PDF hosted at the Radboud Repository of the Radboud University
advertisement
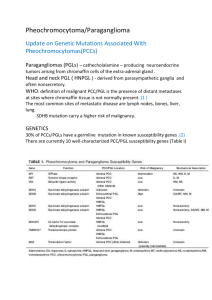
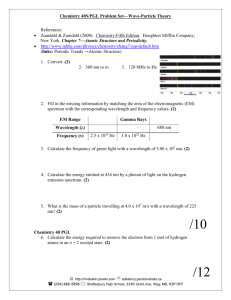
PDF hosted at the Radboud Repository of the Radboud University Nijmegen The following full text is a publisher's version. For additional information about this publication click this link. http://hdl.handle.net/2066/52566 Please be advised that this information was generated on 2016-03-04 and may be subject to change. 0021-972X/07/$15.00/0 Printed in U.S.A. The Journal of Clinical Endocrinology & Metabolism 92(3):779 –786 Copyright © 2007 by The Endocrine Society doi: 10.1210/jc.2006-2315 EXTENSIVE CLINICAL EXPERIENCE Clinical Presentations, Biochemical Phenotypes, and Genotype-Phenotype Correlations in Patients with Succinate Dehydrogenase Subunit B-Associated Pheochromocytomas and Paragangliomas Henri J. L. M. Timmers, Anna Kozupa, Graeme Eisenhofer, Margarita Raygada, Karen T. Adams, Daniel Solis, Jacques W. M. Lenders, and Karel Pacak Reproductive Biology and Medicine Branch (H.J.L.M.T., A.K., K.T.A., D.S., K.P.), National Institute of Child Health and Human Development, Clinical Neurocardiology Section (G.E.), National Institute of Neurological Disorders and Stroke, and Laboratory of Clinical Genetics (M.R.), National Institutes of Health, Bethesda, Maryland 20892-1109; and Department of Internal Medicine (J.W.M.L.), Division of General Internal Medicine, and Department of Endocrinology (H.J.L.M.T.), Radboud University Nijmegen Medical Centre, 6500 HB Nijmegen, The Netherlands Context: Mutations of the gene encoding succinate dehydrogenase subunit B (SDHB) predispose to malignant paraganglioma (PGL). Recognition of the SDHB phenotype in apparently sporadic PGL directs appropriate treatment and family screening. and was the sole symptom in 14%. Seventy-six percent had hypertension, and 90% lacked a family history of PGL. All primary tumors but one originated from extraadrenal locations. Mean ⫾ SD tumor size was 7.8 ⫾ 3.7 cm. In this referral-based study, 28% presented with metastatic disease and all but one eventually developed metastases after 2.7 ⫾ 4.1 yr. Ten percent had additional head and neck PGLs. The biochemical phenotype was consistent with hypersecretion of both norepinephrine and dopamine in 46%, norepinephrine only in 41%, and dopamine only in 3%. Ten percent had normal catecholamine (metabolite) levels, consistent with biochemically silent PGL. No obvious genotype-phenotype correlations were identified. Objective: The objective of the study was to assess mutation-specific clinical and biochemical characteristics of SDHB-related PGL. Design: The study design was retrospective descriptive. Patients: Patients included 29 patients (16 males) with SDHB-related abdominal or thoracic PGL. Conclusions: SDHB-related PGL often presents as apparently sporadic PGL with symptoms related to tumor mass effect rather than to catecholamine excess. The predominant biochemical phenotype consists of hypersecretion of norepinephrine and/or dopamine, whereas 10% of tumors are biochemically silent. The clinical expression of these tumors cannot be predicted by the genotype. (J Clin Endocrinol Metab 92: 779 –786, 2007) Intervention: There was no intervention. Main Outcome Measures: Clinical presentations, plasma and urine concentrations of catecholamines and O-methylated metabolites, and genotype-phenotype correlations were measured. Results: Mean ⫾ SD age at diagnosis was 33.7 ⫾ 15.7 yr. Tumorrelated pain was among the presenting symptoms in 54% of patients P ARAGANGLIOMAS (PGLS) are tumors that derive from either sympathetic tissue in adrenal and extraadrenal locations or parasympathetic tissue of the head and neck (1). The majority of sympathetic tissue-derived PGLs produce catecholamines, whereas parasympathetic PGLs usually do not. A PGL arising from catecholamine-producing cells of the adrenal medulla is also referred to as pheochromocytoma (PHEO) (2, 3). The three genes involved in the pathogenesis of familial PGL syndrome described to date (4 – 6) include those encoding the B, C, and D subunits of mitochondrial complex II enzyme succinate dehydrogenase (SDH). Mutations of these genes result in distinct clinical syndromes. SDHC mutation carriers typically present with benign solitary head and neck PGL (7), whereas SDHD mutations are most frequently associated with multifocal head and neck PGL and less frequently with adrenal and extraadrenal PGL (8, 9). The typical PGL associated with SDHB mutations originates from extraadrenal abdominal or thoracic locations (8 –11). In contrast to predominantly benign SDHC and D-associated tumors, up to 70% of SDHB-related abdominal and thoracic PGLs develop into metastatic disease (12). Recognizing SDHB-related disease in individual patients can be delayed due to several factors. Despite an autosomal dominant pattern of inheritance, penetrance of the disease is incomplete and age dependent (8). Many patients with SDHB-related tumors have no family history of PGL. Of First Published Online January 2, 2007 Abbreviations: CT, Computed tomography; MRI, magnetic resonance imaging; PGL, paraganglioma; PHEO, pheochromocytoma; SDH, succinate dehydrogenase. JCEM is published monthly by The Endocrine Society (http://www. endo-society.org), the foremost professional society serving the endocrine community. 779 780 J Clin Endocrinol Metab, March 2007, 92(3):779 –786 Timmers et al. • SDHB-Related Paraganglioma patients with apparently sporadic PHEO or abdominal/thoracic PGL, 4 –7% have been identified as carriers of pathogenic SDHB mutations (12, 13). Furthermore, the diagnosis may be delayed by lack of symptoms related to catecholamine excess. Such clinically silent PGLs either do not produce catecholamines or produce and metabolize but do not secrete catecholamines or produce dopamine but not other catecholamines (14 –17). The aim of this study was to gain detailed insight into the clinical and biochemical characteristics of SDHB-associated tumors. In this single-center, referral-based study of patients with SDHB-associated PHEO or abdominal/thoracic PGL, clinical presentation, biochemical phenotype, tumor localization and pathology, and additional diagnoses were evaluated for evidence of genotype-phenotype correlations. Timely recognition of the SDHB phenotype in apparently nonfamilial cases direct an appropriate strategy for treatment, follow-up, and family screening. Patients and Methods Patients This study included 29 patients (16 males, 13 females) with histological proof PHEO or of extraadrenal abdominal (including intrapelvic) or thoracic PGL. There was no evidence of any family relationships among patients. Eighteen patients were also included in a previous study by our group (18). The patients represent all consecutive carriers of an allelic variant of the SDHB gene among a large group of patients who underwent genetic testing as part of evaluation of benign or malignant PGL at the National Institutes of Health (NIH). Genetic testing for mutations in the SDHB gene was performed at the Department of Human Genetics of the Pittsburgh University Medical Center as described elsewhere (19). Patients were included between November 2000 and May 2006. The protocol for this study was approved by the Institutional Review Board of the National Institutes of Child Health and Human Development at the NIH. All patients provided written informed consent. The reason for referral to the NIH was to outline an optimal treatment plan for (suspected) metastatic PGL. The mean ⫾ sd interval between the initial diagnosis and referral to NIH was 5.0 ⫾ 8.5 yr. Clinical evaluation included a standardized inventory of symptoms and signs. Information on individual patients is summarized in Table 1. Laboratory tests and imaging Blood samples were collected into heparin-containing tubes by use of a forearm venous cannula, with patients supine for at least 20 min before sampling. Patients were instructed to fast and abstain from caffeinated and decaffeinated beverages overnight and avoid taking acetaminophen for 5 d before blood sampling. All samples were collected on ice, and plasma was separated and stored at ⫺80 C before analysis according to recommended procedures (20). Plasma was assayed by HPLC for concentrations of free metanephrines and catecholamines, as described previously (21, 22), with further details and modifications as listed on the Clinical Neurochemistry Laboratory web site (http://www.catecholamine.org/labprocedures). The 24-h urinary outputs of catecholamines and deconjugated (free plus conjugated) fractionated metanephrines for patients seen at the NIH were measured by HPLC or liquid chromatography with tandem mass spectroscopy, under a contract between the NIH Clinical Center and an outside commercial laboratory (Mayo Medical Laboratories, Rochester, MN). HPLC procedures were also used for urinary measurements in patients seen elsewhere, as described previously. Biochemical profiles were determined during the initial evaluation at the NIH. Hypersecretion of catecholamines was defined as elevation of plasma and/or urine levels of the catecholamines TABLE 1. Characteristics of individual patients No. Sex, age at SDHB sequence diagnosis variant protein (yr) cDNA Ref. Primary tumor location, size (cm) Metastases, years since diagnosis Metastases, location Family history of PGL 0.0 8.4 0.9 a/p, li, b a/p, lu, li, b, n lu, li, b Neg Neg Neg a/p, li, b a/p, lu b a/p, b a/p, lu, li, n a/p, lu, b, n a/p, b a/p, li a/p, lu, b, me a/p, lu, b, me a/p, li, b 1 2 3 F, 38 M, 10 F, 51 p.Pro130HisfsX5 IVS1–9A⬎G IVS3⫹1G⬎A c.391_392delC c.73–9A⬎G c.286⫹1G⬎A 28 18 18 l (juxta-)adrenal, ⬎5 r paraadrenal, 10 r paraaortic abd, 7.5 4 5 6 7 8 9 10 11 12 13 14 15 16 17 18 M, 35 F, 34 M, 52 F, 23 F, 49 M, 28 M, 8 F, 37 M, 10 M, 39 F, 39 F, 25 M, 35 M, 29 M, 60 IVS3–1G⬎C p.Arg115X p.Cys196Tyr p.Val124SerfsX39 p.Ile127Ser p.Cys196Tyr p.Val140Phe p.Val140Phe p.Arg46X p.Gln214His IVS3⫹2T⬎A p.Cys192Arg IVS1⫹1G⬎T p.Gly96Asp p.Trp200Cys c.287–1G⬎C c.343C⬎T c.587G⬎A c.369_370insA c.380T⬎G c.587G⬎A c.418G⬎T c.418G⬎T c.136C⬎T c.642G⬎C c.286⫹2T⬎A c.574T⬎C c.72⫹1G⬎T c.287G⬎A c.600G⬎T New 8, 23 8, 9 New 18 8, 9, 12 18 18 8, 23, 25 18 18 9, 12 8, 26 18 New l pararenal, 14.5 bladder, 5 l paraaortic abd, 6.0 Paraaortic abd, 3.0 r paraadrenal, 5.5 Bladder/chest wall l parailiac art, ⬎5.0 Pelvic, 13.5 l paraadrenal, 5.0 l paraadrenal, 9.0 l extraadrenal abd, 7.0 r paraaortic abd, 4.0 Aortic bifurcation, 7.7 l pararenal, 18.0 Aortic bifurcation, 6.0 0.5 2.5 0.2 0.3 4.3 0.0 0.0 0.8 17.1 4.1 4.5 0.0 1.7 0.2 a/p, b, me b a/p, lu, b Pos Neg Neg Neg Neg Neg Neg Neg Neg Neg Neg Neg Neg Neg Neg 19 20 21 M, 23 F, 24 M, 47 p.Arg46X c.136C⬎T 8, 23 p.Ile127Ser c.380T⬎G 18 p.Glu228GlyfsX27 c.683_684delAG 18 Aortic bifurcation, 7.5 l juxtaadrenal, 5.5 l para-(ad)renal, 10.0 0.0 0.0 3.5 b b a/p, b, me Neg Neg Pos 22 23 24 F, 72 F, 35 F, 45 IVS1⫹1G⬎T p.Arg46X p.Val140Phe Aortic bifurcation, 10.0 Bladder, 3.5 r paraaortic abd, 5.5 0.2 1.5 0.0 a/p, b a/p, me a/p Neg Neg Neg c.72⫹1G⬎T c.136C⬎T c.418G⬎T 8, 26 8, 23 18 25 F, 51 IVS5–2A⬎G c.541–2A⬎G 18 r adrenal, 5.5 3.4 a/p, me, n Pos 26 M, 11 p.Val140Phe c.418G⬎T 18 Paraaortic abd, 8.0 1.1 a/p, lu, b Neg 27 28 29 M, 39 M, 7 M, 35 p.Arg46Gln p.Arg230His p.Val140Phe c.137G⬎A c.689G⬎A c.418G⬎T 27 10 18 l extraadrenal abd, 15.0 l pararenal, 4.0 l pararenal, 8.0 0.0 7.1 13.3 a/p, me, b a/p, lu, b b Neg Neg Neg Additional diagnosis Hypercholesterolemia, obesity, depression Sinusitis, appendicitis Hypothyroidism Dyspepsia Uterus myoma, cholelithiasis Miscarriage Varicocele Cholelithiasis, deep venous trombosis Hiatus hernia Hernia nuclei pulposi, depression Uterus myoma, hypothyroidism Uterus/bladder prolaps, cholelithiasis Benign breast tumor, colon polyps, melanoma, goiter Myocardial hypertrophy, hernia nuclei pulposi Asthma, acid reflux, nodule l upper thyroid Pos, Positive; Neg, negative; M, male; F, female; l, left; r, right; art, artery; abd, abdomen; a/p, abdominal/pelvic; lu, lung; li, liver; me, mediastinum; n, neck. Timmers et al. • SDHB-Related Paraganglioma J Clin Endocrinol Metab, March 2007, 92(3):779 –786 781 tases of a large, 16 cm extra-adrenal PGL located in the left retroperitoneum. These 3 patients lacked symptoms of catecholamine excess, which is consistent with the findings of normal levels of plasma and urine catecholamines and catecholamine metabolites. Also, during progression of metastatic lesions during follow-up, their plasma and urine levels of catecholamines and their metabolites remained normal. The fourth patient (no. 21) who had pain as an isolated initial symptom presented with abdominal pain and nausea due to an invasive 10 cm retroperitoneal tumor. Laboratory findings in this particular patient indicated isolated hypersecretion of dopamine and not of other catecholamines. Later on he developed metastatic lesions to the bone and mediastinum. At this point he did experience occasional palpitations, diaphoresis and bouts of hypertension in addition to therapyresistant bone pain. Another patient (no. 11) was completely free of symptoms and signs, when a 9-cm intrapelvic tumor was incidentally discovered on ultrasound during pregnancy. Her laboratory findings were consistent with both norepinephrine and dopamine production. In 3 of 29 (10%) patients, family history was positive for PGL. The father of one patient (no. 4) was a carrier of the same SDHB mutation as was his son (IVS3–1G⬎C), and had a neck PGL removed at age 30. The father of another patient (no. 21) had multiple head and neck PGL and was being treated for malignant abdominal PGL with multiple bone lesions elsewhere. The mother of another patient (no. 25) had a mediastinal PGL removed in her fifties and was doing well. Information on the genotype of the latter two relatives is lacking. A sister of another (no. 23), who was also carrier of the p.Arg46X mutation, had no history of PGL, but was treated for papillary thyroid cancer. and/or the O-methylated metabolites metanephrine and normetanephrine above the upper range of normal. Anatomic localization of PGL was performed by whole-body CT and/or whole-body MRI, which included the head and neck area in search of (additional) parasympathetic PGL. Results Initial clinical presentation Age at presentation of first symptoms was 30.6 ⫾ 16.0 (range 6 –70) yr. The initial clinical presentation included one or more symptoms relating to catecholamine excess in 23 of 28 (82%) of patients (Table 2). Nine of 28 (32%) patients had a classic triad of headache, palpitations and diaphoresis. These symptoms occurred episodically in 14 of 16 (88%) patients, were related to exercise in three patients (no. 5, 20, and 26) and to micturition in two patients (no. 10, 24). The latter two had intrapelvic tumors. Three patients presented with hypertensive crisis, either during pregnancy (no. 5) or during anesthesia for stomach surgery (no. 19), one coinciding with stroke (no. 28). Twenty-two of 29 (76%) patients had a history of hypertension, including one (no. 1) who became blind due to hypertensive retinopathy. Tumor-related pain was among the initial presenting symptoms in 15 of 28 (54%) patients, and was the sole presenting symptom in 4 patients (no. 17, 18, 21, 27). One of these patients (no. 17) presented with upper abdominal discomfort caused by a large 18 cm retroperitoneal mass. Another (no. 18) had experienced pelvic pain, hematuria and weight loss before presenting with deep venous thrombosis of the left leg due to intrapelvic metastases. Another (no. 27) presented with back pain related to multiple metastatic lesions of the lumbar spine that were pathologically proven to be metasTABLE 2. Signs and symptoms at presentation Anxiety/ panic attacks Hypertension Dizziness Nausea Chest pain Tumorrelated pain ⫹ ⫺ ⫹ ⫺ ⫺ ⫺ ⫹ ⫹ ⫹ ⫹ ⫹ ⫹ ⫹ ⫹ ⫺ ⫺ ⫺ ⫹ ⫺ ⫹ ⫹ ⫹ ⫺ ⫹ ⫹ ⫺ ⫺ ⫺ ⫺ ⫹ ⫹ ⫹ ⫹ ⫹ ⫹ ⫺ ⫺ ⫺ ⫺ ⫹ ⫹ ⫺ ⫹ ⫺ ⫺ ⫹ ⫺ ⫺ ⫺ ⫹ ⫺ ⫺ ⫹ ⫺ ⫺ ⫹ ⫹ ⫺ ⫹ ⫺ ⫹ ⫺ ⫺ ⫹ ⫺ ⫺ ⫺ ⫺ ⫺ ⫺ ⫹ ⫹ ⫹ ⫹ ⫹ Headache Tachycardia/ palpitations Diaphoresis Flushing 1 2 3 4 5 ⫹ ⫹ ⫺ ⫺ ⫹ ⫹ ⫺ ⫹ ⫹ ⫹ ⫹ ⫹ ⫹ ⫺ ⫹ ⫺ ⫺ 6 7 8 9 10 11 ⫺ ⫹ ⫹ ⫹ ⫹ ⫺ ⫹ ⫹ ⫹ ⫹ ⫹ ⫹ ⫺ ⫹ ⫺ ⫺ ⫹ ⫺ ⫺ ⫺ ⫹ ⫺ ⫺ ⫺ ⫺ ⫺ ⫺ 12 13 14 15 16 ⫹ ⫹ ⫹ ⫹ ⫹ ⫺ ⫹ ⫺ ⫺ ⫺ ⫺ ⫺ ⫹ ⫺ ⫹ ⫺ ⫹ ⫹ 17 18 ⫺ ⫺ ⫺ ⫺ ⫺ ⫺ ⫺ ⫺ ⫺ ⫺ ⫺ ⫺ ⫺ 19 20 21 22 ⫹ ⫺ ⫺ ⫺ ⫹ ⫺ ⫺ ⫹ ⫺ ⫺ ⫺ ⫺ ⫺ ⫹ ⫺ ⫺ ⫹ ⫹ ⫹ ⫹ ⫺ ⫹ ⫹ ⫹ ⫹ ⫺ ⫹ ⫹ 62 ⫹ ⫹ ⫹ ⫹ ⫺ ⫹ ⫹ 68 ⫺ ⫹ ⫹ ⫹ ⫺ ⫹ ⫹ 56 Patient no. 23 24 25 26 27 28 29 Percent of total ⫹ ⫹ ⫹ Pallor Tremor ⫹ ⫹ ⫹ ⫹ ⫺ ⫺ ⫹ 44 ⫹ ⫺ ⫹ ⫺ ⫹ ⫺ 20 ⫺ ⫺ ⫺ ⫹ ⫹ 29 ⫹ ⫹ ⫺ ⫹ ⫺ 62 ⫹ ⫹ ⫹ ⫺ ⫹ ⫹ ⫹ ⫹ ⫺ ⫹ ⫺ 75 ⫺ ⫹ ⫺ ⫺ ⫺ 32 ⫹ ⫺ ⫹ ⫺ ⫹ ⫹ 57 ⫺ ⫹ ⫺ ⫹ ⫺ ⫺ ⫹ 53 ⫹ ⫹ ⫹ ⫹ ⫹ ⫺ ⫹ ⫺ ⫺ ⫹ ⫹ ⫹ ⫹ 54 Additional comments Severe hypertensive retinopathy, fatigue Recent diabetes mellitus, weight loss Exercise-related symptoms, hypertensive crisis during pregnancy Weight loss Constipation, dyspnea Fatigue Tachycardia upon voiding, fatigue, weight loss No symptoms (incidentaloma on ultrasound for pregnancy) Fatigue Presenting symptoms unknown, patient diseased Fatigue, orthostatic tachycardia, dizziness Erectile dysfunction, deep venous thrombosis, weight loss Fatigue, dyspnea Deep venous trombosis, hematuria, fatigue, weight loss Fatigue, weakness Exercise-related nausea/vomiting, abdominal pain Fatigue, weight loss, blurred vision, constipation, weakness Sympoms related to voiding Dizziness Dyspnea Exercise-related symptoms, fatigue, weakness Hypertensive crisis including stroke Numbness in hands, fatigue 782 J Clin Endocrinol Metab, March 2007, 92(3):779 –786 Timmers et al. • SDHB-Related Paraganglioma Diagnosis and follow-up Mean ⫾ sd age at diagnosis of PHEO or PGL was 33.7 ⫾ 15.7 yr. The delay until the diagnosis was 4.5 ⫾ 4.6 (range 1–19) years. Primary tumors, detected by either computed tomography (CT) or magnetic resonance imaging (MRI), were in extraadrenal locations in all but one patient (no. 25). The maximal diameter of the primary tumors from either pathology or radiology reports was 7.8 ⫾ 3.7 cm. In eight of 29 (28%) patients, metastatic disease was already apparent at initial presentation. Malignant PHEO and PGL was defined as the presence of metastatic lesions at sites in which chromaffin tissue is normally absent (23). Pathology reports of all resected (n ⫽ 21) and biopsied (n ⫽ 8) primary tumors were consistent with PHEO or PGL. In 14 of 29 (48%) patients, tumor invasion of blood/lymphatic vessels or adjacent organs was mentioned in the pathology report. Head and neck PGLs had been diagnosed before referral in three of 2930 (10%) patients (no. 12, 21: left glomus caroticum, and no. 24: left glomus jugulare). No additional head and neck tumors were identified during evaluation at the NIH. Additional diagnoses from medical history are indicated in Table 1. In this referral-based study, all patients except one developed metastatic lesions. One patient (no. 15) had no radiological or biochemical evidence of malignant PGL. Mean interval between diagnosis of PGL and metastatic disease was 2.7 ⫾ 4.1 (range 0 –17) yr. Metastatic locations included the abdominal/intrapelvic compartment (outside the liver) in 89% of patients, bone in 75%, lung in 36%, liver in 25%, mediastinum in 29%, and head or neck in 14% (Table 1). Metastatic lesions were detected by CT and/or MRI in 27 of 28 (96%) patients. In one patient (no. 20), CT and MRI were negative, whereas [123I]-metaiodobenzylguanidine scintigraphy showed multiple bone lesions as well as pathological activity in the right abdominal paraaortic region. Four patients died of widespread metastatic disease (no. 8, 13, 22, and 25). Biochemical phenotype Data available from outside centers on laboratory findings at diagnosis of primary nonmetastatic PHEO were limited. At diagnosis of the primary tumor, plasma concentrations of norepinephrine were elevated in five of five patients, free normetanephrine in five of six, and plasma dopamine in three of six, whereas none had elevated plasma concentrations of epinephrine or free metanephrine. At this point, 24-h urinary output of norepinephrine was elevated in six of seven patients, deconjugated normetanephrine in four of six, vanillylmandelic acid in nine of 10, dopamine in one of one, and epinephrine and metanephrine in none. At evaluation of metastatic disease at the NIH, the profile of catecholamine hypersecretion was distributed as follows: both norepinephrine and dopamine in 13, norepinephrine only in 12, dopamine only in one, and no hypersecretion of catecholamines in the three (Table 3). Two patients (no. 9, 22) with wide- TABLE 3. Biochemical phenotype Plasma Urine Patient no. NE E DA NMN MN CgA 1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 18 19 20 21 22 23 24 25 26 27 28 29 Percent of total ⫹ ⫹ ⫹ ⫹ ⫹ ⫹ ⫹ ⫹ ⫹ ⫹ ⫹ ⫹ ⫹ ⫹ ⫹ ⫹ ⫺ ⫺ ⫹ ⫹ ⫺ ⫹ ⫹ ⫹ ⫹ ⫹ ⫺ ⫹ ⫹ 86 ⫺ ⫺ ⫺ ⫺ ⫺ ⫺ ⫺ ⫺ ⫺ ⫺ ⫺ ⫺ ⫺ ⫺ ⫺ ⫺ ⫺ ⫺ ⫺ ⫺ ⫺ ⫹ ⫺ ⫺ ⫺ ⫺ ⫺ ⫺ ⫺ 3 ⫹ ⫹ ⫺ ⫹ ⫺ ⫺ ⫺ ⫹ ⫹ ⫹ ⫹ ⫹ ⫹ ⫺ ⫺ ⫹ ⫺ ⫺ ⫹ ⫺ ⫹ ⫹ ⫹ ⫺ ⫺ ⫺ ⫺ ⫺ ⫺ 48 ⫹ ⫹ ⫹ ⫹ ⫹ ⫹ ⫹ ⫹ ⫹ ⫹ ⫺ ⫹ ⫹ ⫹ ⫺ ⫺ ⫺ ⫺ ⫺ ⫺ ⫺ ⫹ ⫹ ⫹ ⫹ ⫹ ⫺ ⫺ ⫹ ⫹ ⫺ ⫹ ⫹ ⫹ ⫹ ⫹ ⫺ ⫹ ⫹ 82 ⫺ ⫺ ⫺ ⫺ ⫺ ⫺ ⫹ ⫺ ⫺ ⫺ ⫺ ⫺ ⫺ ⫺ 7 ⫹ ⫺ ⫺ ⫺ ⫺ ⫺ ⫹ ⫹ ⫺ ⫹ ⫺ ⫹ ⫺ ⫹ ⫹ ⫹ ⫹ ⫹ 81 NE E DA NMN MN ⫹ ⫺ ⫹ ⫺ ⫺ ⫹ ⫹ ⫹ ⫹ ⫹ ⫹ ⫺ ⫹ ⫹ ⫹ ⫹ ⫺ ⫺ ⫹ ⫹ ⫺ ⫺ ⫺ ⫺ ⫺ ⫺ ⫺ ⫺ ⫺ ⫺ ⫺ ⫺ ⫺ ⫺ ⫺ ⫺ ⫺ ⫺ ⫺ ⫺ ⫺ ⫺ ⫺ ⫹ ⫹ ⫹ ⫺ ⫹ ⫹ ⫺ ⫹ ⫹ ⫹ ⫹ ⫹ ⫹ ⫹ ⫹ ⫹ ⫹ ⫺ ⫹ ⫹ ⫹ ⫹ ⫺ ⫺ ⫺ ⫺ ⫺ ⫺ ⫺ ⫹ ⫺ ⫺ ⫺ ⫹ ⫺ ⫹ ⫹ ⫺ ⫺ ⫹ ⫺ ⫺ ⫺ ⫹ ⫹ ⫺ ⫺ ⫺ ⫺ ⫺ ⫹ ⫹ ⫹ ⫹ ⫺ ⫹ ⫺ ⫺ ⫺ ⫺ ⫺ ⫺ ⫺ ⫺ ⫺ ⫺ ⫺ ⫺ ⫹ ⫹ ⫹ ⫹ ⫺ ⫹ ⫺ ⫹ ⫺ ⫺ ⫺ ⫹ 75 0 33 84 20 Biochemical phenotype NE⫹DA NE⫹DA NE NE⫹DA NE NE NE NE⫹DA NE⫹DA (⫹E) NE⫹DA NE⫹DA NE⫹DA NE⫹DA NE NE NE⫹DA none none NE⫹DA NE DA NE⫹DA (⫹E) NE⫹DA NE NE NE none NE NE Elevated (marked as ⫹) and normal (marked as ⫺) concentrations of catecholamines and their metabolites at evaluation of metastatic disease (all but no. 16) and primary nonmetastatic PHEO (no. 16). Patients 8 and 14 were evaluated after chemotherapy. NE, Norepinephrine; E, epinephrine; DA, dopamine; NMN, normetanephrine; MN, metanephrine; CgA, chromogranin A. Timmers et al. • SDHB-Related Paraganglioma spread metastatic disease from extraadrenal PGL and largely elevated levels of norepinephrine and dopamine had additional elevation of plasma epinephrine and/or metanephrine. In the first patient (no. 9), plasma norepinephrine and dopamine were increased to 55 and 4 times the upper reference limit of normal, respectively, whereas plasma epinephrine was normal and plasma metanephrine was elevated to twice the upper limit, respectively. The second patient (no. 22) with largely increased plasma norepinephrine (40 times the upper limit) and dopamine (25 times the upper limit) also had mildly elevated plasma levels of epinephrine and metanephrine (both two times the upper limit) on one occasion. Plasma concentrations of chromogranin A were elevated in 13 of 16 patients (81%) and 10 of 13 patients (77%) with metastatic disease (Table 3). Genotype-phenotype correlation In 29 index patients, 20 different sequence variants of the SDHB gene were found (Table 1), nine of which had been previously reported as disease-causing mutations by others (8, 9, 12, 13, 24 –29). Eleven allelic variants were identified by our group, eight of which were published previously (18). Of these 11 variants, nine are very likely to represent diseasecausing mutations for the following reasons: five were also found in other patients with PGL (no. 4, 8, 11, 14, 18, 20, 24, 26, 29), two resulted in a frameshift causing a premature stop codon and a truncated protein (no. 7, 21), one was located in a splice site donor site (no. 3), and one in a splice site acceptor site (no. 25). The latter two splice site mutations are likely to interfere with RNA processing. In addition, the p.Val140Phe allelic variant, which was present in five patients (Table 1), was absent in 100 control subjects. Whether the missense mutations observed in the remaining two patients (no. 2 and 13) with new variants represent disease-causing mutations remains to be confirmed. In the first patient (no. 2) the variant was located close to a splice acceptor consensus region, whereas the variant in second patient (no. 13) causes substitution of an amino acid in a strongly conserved region of the protein. Family history of both patients was negative for PGL. Additional genetic testing for additional mutations of SDHD, RET, and VHL genes was performed in 21, 20, and 19 patients, respectively. All results were negative. Genotype-phenotype correlations among patients with SDHB mutations in different exons did not reveal obvious differences for age at presentation, biochemical phenotype, primary tumor size and location, distribution of metastatic lesions, or presence of additional head and neck PGLs (Fig. 1). Discussion Important information on the clinical characteristics and penetrance of different SDH-related PGL syndromes among index cases and their family members was gathered by large multinational PGL study consortia (8, 9, 12). In these reports, a particularly severe clinical phenotype of tumors with high malignant potential was observed in carriers of a mutation in the SDHB gene. We present the first single-center evaluation of genetic, clinical, and biochemical characteristics of a large group of patients with SDHB-related PGL. Early rec- J Clin Endocrinol Metab, March 2007, 92(3):779 –786 783 ognition of features pointing toward SDHB-related disease is important because this diagnosis warrants aggressive therapy and intensive follow-up. Clinical presentation The majority of patients had one or more symptoms related to catecholamine excess in addition to hypertension. However, only one third had the classical triad of headache, palpitations, and diaphoresis. In more than half of the patients, the clinical picture at initial presentation was dominated by problems caused by space-occupying effects of the tumor, including pain or discomfort, deep venous thrombosis, urological problems, and weight loss. These symptoms and signs are unusual in benign PHEO and PGL and probably relate to a high prevalence of large invasive tumors and metastatic disease at presentation. Space-occupying complications in patients with suspected PGL should trigger clinicians to think of an SDHB-related malignant tumor. An atypical presentation may account for the observed mean delay between the onset of symptoms and the diagnosis of 4.5 yr. The majority of the currently investigated patients presented in their early 30s, which is similar to earlier observations for index cases (8). We confirm, however, that SDHBrelated tumors may also occur in young children before 10 yr of age or not until after age 65 yr (11, 27). The age-related penetrance among SDHB mutation carriers was found to be 29% by 30 yr of age and 45% by age 40 yr (8). Genetic and/or environmental factors responsible for this large variability in penetrance are unknown. Only 10% of the currently investigated patients had a family history of PGL, compared with 37% of patients in a previous report (8). In the same study, screening of asymptomatic SDHB-positive relatives identified tumors in 11% (8). We agree with the notion that all first-degree family members of patients with SDHB-associated PGL should be offered genetic testing (30). We are currently extending our genetic, clinical, and biochemical studies to the patients’ relatives. Our findings emphasize that a negative family history of PHEO and PGL by no means rules out the presence of an SDHB mutation. The prevalence of SDHB mutations in apparently sporadic nonsyndromic PHEO is 4 –7% (12, 13, 31). It is in the patients lacking a positive family history that clinicians depend on other clinical, biochemical, and radiological clues for SDHB mutations. Familial PGL syndrome may be expected from the finding of additional head and neck PGL, which are present in up to 31% of SDHB mutation carriers (8, 9). In addition, 80% of SDHB-associated PGL are located in extraadrenal abdominal, intrapelvic, or thoracic locations (12). Tumors are more often multifocal and are usually large, with diameters of around 9 cm (12). Among the patients in the current study, only 10% had an additional head or neck PGL and as many as 97% of the primary tumors were in extra-adrenal locations, with a mean diameter of nearly 8 cm. Biochemical phenotype Evaluation of the biochemical phenotype of PGL mainly revealed hypersecretion of norepinephrine and/or dopamine. Our findings of predominant hypersecretion of nor- 784 J Clin Endocrinol Metab, March 2007, 92(3):779 –786 Timmers et al. • SDHB-Related Paraganglioma FIG. 1. Phenotype of index patients with PHEO according to SDHB mutation. The eight exons of SDHB are represented diagrammatically. Missense mutations are shown in the upper portion of the figure, and truncating or splice site mutations are shown in the lower portion. The phenotype observed in each patient is represented by a unit of four boxes, with the patient number shown above. DA producing, Hypersecretion of dopamine (⫾ other catecholamines). epinephrine are consistent with the notion that extraadrenal PGL rarely secrete epinephrine (32). This probably reflects a decreased expression of phenylethanolamine-N-methyltransferase, the enzyme that converts norepinephrine to epinephrine (33). According to limited information on the biochemical phenotype of SDHB-related PGL in a previous report (8), six of 30 patients showed elevated urinary excretion of both epinephrine and norepinephrine, whereas one of 30 patients showed elevations confined to urinary epinephrine. It is not mentioned whether elevated urinary epinephrine levels were found in adrenal or extraadrenal tumors. Cosecretion of dopamine, which was present in half of the patients with norepinephrine hypersecretion, is mainly found in multifocal or metastatic extraadrenal PGL (14). In addition, increased excretion of dopamine was shown to predict malignant potential in preoperative patients with apparently nonmetastatic PGL (34). Exclusive overproduction of dopamine, as found in one patient, is rare and mainly occurs in extraadrenal PGL (14, 16, 17). As observed in the case we present here, these patients have an atypical presentation, lacking symptoms of catecholamine excess and hypertension (16). In clinical practice, measurement of plasma levels of dopamine or its O-methylated metabolite methoxytyramine should be considered for identification of tumors that predominantly produce dopamine but only in patients with an atypical presentation in whom PGL is strongly suspected despite normal plasma and urinary levels of other catecholamines, and the catecholamine O-methylated metabolites, normetanephrine, and metanephrine (14). Patients with PGL who lack symptoms of catecholamine excess pose a significant diagnostic challenge (15). Such clinically silent tumors may occur in PGLs that do not produce catecholamines, in those that produce and metabolize, but do not secrete catecholamines, and those that produce dopamine but not other catecholamines (14 –16). The diagnosis of biochemically silent tumors, i.e. tumors that either do not Timmers et al. • SDHB-Related Paraganglioma produce or do not secrete catecholamines, is usually delayed until advanced metastatic disease, when complications of space-occupying lesions occur. This was also the case in the three patients with biochemically silent tumors in the current study. In this respect, these SDHB-related extraadrenal abdominal PGLs appear to share features with parasympathetic head and neck PGLs, which are also usually biochemically silent (35). These tumors may arise from subsets of cells that lack the ability to produce, metabolize, and secrete catecholamines. Alternatively, tumor cells may lose this ability due to dedifferentiation before the tumor is big enough to secrete significant amounts of catecholamines. For the monitoring of these biochemically silent PGLs, plasma levels of chromogranin A may provide an alternative biochemical parameter (36). Plasma chromogranin was positive in two of the three patients’ tumors that did not produce catecholamines. SDHB mutations and malignant disease Of the patients described in our study, all but one (97%) developed metastatic lesions of PGL at a mean interval of 2.7 yr after the diagnosis. The finding of a very high rate of malignant PGL among SDHB mutation carriers is due to selection bias of this referral-based study. In the majority of cases, the actual reason for referral to the NIH was evaluation and treatment of metastatic disease. However, among previously described patients with SDHB-associated PHEO or abdominal/thoracic PGL, the rates of malignancy were also high: 11 of 32 (34%) (9), 15 of 21 (71%) (12), and 18 of 48 (37.5%) (8). In nearly one third of cases, though, malignant disease was already evident at the initial diagnosis of PHEO/ PGL, which is similar to the previous finding of 22% (8). Apart from malignant PGL, SDHB mutations have been suggested to be associated with malignant tumors of the extraparaganglial system. Among 53 SDHB mutation carriers, two patients from the same family had renal clear cell carcinoma at young age and one patient with a different mutation had a papillary thyroid carcinoma at age 14 yr (9, 37). These associations, however, were not confirmed by more recent studies (8, 12) including the present one. Previously, genotype-phenotype correlations failed to distinguish differences in tumor location and malignant potency of SDHB-related PGL between different mutations (8). In addition, clinical phenotypes may largely differ between family members with the same mutation. In the present study, features that are associated with aggressive tumor behavior, including young age at presentation, large tumor size, metastatic disease at presentation, and hypersecretion of dopamine, were equally distributed among patients with missense vs. truncating mutations and were independent of exon locations. Apart from intragenic mutations, there are two reports on five patients with extraadrenal PGL related to large deletions of the SDHB gene (38, 39). These whole gene or partial deletions, with a possible hot spot in the first exon, remain undetected by conventional SDHB gene analysis. Because data on such deletion families are still limited, it remains to be elucidated whether this genotype is associated with a phenotype distinct from intragenic SDHB mutations. J Clin Endocrinol Metab, March 2007, 92(3):779 –786 785 Conclusions SDHB-associated PHEO and PGL is characterized by a high malignant potency, warranting aggressive therapy, strict follow-up, and family screening. The diagnosis may be delayed by a negative family history and an atypical clinical presentation with signs and symptoms that are predominantly related to tumor growth rather than to catecholamine excess. The biochemical phenotype usually consists of hypersecretion of norepinephrine and/or dopamine, but 10% of tumors are biochemically silent. The clinical expression of these tumors in individual patients cannot be predicted by the type and location of the SDHB gene mutation. Acknowledgments We thank Diana Benn for helpful discussions and feedback to the manuscript. We thank Thanh-Truc Huynh for her technical assistance. Received October 24, 2006. Accepted December 21, 2006. Address all correspondence and requests for reprints to: Karel Pacak, M.D., Ph.D., D.Sc., Head, Section on Medical Neuroendocrinology, Reproductive Biology and Medicine Branch, National Institute of Child Health and Human Development, 10 Center Drive, Building 10, CRC, Room 1-E 3140, MSC 1109, Bethesda, Maryland 20892-1109. E-mail: karel@mail.nih.gov. This work was supported by the Intramural Research Program of the National Institute of Child Health and Human Development/National Institutes of Health. Disclosure Statement: The authors have nothing to disclose. References 1. DeLellis RA, Lloyd RV, Heitz PU, Eng C 2004 Pathology and genetics: WHO classification of tumours of endocrine organs. Oxford, UK: Oxford University Press 2. Pacak K, Keiser H, Eisenhofer G 2005 Pheochromocytoma. In: Textbook of endocrinology. 5th ed. Philadelphia: Elsevier Saunders, Inc.; 2501–2534 3. Lenders JW, Eisenhofer G, Mannelli M, Pacak K 2005 Phaeochromocytoma. Lancet 366:665– 675 4. Baysal BE, Ferrell RE, Willett-Brozick JE, Lawrence EC, Myssiorek D, Bosch A, van der Mey A, Taschner PE, Rubinstein WS, Myers EN, Richard 3rd CW, Cornelisse CJ, Devilee P, Devlin B 2000 Mutations in SDHD, a mitochondrial complex II gene, in hereditary paraganglioma. Science 287:848 – 851 5. Astuti D, Latif F, Dallol A, Dahia PL, Douglas F, George E, Skoldberg F, Husebye ES, Eng C, Maher ER 2001 Gene mutations in the succinate dehydrogenase subunit SDHB cause susceptibility to familial pheochromocytoma and to familial paraganglioma. Am J Hum Genet 69:49 –54 6. Niemann S, Muller U 2000 Mutations in SDHC cause autosomal dominant paraganglioma, type 3. Nat Genet 26:268 –270 7. Schiavi F, Boedeker CC, Bausch B, Peczkowska M, Gomez CF, Strassburg T, Pawlu C, Buchta M, Salzmann M, Hoffmann MM, Berlis A, Brink I, Cybulla M, Muresan M, Walter MA, Forrer F, Valimaki M, Kawecki A, Szutkowski Z, Schipper J, Walz MK, Pigny P, Bauters C, Willet-Brozick JE, Baysal BE, Januszewicz A, Eng C, Opocher G, Neumann HP 2005 Predictors and prevalence of paraganglioma syndrome associated with mutations of the SDHC gene. JAMA 294:2057–2063 8. Benn DE, Gimenez-Roqueplo AP, Reilly JR, Bertherat J, Burgess J, Byth K, Croxson M, Dahia PL, Elston M, Gimm O, Henley D, Herman P, Murday V, Niccoli-Sire P, Pasieka JL, Rohmer V, Tucker K, Jeunemaitre X, Marsh DJ, Plouin PF, Robinson BG 2006 Clinical presentation and penetrance of pheochromocytoma/paraganglioma syndromes. J Clin Endocrinol Metab 91:827– 836 9. Neumann HP, Pawlu C, Peczkowska M, Bausch B, McWhinney SR, Muresan M, Buchta M, Franke G, Klisch J, Bley TA, Hoegerle S, Boedeker CC, Opocher G, Schipper J, Januszewicz A, Eng C 2004 Distinct clinical features of paraganglioma syndromes associated with SDHB and SDHD gene mutations. JAMA 292:943–951 10. Young AL, Baysal BE, Deb A, Young Jr WF 2002 Familial malignant catecholamine-secreting paraganglioma with prolonged survival associated with mutation in the succinate dehydrogenase B gene. J Clin Endocrinol Metab 87:4101– 4105 11. Pham TH, Moir C, Thompson GB, Zarroug AE, Hamner CE, Farley D, van Heerden J, Lteif AN, Young Jr WF 2006 Pheochromocytoma and paraganglioma in children: a review of medical and surgical management at a tertiary care center. Pediatrics 118:1109 –1117 786 J Clin Endocrinol Metab, March 2007, 92(3):779 –786 12. Amar L, Bertherat J, Baudin E, Ajzenberg C, Bressac-de Paillerets B, Chabre O, Chamontin B, Delemer B, Giraud S, Murat A, Niccoli-Sire P, Richard S, Rohmer V, Sadoul JL, Strompf L, Schlumberger M, Bertagna X, Plouin PF, Jeunemaitre X, Gimenez-Roqueplo AP 2005 Genetic testing in pheochromocytoma or functional paraganglioma. J Clin Oncol 23:8812– 8818 13. Neumann HP, Bausch B, McWhinney SR, Bender BU, Gimm O, Franke G, Schipper J, Klisch J, Altehoefer C, Zerres K, Januszewicz A, Eng C, Smith WM, Munk R, Manz T, Glaesker S, Apel TW, Treier M, Reineke M, Walz MK, Hoang-Vu C, Brauckhoff M, Klein-Franke A, Klose P, Schmidt H, Maier-Woelfle M, Peczkowska M, Szmigielski C, Eng C 2002 Germ-line mutations in nonsyndromic pheochromocytoma. N Engl J Med 346:1459 –1466 14. Eisenhofer G, Goldstein DS, Sullivan P, Csako G, Brouwers FM, Lai EW, Adams KT, Pacak K 2005 Biochemical and clinical manifestations of dopamine-producing paragangliomas: utility of plasma methoxytyramine. J Clin Endocrinol Metab 90:2068 –2075 15. Bonnet S, Durand X, Baton O, Gimenez-Roqueplo AP, Baudin E, Visset J, Algayres JP, Baranger B 2006 Malignant hereditary paraganglioma: problems raised by nonfunctional forms management. Ann Chir 131:626 – 630 16. Proye C, Fossati P, Fontaine P, Lefebvre J, Decoulx M, Wemeau JL, Dewailly D, Rwamasirabo E, Cecat P 1986 Dopamine-secreting pheochromocytoma: an unrecognized entity? Classification of pheochromocytomas according to their type of secretion. Surgery 100:1154 –1162 17. Koch CA, Rodbard JS, Brouwers FM, Eisenhofer G, Pacak K 2003 Hypotension in a woman with a metastatic dopamine-secreting carotid body tumor. Endocr Pract 9:310 –314 18. Brouwers FM, Eisenhofer G, Tao JJ, Kant JA, Adams KT, Linehan WM, Pacak K 2006 High frequency of SDHB germline mutations in patients with malignant catecholamine-producing paragangliomas: implications for genetic testing. J Clin Endocrinol Metab 91:4505– 4509 19. Baysal BE, Willett-Brozick JE, Lawrence EC, Drovdlic CM, Savul SA, McLeod DR, Yee HA, Brackmann DE, Slattery 3rd WH, Myers EN, Ferrell RE, Rubinstein WS 2002 Prevalence of SDHB, SDHC, and SDHD germline mutations in clinic patients with head and neck paragangliomas. J Med Genet 39:178 –183 20. Willemsen JJ, Sweep CG, Lenders JW, Ross HA 2003 Stability of plasma free metanephrines during collection and storage as assessed by an optimized HPLC method with electrochemical detection. Clin Chem 49:1951–1953 21. Lenders JW, Eisenhofer G, Armando I, Keiser HR, Goldstein DS, Kopin IJ 1993 Determination of metanephrines in plasma by liquid chromatography with electrochemical detection. Clin Chem 39:97–103 22. Eisenhofer G, Goldstein DS, Stull R, Keiser HR, Sunderland T, Murphy DL, Kopin IJ 1986 Simultaneous liquid-chromatographic determination of 3,4dihydroxyphenylglycol, catecholamines, and 3,4-dihydroxyphenylalanine in plasma, and their responses to inhibition of monoamine oxidase. Clin Chem 32:2030 –2033 23. Linnoila RI, Keiser HR, Steinberg SM, Lack EE 1990 Histopathology of benign versus malignant sympathoadrenal paragangliomas: clinicopathologic study of 120 cases including unusual histologic features. Hum Pathol 21:1168 – 1180 24. Bayley JP, van Minderhout I, Weiss MM, Jansen JC, Oomen PH, Menko FH, Pasini B, Ferrando B, Wong N, Alpert LC, Williams R, Blair E, Devilee P, Taschner PE 2006 Mutation analysis of SDHB and SDHC: novel germline mutations in sporadic head and neck paraganglioma and familial paraganglioma and/or pheochromocytoma. BMC Med Genet 7:1 25. Cascon A, Ruiz-Llorente S, Fraga MF, Leton R, Telleria D, Sastre J, Diez JJ, Timmers et al. • SDHB-Related Paraganglioma 26. 27. 28. 29. 30. 31. 32. 33. 34. 35. 36. 37. 38. 39. Martinez Diaz-Guerra G, Diaz Perez JA, Benitez J, Esteller M, Robledo M 2004 Genetic and epigenetic profile of sporadic pheochromocytomas. J Med Genet 41:e30 Benn DE, Croxson MS, Tucker K, Bambach CP, Richardson AL, Delbridge L, Pullan PT, Hammond J, Marsh DJ, Robinson BG 2003 Novel succinate dehydrogenase subunit B (SDHB) mutations in familial phaeochromocytomas and paragangliomas, but an absence of somatic SDHB mutations in sporadic phaeochromocytomas. Oncogene 22:1358 –1364 Elston MS, Benn D, Robinson BG, Conaglen JV 2006 An apparently sporadic paraganglioma with an SDHB gene germline mutation presenting at age 68 years. Intern Med J 36:129 –131 Gimenez-Roqueplo AP, Favier J, Rustin P, Rieubland C, Crespin M, Nau V, Khau Van Kien P, Corvol P, Plouin PF, Jeunemaitre X 2003 Mutations in the SDHB gene are associated with extra-adrenal and/or malignant phaeochromocytomas. Cancer Res 63:5615–5621 Zantour B, Guilhaume B, Tissier F, Louvel A, Jeunemaitre X, GimenezRoqueplo AP, Bertagna X 2004 A thyroid nodule revealing a paraganglioma in a patient with a new germline mutation in the succinate dehydrogenase B gene. Eur J Endocrinol 151:433– 438 Young Jr WF, Abboud AL 2006 Editorial: paraganglioma—all in the family. J Clin Endocrinol Metab 91:790 –792 Jimenez C, Cote G, Arnold A, Gagel RF 2006 Review: should patients with apparently sporadic pheochromocytomas or paragangliomas be screened for hereditary syndromes? J Clin Endocrinol Metab 91:2851–2858 Eisenhofer G, Lenders JW, Goldstein DS, Mannelli M, Csako G, Walther MM, Brouwers FM, Pacak K 2005 Pheochromocytoma catecholamine phenotypes and prediction of tumor size and location by use of plasma free metanephrines. Clin Chem 51:735–744 Feldman JM, Blalock JA, Zern RT, Wells Jr SA 1979 The relationship between enzyme activity and the catecholamine content and secretion of pheochromocytomas. J Clin Endocrinol Metab 49:445– 451 John H, Ziegler WH, Hauri D, Jaeger P 1999 Pheochromocytomas: can malignant potential be predicted? Urology 53:679 – 683 Koch CA, Vortmeyer AO, Zhuang Z, Brouwers FM, Pacak K 2002 New insights into the genetics of familial chromaffin cell tumors. Ann NY Acad Sci 970:11–28 Grossrubatscher E, Dalino P, Vignati F, Gambacorta M, Pugliese R, Boniardi M, Rossetti O, Marocchi A, Bertuzzi M, Loli P 2006 The role of chromogranin A in the management of patients with phaeochromocytoma. Clin Endocrinol (Oxf) 65:287–293 Vanharanta S, Buchta M, McWhinney SR, Virta SK, Peczkowska M, Morrison CD, Lehtonen R, Januszewicz A, Jarvinen H, Juhola M, Mecklin JP, Pukkala E, Herva R, Kiuru M, Nupponen NN, Aaltonen LA, Neumann HP, Eng C 2004 Early-onset renal cell carcinoma as a novel extraparaganglial component of SDHB-associated heritable paraganglioma. Am J Hum Genet 74:153–159 Cascon A, Montero-Conde C, Ruiz-Llorente S, Mercadillo F, Leton R, Rodriguez-Antona C, Martinez-Delgado B, Delgado M, Diez A, Rovira A, Diaz JA, Robledo M 2006 Gross SDHB deletions in patients with paraganglioma detected by multiplex PCR: a possible hot spot? Genes Chromosomes Cancer 45:213–219 McWhinney SR, Pilarski RT, Forrester SR, Schneider MC, Sarquis MM, Dias EP, Eng C 2004 Large germline deletions of mitochondrial complex II subunits SDHB and SDHD in hereditary paraganglioma. J Clin Endocrinol Metab 89:5694 –5699 JCEM is published monthly by The Endocrine Society (http://www.endo-society.org), the foremost professional society serving the endocrine community.