicine, 20;3(79):79re1. 16 2 FasterCures. 2005. Think Research: Using Electronic Medical Records to Bridge Patient Care and Research, http://fastercures.org/objects/pdfs/comments/emr_whitepaper.pdf, accessed August 11, 2011. 17 U.S. Department of Health and Human Services, National Institutes of Health, National Cancer Institute. April 2010. The HMO Cancer Research Network: Capacity, Collaboration, and Investigation. 3 18 Campbell, M.K. et al. 2007. Recruitment to randomised trials: Strategies for trial enrollment and participation study, The STEPS Study, Health Technology Assessment. 11(48):iii, ix-105. 4 Cheng, S. et al. 2010. A sense of urgency: Evaluating the link between clinical trial development time and the accrual performance of Cancer Therapy Evaluation Program (NCI-CTEP) sponsored studies, Clinical Cancer Research, 16(22):5557-5562. 5 Schilsky, R. 2011. Accrual to cancer clinical trials in the era of molecular medicine, Science Translational Medicine, 3(75):75cm9. DOI: 10.1126/scitranslmed.3001712. 6 Nadler, J.J., and Downing, G.J. 2010. Liberating health data for clinical research applications, Science Translational Medicine. 2(18):1-4. HMORN Virtual Data Warehouse, http://www.hmoresearchnetwork.org/resources/toolkit/HMORN_VDW.doc, accessed August 11, 2011. Brown, J., Holmes, J., Maro, J. et al. July 2009. Design specifications for network prototype and cooperative to conduct population-based studies and safety surveillance. Effective Health Care Research Report No. 13. Rockville, Md.: Agency for Healthcare Research and Quality. 19 McCarty C.A., et al. 2011. The eMERGE Network: A Consortium of Biorepositories Linked to Electronic Medical Records Data for Conducting Genomic Studies, BMC Medical Genomics 4(13). doi:10.1186/1755-8794-4-13. 20 NIH News. eMERGE network moves closer to tailored treatments based on patients' genomic information NIH-supported project expands into clinic. August 17, 2011. http://www.nih.gov/news/health/aug2011/nhgri-17.htm 21 7 Office of the National Coordinator for Health Information Technology (ONC). Federal Health Information Technology Strategic Plan 2011-2015. Nass, S. et al. 2009. Beyond the HIPAA Privacy Rule: Enhancing Privacy Improving Health Through Research. Institute of Medicine. Committee on Health Research and the Privacy of Health Information: The HIPAA Privacy Rule. Washington, D.C.: National Academies Press. 8 Blumenthal, D. 2010. Launching HITECH, New England Journal of Medicine. 362 (5):382-385. 9 22 Informatics for Integrating Biology and the Bedside, https://www.i2b2.org/index.html, accessed August 11, 2011. ONC, op cit. 23 10 11 ONC, ibid. http://www.cdc.gov/phin/2011/spotlight/PHITPO_statement.html. 12 DesRoches, C.M. et al. 2008. Electronic health records in ambulatory care—A national survey of physicians, New England Journal of Medicine, 359:50-60. 13 Jha et al. 2009. Use of electronic health records in U.S. hospitals, New England Journal of Medicine, 360:1628-38. 14 Department of Health and Human Services Press Office. January 13, 2011. Surveys show significant proportions of hospitals and doctors already plan to adopt electronic health records and qualify for federal incentive payments, http://www.hhs. gov/news/press/2011pres/01/20110113a.html, accessed August 11, 2011. Murphy, S.N., et al. 2010. Servicing the enterprise and beyond with informatics for Integrating Biology and the Bedside (i2b2), Journal of the American Medical Informatics Association, 17:124-30. 24 Himes, B.E. et al. 2009. Prediction of chronic obstructive pulmonary disease (COPD) in asthma patients using electronic medical records, Journal of the American Medical Informatics Association, 16(3):371-379. 25 Deshmukh, V. et al. 2009. Evaluating the informatics for integrating biology and the bedside system for clinical research, BMC Medical Research Methodology. doi: 10.1186/1471-2288-9-70. 26 Fridsma, D.B. et al. 2008. The BRIDG Project: A Technical Report, Journal of the American Medical Informatics Association, 2008;15:130-137. doi:10.1197/jamia.M2556. 27 15 Shah, N.R., et al. 2010. Clinical effectiveness: Leadership in comparative effectiveness and translational research, Clinical Medicine and Research. 8(1):28-29. 38 STILL THINKING RESEARCH U.S. Department of Health and Human Services. July, 2010. The Sentinel Initiative: Access to Electronic Healthcare Data for More than 25 Million Lives. Achieving FDA Section 905 Goal One. Strategies to Advance the Use of Electronic Health Records to Bridge Patient Care and Research 28 Reis, S.E., et al. 2010. Reengineering the National Clinical and Translational Research Enterprise: The Strategic Plan of the National Clinical and Translational Science Awards Consortium, Academic Medicine, 85(3):463-469. doi: 10.1097/ACM.0b013e3181ccc877. 39 PACeR: Partnership to Advance Clinical electronic Research. Transforming and Improving Clinical Research Capabilities in New York State to Benefit Patients. Phase 1 White Paper, Feasibility Assessment, and Phase 2 Plan, http://pacerhealth.org/ media/pdf/2011-05-12_pacer_whitepaper.pdf, accessed August 11, 2011. 29 Electronic Health Records Overview. 2006. Produced by the MITRE Corporation through support from the National Center for Research Resources, http://www.ncrr.nih.gov/informatics_ support/clinical_research_informatics_reports/ehr.pdf, accessed August 11, 2011. 40 Liao, K.P. et al. 2010. Electronic medical records for discovery research in rheumatoid arthritis, Arthritis Care & Research, 62: 1120-1127. doi: 10.1002/acr.20184. 41 Hastings, S. et al. 2009. Adoption and Adaption of caGRID for CTSA. Summit on Translational Bioinformatics. March 1, 2009. 44-8 Nass, S.J., Moses, H.L., Mendelson, H., Editors. 2010. A National Cancer Clinical Trials System for the 21st Century: Reinvigorating the NCI Cooperative Group Program. Washington, D.C. National Academies Press. 31 42 30 Steele, S. 2010. Working with the CTSA Consortium: What we bring to the table, Science Translational Medicine. 2(63):63mr5. 32 Selker, H.P. et al. 2010. White paper on CTSA consortium role in facilitating comparative effectiveness research: September 23, 2009 CTSA Consortium Strategic Goal Committee on Comparative Effectiveness Research, Clinical Translational Science, 3(1):29-37. 33 Harris, P.A. et al. 2009. Research Electronic Data Capture (REDCap)—A Metadata-driven methodology and workflow process for providing translational research informatics support, Journal of Biomedical Informatics. 42(2): 377-381. National Cancer Institute at the National Institutes of Health. Cancer Clinical Trials: The Basics Workbook, http://www.cancer .gov/clinicaltrials/education/basicworkbook/, accessed August 11, 2011. 43 Nass et al., op cit. 44 Data published at NIH Web site Feb 14, 2011. Estimates of Funding for Various Research, Condition, and Disease Categories (RCDC), http://report.nih.gov/rcdc/categories/ 45 Nass, et al., op cit. 46 Research Electronic Data Capture, http://project-redcap.org, accessed June 3, 2011. Embi, P.J. et al. 2005. Effect of a clinical trial alert system on physician participation in trial recruitment, Archives of Internal Medicine. 165: 2272-2277. 35 47 34 Reis, S.E. et al. 2008. Crossing the Research Valleys of Death: The University of Pittsburgh Approach, Clinical Translational Science, 1 (1):9-10. 36 Public opinion poll conducted by Charlton Research Company for Research!America. June 2009. http://www.researchamerica. org/uploads/YourCongress2009.pdf, accessed August 11, 2011. 37 Miller, J.L. et al. 2005. The EHR solution to clinical trial recruitment in physician groups. Holston Medical Group, http://www.healthmgttech.com/index.php/solutions/electronicmedical-records/the-ehr-solution-to-clinical-trial-recruitment-inphysician-groups.html, accessed August 11, 2011. 48 Seyfried, L. et al. 2009. Enhanced identification of eligibility for depression research using an electronic medical record search engine, International Journal of Medical Informatics. 78(12):E13-e18. How the Public Views Privacy and Health Research. Results of a National Survey commissioned by the Institute of Medicine Committee on “Health Research and the Privacy of Health Information: The HIPAA Privacy Rule,” survey conducted by Harris Interactive and Dr. Alan F. Westin, http://www.ftc.gov/os/ comments/healthcarewrkshp/534908-00001.pdf, accessed August 11, 2011. Harris Interactive Poll. The Many Reasons Why People Do (and Would) Participate in Clinical Trials, http://www.harrisinteractive.com/news/newsletters/healthnews/HI_HealthCareNews2003 Vol3_Iss10.pdf, accessed August 11, 2011. 38 50 Markle Foundation survey conducted by Lake Research Partners and American Viewpoint. November 2006. Survey Finds Americans Want Electronic Personal Health Information to Improve Own Health Care, http://www.markle.org/ sites/default/files/research_doc_120706.pdf, accessed August 11, 2011. 49 Embi, P.J. et al. 2008. Physicians' perceptions of an electronic health record-based clinical trial alert approach to subject recruitment: A survey, BMC Medical Informatics and Decision Making, 8:13. 39 51 English R., Lebovitz, Y. Giffin, R. 2010. Transforming clinical research in the United States: challenges and opportunities. Washington, D.C.: National Academies Press. 52 U.S. Department of Health and Human Services. Office of the National Coordinator for Health Information Technology, Federal Health Information Technology Strategic Plan 2011-2015. 53 Goldberg S.I. et al. 2008. Analysis of data errors in clinical research databases. AMIA Annual Symposium Proceedings 242-6. 54 Dzau, op cit. 55 Sung, N. et al. 2003. Central challenges facing the national clinical research enterprise, Journal of the American Medical Association 289(10):1278-1287. 56 Aguilar-Gaxiola et al. 2008. Researchers and Their Communities: The Challenge of Meaningful Community Engagement. Summary paper developed by the CTSA Community Engagement Key Function Committee. http://www.ctsaweb.org/uploadedfiles/Best%20Practices%20in %20Community%20Engagement_Summary_2007-08.pdf 57 Ritchie M.D., et al. 2010. Robust replication of genotype-phenotype associations across multiple diseases in an electronic medical record, American Journal of Human Genetics 86:560572. 58 http://www.cdc.gov/genomics/public/faq.htm. 59 Richesson, R. and Krischer, J. 2007. Data Standards in Clinical Research: Gaps, Overlaps, Challenges, and Future Directions, Journal of the American Medical Informatics Association. 14(6) 687-96. 40 STILL THINKING RESEARCH Strategies to Advance the Use of Electronic Health Records to Bridge Patient Care and Research Join Us Accelerate Medical Progress > Help us facilitate outcomes-oriented collaboration. > Take part in programs designed to engage patients in research. > Get involved in efforts that will maximize smart R&D investments. > Support our efforts to ensure policies and processes promote progress. > Invest in our mission with a gift to FasterCures. Get Involved! FasterCures The Center for Accelerating Medical Solutions Learn More: www.fastercures.org Be in the Know: FasterCures SmartBrief Read and Comment: The FasterCures Blog Stay Connected: @fastercures FasterCures 1101 New York Avenue, NW, Suite 620, Washington, DC 20005 / 202-336-8900 / www.FasterCures.org FasterCures, a center of the Milken Institute, is nonprofit, nonpartisan, and independent of interest groups.