COMPUTATIONAL ANALYSIS OF polyether
advertisement

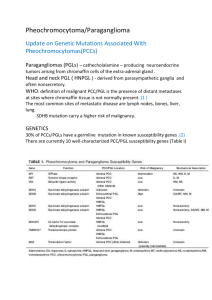
COMPUTATIONAL ANALYSIS OF POLYETHER-POLYOLS TYPE POLYGLYCEROLS FOR TISSUE ENGINEERING APPLICATIONS Passos, E. D.1, de Queiroz, A. A. A.2 1, 2 Center for Research and Innovation in Advanced Materials biofunctional – Federal University of Itajubá – Unifei, Itajubá (MG), Brazil esdrasdp@gmail.com ABSTRACT The development of scaffolds for tissue engineering applications has recently focused on the design of biomimetic materials that are able to interact with surrounding tissues by biomolecular recognition. When scaffolds are exposed to biological environments, extracellular matrix (ECM) proteins are adsorbed on the surface and then cells indirectly interact with the synthetic surface through the adsorbed ECM proteins. A synthetic cardiovascular graft can be used for the replacement of damaged native tissues in cardiac or peripheral bypass surgery when there is limited supply of autologous tissues. However, synthetic vascular grafts generally exhibit a lower patency rate than natural tissues mainly due to thrombus formation following the implantation. Computational methods for design scaffolds with improved haemocompatibility has become of growing importance as alternative approaches to animal experimentation. In this work molecular dynamics (MD) was used to simulate the interaction between human serum albumin (HSA) and human serum fibrinogen (HFb) and polyether-polyols type poly(glycerol)´s, (PGL). The simulation was made by using GROMACS and the media were aqueous solution, 37ºC and 1 atmosphere of pressure. Our results show that the more effective interactions occur between PGL and HSA than HFb. MD symulations indicates that PGL would be a class of consistent, economical, and high performance multivalent scaffold 3D tissue constructs for soft-tissue engineering and regenerative medicine. Key words: Molecular Dynamics Simulation, Tissue Engineering, Aliphatic Polyether’s, Scaffolds. 1. INTRODUCTION. The twentieth century was a watershed for the development of lifesaving surgical procedures and techniques that also vastly improved the quality of human life. The clinical surgeries were informed by the extraordinary explosion in knowledge of human anatomy, physiology, and biology. All the knowledge converged to a complex array of pre-existing lines of work from the interdisciplinary between the clinical medicine, engineering, and science. Actually, an intense research has been devoted to the development of scaffolds in the area of medicine that has come to known as tissue engineering [1-5]. The success of polymeric scaffolds is determined by the response it elicits from the surrounding biological environment. This response is governed, to a large extent, by the surface properties of the scaffold. Multiple approaches have been developed to provide micrometer to nanometer scale alterations in polymer scaffolds to enable improved protein and cell interactions. Chemical modification of polymeric scaffold by physical or chemical methods is one of the upcoming approaches that have been employed successfully to providing cell adhesion and growth on polymeric scaffolds [612]. Over the past twenty years, our laboratory has developed expertise in the fabrication of synthetic scaffolds with tailored chemistries for a variety of tissue engineering applications. These novel materials are based on hyperbranched and dendritic poly(glycerols) (PGL) [13-15] (Figure 1). We have demonstrated these materials to be non-toxic to surrounding cells and tissues [16-18]. Additionally, as these materials are based on naturally-occurring compounds, they degrade over time in the body to natural products which can be safely and efficaciously excreted. Thus, after implantation of PGL-based scaffolds, no further surgery would be needed for removal of the material, thereby reducing discomfort to the patient and cost of the procedure. Figure 1- Illustration of poly(glycerol) (PGL) (A), Hyperbranched poly(glycerol) (HPGL) (B) and Dendritic poly(glycerol) (PGLD) (C). One of the important criteria for a scaffold is that it should be able to serve as an anchor for stem cells to be retained near the injury site, instead of allowing cells to be attracted and migrate to healthy regions. Protein absorption on substrates is one of the critical factors to control cell adhesion [19-21]. Such strong affinity to protein molecules may be an indicative to the cell adhesion capability of scaffold. The focus of this work is the study of PGL – protein interactions. It is based on two concepts: (i) that an atomic level of detail will be required if the true effects of polymers on protein behavior are to be completely elucidated and (ii) that in place of direct experimental advances, the best way to approach this problem is through the use of molecular simulation techniques, replacing animal experimentation . The use of molecular dynamics (MD) simulations allows the physicochemical nature of molecular interactions to be observed at a level of resolution that is currently beyond reach experimentally. 2. MATERIALS AND METHODS 2.1. Molecular Dynamics Simulation Details All molecular dynamics (MD) simulations were carried out using GROMACS 4 software [21]. In each simulated system, water was modeled with the TIP3P model [22] and proteins were modeled with the OPLS-AA force field [23] implemented in GROMACS; each system also included 100 mM NaCl with literature parameters used to describe the ions [24-25] at a system pH of 7.0. NaCl was used because they were the predominate ions used in biological human organism. The system size of each simulation was dependent on the specific volume of each protein, determined by HYDROPRO [26]; the final volume of the box was adjusted so that each system contained 100, 200 or 300 mg/mL PGL 3,350 with 6, 12 and 18 PGL molecules, respectively. All simulations used a dodecahedral box with approximately an 80 Å image distance – the distance from the center of one system to the next – and applied with periodic boundary conditions. All PGL structures were first energy minimized using the steepest descent algorithm for 1000 steps and then incrementally heated to 310 K (37 ºC) over 500 ps in the NPT ensemble; during this initial period, a pressure of 1 atm was maintained with the Berendsen barostat [58] and temperature was maintained with the Berendsen thermostat [27]. Directly following, each system was equilibrated for a further 10.5 ns in the NPT ensemble, switching to the canonical coupling schemes of the ParrinelloRahman barostat [28] at 1 atm pressure and the Nosé-Hoover thermostat [29-30] at 310 K. Each production simulation lasted 500 ns in the canonical coupling scheme. Cutoffs for both the short-range electrostatic and van der Waals interactions were set to 10 Å, and the long-range electrostatic interactions utilized the Particle Mesh Ewald (PME) method [31]. A 2.5 fs time step was employed with all covalent bonds constrained using the LINCS algorithm [32]. All atomic coordinates were saved at 1 ps intervals for subsequent analysis. Two different proteins were simulated; Human Serum Albumin (HSA) and Human Serum Fibrinogen (HFb), each was simulated alone in aqueous solution and with three different concentrations of PGL 3,350 (100, 200 and 300 mg/mL, again corresponding to 6, 12 and 18 monomers of PGL 3,350, respectively). All protein structures were obtained from the Protein Data Bank [29]. 3. RESULTS E DISCUSSION 3.1. Structural Stability of the Systems In order to show the reliability of MD experiments results obtained from our simulation we followed up temperature changes of the system during simulation (Figure 2). The constancy of temperature at 310K indicates the stability of the system. Changes in total and kinetic energy also confirmed the satiability of our system. In this context, the ratio of Kinetic/Total energy is a bit better index for the prevalence of stability in system. This ratio in our system is completely constant and it did not exceed 0.05 which in turn show the conservation of energy during simulation (data not shown). Figure 2- Changes in system temperature during simulation around 310K. The data were obtained in aqueous solution, 310K and 1 atmosphere of pressure. From misalliances data obtained from trajectory analysis that could be easily interpreted are surface accessible area, gyration radius and RMSD changes of protein during simulation. The first parameter, the accessible surface area (ASA), is the surface area in Å2 of PGL that is accessible to a non-aqueous solvent [17]. Any change in ASA during simulation indicates structural changes in PGL structure (tertiary). Figure 3 show that PGL with n= 2 in contrast to n >2 more effectively decreases surface accessible area of polyglycerol. This finding indicates that the hydrogen bonding in poly(glycerols) with n<10 probably acts via increaseing polymer compactness that in turn leads to decrease in disturbance of polymer structure and necessarily induces increase in random coil proportion. Figure 3- The surface accessible area of PGL in the presence of different inhibitors. The data were obtained in aqueous solution, 310K and 1 atmosphere of pressure. The next parameter we studied was the radius of gyration of PGL´s or Rg. The size of a polymer molecule can be described by the radius of gyration which is the trace of the tensor of gyration given as: where rα is the position of site α, rCM is the position of the molecular centre of mass, mα is the mass of site α and the angle brackets denote an ensemble average. The radius of gyration (Rg) is thus the average distance from the centre of gravity to the chain segment. It can be measured experimentally using different techniques and is dependent on molecular weight. Polymers with higher degree of polymerization normally have larger radius of gyration. Furthermore for a given value of molecular weight, depending on the branching topology, the value of the radius of gyration for different branched polymers can vary. Figure 4 show the Rg change during simulation as a function of PGL concentration. Rg describes the overall spread of the molecule and determines the PGL structure compactness, the more Rg the less compactness of PGL structure. As it is evident the decrease in polymerization degree (n) decreases the PGL radius during simulation which is in confirmatory with surface accessible area changes (Fig. 3). Figure 4- Dependence of gyration radius of PGL with different polymerization degree. The data were obtained in aqueous solution at PGL concentration of 300 mg/mL, 310K and 1 atmosphere of pressure. We also examined the influence of n for a fixed polymer concentration of 300 mg/L as shown in Figure 5. This leads to Rg = 1.98n0.48, where the exponent of 0.48 is in comparison to the predicted value of 1/2. The exponent of 0.48 suggests that the PGL chains are quite flexible in the semidilute solution and is consistent with the single chain density–density correlation function, modeled by the Debye structure factor. However, more experiments are needed to confirm this result over a wider n range. Figure 5- Dependence of Rg on degree of polymerization at PGL concentration of 300 mg/mL. The development of biomaterials for tissue engineering applications has recently focused on the design of biomimetic materials that are able to interact with surrounding tissues by biomolecular recognition [33-35]. When biomaterials are exposed to biological environments, extracellular matrix (ECM) proteins are non-specifically adsorbed on the surface of nearly all the biomaterials, and then cells indirectly interact with the biomaterial surface through the adsorbed ECM proteins. The design of biomimetic materials is an attempt to make the materials such that they are capable of eliciting specific cellular responses and directing new tissue formation mediated by specific interactions, which can be manipulated by altering design parameters instead of by non-specifically adsorbed ECM proteins. A synthetic cardiovascular graft can be used for the replacement of damaged native tissues in cardiac or peripheral bypass surgery when there is limited supply of autologous tissues. However, synthetic vascular grafts generally exhibit a lower patency rate than natural tissues mainly due to thrombus formation and intimal hyperplasia following the implantation [36]. In addition, the failure rate of synthetic grafts increased particularly in small diameter applications in which the internal diameter is less than 6 mm. Thus, the design of vascular grafts with improved biocompatibility is critical for cardiovascular tissue engineering. Generally, blood coagulates and causes blood clotting when it encounters foreign synthetic surfaces. This phenomenon is assumed to begin with the initial absorption of blood proteins, which is followed by platelet adhesion and activation of the coagulation pathway, leading to thrombus formation. Studies have pointed that the significantly reduction of thrombus formation onto synthetic polymers surfaces is a specifically albumin adsorption. This specific absorption was postulated to increase the amount of albumin on the surface and to decrease the number of platelets on the surface available to aggregate into a thrombus [37]. Figure 6 show the Root Mean Square Displacement (RMSD) of PGL-HSA and PGL-HFb complexes. RMSD changes in Figure 6 shows that the PGL – proteins complexes reaches the equilibrium state over 1 ps of simulation. The more increase in RMSD means the more interaction of protein with PGL during simulation as it seen for HSA (Fig. 6) and this is reflected in more changes in PGL to proteins distance. Figure 6- Root Mean Square Displacement (RMSD) changes of PGL in the presence of HSA (A) and HFb (B). The data were obtained in aqueous solution, 310K and 1 atmosphere of pressure. Figure 7 shows that the RMSDs of HAS in 300 mg/mL of PGL 3,350 are either lower or equal to those in solutions without PGL 3,350. Not only does PGL 3,350 appear not to unfold the HSA, therefore, but decreased the RMSD of the protein backbone. Figure 7- RMSD analysis for HSA. The RMSD compare 0 mg/mL (gray) to 300 mg/mL (red) PEG 3,350. CONCLUSIONS Overally in case of poly(glycerol) polymers we can conclude that HSA bind preferentially to PGL increasing its compactness, increasing its random structures and its surface accessible area. The decreasing gyration radius of PGL with polymerization degree convert the native, relaxed and functional structure of polyglycerol to deformed. The MD simulation results indicates that more effective interactions occur between PGL and HSA than HFb. MD symulations suggests that PGL would be a class of consistent, economical, and high performance multivalent scaffold 3D tissue constructs for soft-tissue engineering and regenerative medicine. Acknowledgments The authors are grateful for funding from the Capes, Finep and CNPq by the financial support. REFERENCES [1] YANNAS, I. V. Tissue and Organ Regeneration in Adults. New York (EUA), Springer-Verlag, 2001. [2] LANGER, R. & Vacanti, J. P. Tissue engineering. Science 260: 920-6, 1993. [3] GRIFFITH, L. G. & NAUGHTON, G. Tissue engineering--current challenges and expanding opportunities. Science 295: 1009-14, 2002. [4] PALSSON, B. O.; BHATIA, S. N. Tissue Engineering. New Jersey: Pearson P rentice Hall, 2004. [5] CHAPEKAP, M. Tissue Engineering: Challenges and opportunities, Journal of Biomedical Materials Research (Applied Biomaterials); 53, 617-620, 2000. [6] MA, P.X. Scaffolds for tissue fabrication. Materials Today 7: 30 –40, 2004. [7] SHI, H. & RATNER BD. Template recognition of protein-imprinted polymer surfaces. J Biomed Mater Res; 49: 1–11, 2000. [8] BOYAN, B.D., HUMMERT, T.W., DEAN, D.D., SCHWARTZ, Z. Role of material surfaces in regulating bone and cartilage cell response. Biomaterials 17: 137–146, 1996. [9] ITO Y. Surface micropatterning to regulate cell functions. Biomaterials 20: 2333–2342, 1999. [10] MANN B.K., TSAI, A.T., SCOTT-BURDEN T. & WEST J.L. Modification of surfaces with cell adhesion peptides alters extracellular matrix deposition. Biomaterials 20:2281–2286, 1999. [11] HENCH LL, POLAK JM. Third-generation biomedical materials. Science 295: 1014 –1017, 2002 [12] PATRICK CW, MIKOS AG, MCINTIRE LV.; Prospects of tissue engineering. In: Frontiers in Tissue Engineering. Elsevier Science Ltd, Oxford. pp. 3-11, 1998. [13] MENDES MOURA R. and DE QUEIROZ, A. A. A.; Dendronized polyaniline nanotubes for cardiac tissue engineering. Artificial Organs, 2011 (In Press). [14] FERNANDES, E; ZUCOLOTTO, V.; DE QUEIROZ, A. A. A.; Electrospinning of Hyperbranched Poly-L-Lysine/PolyanilineNanofibers for Application in Cardiac Tissue Engineering. Journal of Macromolecular Science. Pure and Applied Chemistry, v. 47, p. 1203-1207, 2010. [15] FERNANDES, E.G.R., DE QUEIROZ A.A.A. A bioconjugated poliglycerol dendrimer with glucose sensing properties. J.Mater.Sci.: Mater. Med., v. 20, p. 473-479, 2009. [16] DE QUEIROZ A.A.A., BARACHO, N.C.V.; VARGAS, E.A.T.; BRITO, J. Hyperbranched poliglycerol electrospun nanofibers for wound dressing aplications. Acta Biomaterialia, v. 1, p. 1-18, 2009. [17] DE QUEIROZ A.A.A.; ABRAHAM, GUSTAVO ABEL; CAMILO, MARIA APARECIDA PIRES; HIGA, OLGA ZAZUCO; SILVA, GERALD SARAIVA; FERNÁNDEZ, MARIA DEL MAR; ROMAN, JULIO SAN . Physicochemical and antimicrobial properties of boron-complexed poliglycerol-chitosan dendrimers. J. Biom. Sci.: Polym. Edn., v. 17, n. 6, p. 689-707, 2006. [18] DE QUEIROZ A.A.A.; FERNANDES, E.G.R., ABRAHAM, G.A.; ROMAN, J.S. Antithrombogenic properties of bioconjugate streptokinase-poliglycerol dendrimers. J. Mat.Sci.: Mat. Med., v. 17, n. -, p. 105-111, 2006. [19] J.L. DEWEZ, J.B. LHOEST, E. DETRAIT, V. BERGER, C.C. DUPONT-GILLAIN, L.M. VINCENT, Y.J. SCHNEIDER, P. BERTRAND, P.G. ROUXHET, Adhesion of mammalian cells to polymer surfaces: from physical chemistry of surfaces to selective adhesion on defined patterns. Biomaterials 19: 1441–1445, 1998. [20] C.M. DEKEYSER, E. ZUYDERHOFF, R.E. GIULIANO, H.J. FEDEROFF, C. DUPONTGILLAIN CH, P.G. ROUXHET, A rough morphology of the adsorbed fibronectin layer favors adhesion of neuronal cells, J. Biomed. Mater. Res. A 87: 116–128, 2008. [21] DE QUEIROZ A.A.A.; GALLARDO, A.; ROMÁN, J.S. Vinylpyrrolidone-N,N´dimethylacrylamide water-soluble copolymers: Synthesis, physical chemical properties and proteic interactions. Biomaterials, v. 21, p. 1631-1643, 2000. [22] HESS, B.; KUTZNER, C.; VAN DER SPOEL, D.; LINDAHL, E. J. Chem. Theory Comput. 2008, 4, 435. [23] JORGENSEN, W. L.; CHANDRASEKHAR, J.; MADURA, J. D.; IMPEY, R. W.; KLEIN, M. L. J. Chem. Phys. 1983, 79, 926. [24] JORGENSEN, W. L.; MAXWELL, D. S.; TIRADORIVES, J. J. Am. Chem. Soc. 1996, 118, 11225. [25] AQVIST, J. J. Phys. Chem. 1990, 94, 8021. [26] CHANDRASEKHAR, J.; SPELLMEYER, D. C.; JORGENSEN, W. L. J. Am. Chem. Soc. 1984, 106, 903. [27] DE LA TORRE, J. G.; HUERTAS, M. L.; CARRASCO, B. Biophys. J. 2000, 78, 719. [28] BERENDSEN, H. J. C.; POSTMA, J. P. M.; VANGUNSTEREN, W. F.; DINOLA, A.; HAAK, J. R. J. Chem. Phys. 1984, 81, 3684. [29] PARRINELLO, M.; RAHMAN, A. J. Appl. Phys. 1981, 52, 7182. [30] NOSE, S. J. Chem. Phys. 1984, 81, 511. [31] HOOVER, W. G. Phys. Rev. A 1985, 31, 1695. [32] ESSMANN, U.; PERERA, L.; BERKOWITZ, M. L.; DARDEN, T.; LEE, H.; PEDERSEN, L. G. J. Chem. Phys. 1995, 103, 8577. [33] HUBBELL JA. Bioactive biomaterials. Curr Opin Biotechnol;10:123–9, 1999. [34] HEALY KE. Molecular engineering of materials for bioreactivity. Curr Opin Solid State Mater Sci 4: 381–7, 1999. [35] SAKIYAMA-ELBERT SE, HUBBELL JA. Functional biomaterials: design of novel biomaterials. Annu Rev Mater Res; 31:183–201, 2001. [36] RATCLIFFE A. Tissue engineering of vascular grafts. Matrix Biol; 19:353–7, 2000. [37] ROBERT C. EBERHART, MARK S. MUNRO, GERALDINE B. WILLIAMS, PADMAKAR V. KULKARNI, W. ALLEN SHANNON JR., BRUCE E. BRINK, WILLIAM J. FRY. Albumin Adsorption and Retention on C18-Alkyl-Derivatized Polyurethane Vascular Grafts. Artif. Organs 11(5): 375-382, 1987.