Toddler Nutrition - Mead Johnson Nutrition

LB2264 NEW 9/07
Funding for this publication provided by
©2007 Mead Johnson & Company
Toddler
Nutrition
• Nutrient Intakes of Toddlers vs Recommendations
• Metabolic Programming
• Overweight Status and Risk
• DHA in Toddler Nutrition
Toddler Nutrition
TABLE OF CONTENTS
Executive Summary . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .
4
Introduction . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .
6
Nutrient Intakes of Toddlers vs Recommendations . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .
9
Recommended Intakes . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .
10
Macronutrients . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .
11
Micronutrients . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .
14
Over Consumption of Micronutrients . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .
19
References . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .
20
Metabolic Programming . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .
23
The Intrauterine Environment . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .
24
Birth Weight . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .
24
Maternal Diabetes . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .
25
Growth . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .
25
Toddlers . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .
25
References . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .
26
Overweight Status and Risk . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .
27
Introduction . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .
28
Prevalence of Overweight in Children . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .
28
Definitions of Overweight . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .
29
Health Risks Associated with Overweight in Childhood . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .
29
Energy Imbalance . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .
29
Family and Environment . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .
31
Infant Nutrition and Growth Pattern . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .
32
What To Do?
. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .
33
References . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .
34
DHA in Toddler Nutrition . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .
37
Introduction . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .
38
Sources of DHA . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .
38
Physiological Roles for DHA . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .
39
DHA and the Growing Brain . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .
39
Indicators of DHA Status . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .
40
DHA Intakes of Toddlers . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .
40
DHA Status of Toddlers . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .
41
Summary . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .
42
References . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .
42
TA B L E O F C O N T E N T S
T O D D L E R N U T R I T I O N
Toddler Nutrition
Contributors:
Robert Baker, MD, PhD
Professor of Pediatrics
State University of New York at Buffalo
Co-Chief, Digestive Disease and Nutrition Center
Women and Children’s Hospital of Buffalo
Benjamin H. Caballero, MD, PhD
Professor of Pediatrics, International Health and Maternal and Child Health
Director, Center for Human Nutrition, Bloomberg School of Public Health
Johns Hopkins University
Barbara A. Dennison, MD
Clinical Professor of Epidemiology
State University of New York at Albany
Director, Bureau of Health Risk Reduction
Division of Chronic Disease Prevention and Adult Health
New York State Department of Health
Sheila M. Innis, PhD, MSc
Professor, Department of Pediatrics
Director, Nutrition Research Program
BC Research Institute for Children’s and Women’s Health
University of British Columbia
Rebecca Simmons, MD
Professor of Pediatrics
Center for Research on Reproduction and Women’s Health
Children’s Hospital of Philadelphia
University of Pennsylvania Medical Center
Bonny Specker, PhD
Professor, Nutrition, Food Science and Hospitality
Chair & Director, Ethel Austin Martin Program in Human Nutrition
South Dakota State University
Medical and drug information is constantly evolving because of ongoing research and clinical experience that are often subject to interpretation. While care has been taken to ensure the accuracy of the information presented, the reader is advised that Mead Johnson & Company, and the authors, editors, reviewers, contributors, and publishers of this material are not responsible for the continued currency of the information contained in this material, or any errors or omissions that might appear in this material, or for any consequences arising out of, or resulting from, the use of the material for any purpose or reason whatsoever.
Because of the dynamic nature of medical and drug information, readers are advised that decisions regarding drug or any other therapy must be based on the independent judgment of the clinician, information about a drug (eg, as reflected in the literature), and changing medical practices.
The Editors and Mead Johnson & Company
T O D D L E R N U T R I T I O N 3
4
Executive Summary
Toddlers (children ages 1 to 5 years) experience rapid growth and development. During periods of rapid growth and development, a child may be particularly vulnerable to inappropriate dietary patterns and nutrition. Experts hypothesize that insufficient or excess supply of energy and/or other nutrients during critical periods of growth may program a child to develop health conditions such as overweight, diabetes and hypertension in childhood or later in life. In addition, some micronutrient deficiencies during early life result in irreversible deficits in development.
Toddlers’ eating patterns and behaviors prompt concern about the nutritional adequacy of their diets. As toddlers transition from a liquid nutrient dense diet of predominantly breast milk and/or infant formula to a diet consisting primarily of table foods, their diets may become less dense in some nutrients. Toddlers are also learning to feed themselves and are neophobic, rejecting foods that are new because they are unfamiliar.
Parents often describe toddlers as picky eaters.
Despite the potential importance of toddler nutrition and the characteristics of toddlers’ eating patterns and behaviors, the nutritional needs of toddlers have not been well defined. Relatively little data on toddler nutrition and the long-term health consequences of toddler nutrition exist.
The Dietary Reference Intakes (DRI) are the best standards based on current scientific evidence available for evaluating toddlers’ nutrient intakes. Data indicate that young children consume more energy than DRI estimated requirements but meet recommended intakes of carbohydrate and protein. Fiber intakes, however, rarely meet recommendations. Added sugars are a potential nutritional concern because intakes of more than
20% to 25% of energy may dilute the nutrient density of children’s diets.
Intake data indicate that toddlers between the ages of 1 and 5 get recommended amounts of most vitamins and minerals. Yet pediatric health care providers should not be complacent about micronutrient intakes. Iron deserves continued attention since iron deficiency in the first years of life is relatively common and may have irreversible negative consequences on development. In addition, calcium and vitamin D are critical for bone health and peak bone mass and should receive continued emphasis. As other beverages displace milk in toddlers’ diets, calcium and vitamin D intakes decrease. Preliminary data indicate that significant numbers of toddlers approaching school age may not get recommended amounts of these nutrients. Intake data indicate that vitamin E intakes by young children are lower than recommendations. The nutritional significance of this finding is not known.
Possible over consumption of some micronutrients may be an issue for some young children. Over consumption of vitamin A deserves consideration and unwarranted supplementation should be avoided. Further data on recommended upper levels of intake for vitamins and minerals are needed since there are few data specific to toddlers.
The importance of dietary n-3 fatty acids, including docosahexaenoic acid (DHA), for infant brain and retinal development and in adult health, highlights the need to investigate DHA status and n-3 fatty acid nutrition in children, particularly those between the ages of 1 and 5 years at which time brain development is continuing.
Infants between the ages of 1 and 6 months who consume breast milk or formula with 3.7 g fat/100 mL and
0.3% of the fatty acids as DHA will receive 86 mg DHA with an intake of 780 mL of breast milk or formula per day. Recent studies have estimated that toddlers and children ages 18 to 60 months consume about
E X E C U T I V E S U M M A R Y
1.7 g alpha-linolenic acid per day and 88 mg DHA/day with the lowest intake of about 40 mg DHA/day occurring at 18 to 24 months of age. Researchers also evaluated the DHA concentration of red blood cell phosphatidylethanolamine in 18- to 60-month-old children and found these DHA levels to be lower than that of newborns, breastfed infants, or children of older ages. DHA concentration of the 18- to 60-month-old children was comparable to that of 3-month-old infants fed formula without DHA. The importance of adequate n-3 fatty acid nutrition and the relatively low DHA concentration observed in toddlers indicate that n-3 fatty acid nutrition of children ages 1 to 5 years deserves further investigation.
Overweight is a critical health care issue for toddlers and the prevalence and extent of overweight in toddlers is increasing dramatically. Children with a body mass index (BMI) at or above the 85th but less than the 95th percentile for age and sex are considered to be “at risk of overweight.” Children with a BMI at or above the 95th percentile for age and sex are considered “overweight.” Overweight contributes to numerous health conditions in childhood as well as increased morbidity and mortality in adulthood. The energy imbalance leading to the childhood obesity epidemic may be related to physical inactivity and food consumption trends (increased portion sizes, frequent consumption of fast foods and sweet beverages and decreased consumption of vegetables).
Family and environmental characteristics including television-viewing habits appear to be important predictors of overweight in children. Television viewing appears to affect weight by influencing eating behaviors, food choices, and activity patterns.
Infant nutrition and infant growth patterns may influence weight status later in childhood and adulthood. Rapid growth during early infancy has been linked to overweight later in childhood and early adulthood.
5 Breastfeeding may help protect against later obesity, but it is difficult to determine if weight differences between children and adults who were breastfed compared with those who were formula fed are due to factors in human milk, differences in characteristics of mothers who breastfeed versus those who formula feed, and/or differences in maternal feeding and parenting practices.
Many parents do not recognize that their children are overweight or at risk of overweight. In addition, pediatric health care providers may not routinely screen for overweight by measuring or plotting BMI for age. The American
Academy of Pediatrics now urges physicians to routinely screen toddlers for overweight by measuring BMI and to implement steps to help prevent this increasingly prevalent problem.
E X E C U T I V E S U M M A R Y 5
6
Introduction
Although growth velocity is greater during infancy than in toddlerhood, toddlers do experience rapid growth and development. During periods of rapid growth and development, a child may be particularly vulnerable to inappropriate dietary patterns and nutrition. Experts hypothesize that insufficient or excess supply of energy and/or other nutrients during critical windows of growth and development may program a child to develop health conditions such as overweight, diabetes, and hypertension in childhood or later in life. In addition, some micronutrient deficiencies during early life result in irreversible deficits in mental and motor development. New research on the importance of specific nutrients in promoting growth and development of infants and long-term health of adults is prompting scientists to consider the potential importance of these nutrients for toddlers as well.
Toddlers’ eating patterns and behaviors prompt concern about the nutritional adequacy of their diets. The toddler years are characterized by a transition from a predominantly defined, nutrient dense, liquid diet of breast milk or infant formula to a diet consisting primarily of table foods provided by 3 meals and snacks daily.
1 Toddlers’ diets may become less dense in some nutrients as they transition from an infant diet to a diet of solid foods.
1 Toddlers are also developing the motor skills required to feed themselves and this may influence nutrient intake.
2 Toddlers are often described as having food
“neophobia.” That is, they express dislike or reject foods that are new because they are unfamiliar. Young children often require repeated exposure to a food before accepting it.
3 Many parents consider their toddlers to be picky eaters, and this increases as toddlers age. Carruth and colleagues reported that 35% of caregivers of 12- to 14-month-olds considered their
WHAT IS A TODDLER?
The term toddler comes from the wide-based, unsteady, toddling gait of a child learning to walk.
Pediatric medicine has no official definition of toddlers but toddlerhood is generally thought to begin at 12 months of age and can include preschoolers up to 5 years of age.
toddlers to be picky eaters. For caregivers of toddlers ages 19 to 24 months, the percentage was 50%.
4 Neophobia and the perception of having a picky eater may influence the nutritional quality of the diets offered to and consumed by toddlers.
Despite the potential importance of toddler nutrition and characteristics of toddlers’ eating patterns and behaviors, the nutritional needs of toddlers have not been well studied. Breast milk and breastfed babies are the standards for infant nutrition; and, using these standards, the nutritional needs of infants have been fairly well defined as infant formulas have been developed and studied. National surveys in the U.S. have evaluated the nutritional status and nutritional intakes of older children and adults for many years. In contrast, relatively few toddlers are included in these surveys. Moreover, there are few data on physiological nutrient requirements of young children and potentially adverse or beneficial effects of increased nutrient intakes by young children.
5 In addition, little is known about the physical activity patterns of young children and how activity affects nutrient requirements and growth. Few nutritional status indicators have been identified that are specific to this age group. Consequently, the nutritional needs of toddlers are less well defined.
I N T R O D U C T I O N
The potential impact of inappropriate toddler nutrition and the relative paucity of data on toddlers prompted
Mead Johnson Nutritionals to gather a group of pediatric nutrition experts to discuss 4 areas of nutrition for healthy toddlers in the U.S.: energy, macronutrient and micronutrient intakes, metabolic programming, overweight status and risk, and docosahexaenoic acid (DHA) nutrition. This monograph summarizes their presentations and includes additional data and positions published since the panel’s discussion. The goal of the monograph is to raise awareness of toddler nutrition issues and the importance of food patterns and nutrient intakes for healthy toddlers among pediatric health care professionals.
I N T R O D U C T I O N 7
Nutrient Intakes of Toddlers vs Recommendations
Contributors:
Robert Baker, MD, PhD
Professor of Pediatrics
State University of New York at Buffalo
Co-Chief, Digestive Disease and Nutrition Center
Women and Children’s Hospital of Buffalo
Benjamin H. Caballero, MD, PhD
Professor of Pediatrics, International Health and Maternal and Child Health
Director, Center for Human Nutrition, Bloomberg School of Public Health
Johns Hopkins University
Bonny Specker, PhD
Professor, Nutrition, Food Science and Hospitality
Chair & Director, Ethel Austin Martin Program in Human Nutrition
South Dakota State University
8 N U T R I E N T I N TA K E S O F T O D D L E R S V S R E C O M M E N D AT I O N S
Medical and drug information is constantly evolving because of ongoing research and clinical experience that are often subject to interpretation. While care has been taken to ensure the accuracy of the information presented, the reader is advised that Mead Johnson & Company, and the authors, editors, reviewers, contributors, and publishers of this material are not responsible for the continued currency of the information contained in this material, or any errors or omissions that might appear in this material, or for any consequences arising out of, or resulting from, the use of the material for any purpose or reason whatsoever.
Because of the dynamic nature of medical and drug information, readers are advised that decisions regarding drug or any other therapy must be based on the independent judgment of the clinician, information about a drug (eg, as reflected in the literature), and changing medical practices.
The Editors and Mead Johnson & Company
N U T R I E N T I N TA K E S O F T O D D L E R S V S R E C O M M E N D AT I O N S 9
RECOMMENDED INTAKES
Between 1941 and 1989, the Food and Nutrition Board of the Institute of Medicine prepared the Recommended
Dietary Allowances to provide “standards to serve as a goal for good nutrition.” 6 In 1997, the Institute of Medicine published the first in a set of Dietary Reference Intakes (DRI), which replace the previous Recommended Dietary
Allowances.
7 According to Yates et al., “DRIs are reference values that are quantitative estimates of nutrient intakes to be used for planning and assessing diets for healthy people.” 8 DRI have been established for energy and the macronutrients that provide energy (carbohydrate, protein and fat) 9 as well as micronutrients (vitamins and minerals).
7, 10-12 The DRI include Estimated Average Requirements (EAR), Recommended Dietary Allowances
(RDA), Adequate Intakes (AI), and the Tolerable Upper Intake Levels (UL).
9 For nutrients that yield calories,
Acceptable Macronutrient Distribution Ranges (AMDR) were also established.
9 Estimated Energy Requirements
(EER) are used for determining energy needs.
9 Table 1 defines terms associated with the DRI.
8, 9
Table 1. Definitions of Terms Associated With the Dietary Reference Intakes
8,9
Estimated Average Requirement (EAR): The average daily nutrient intake level estimated to meet the requirements of half the healthy individuals in a particular life stage and gender group. The
EAR is used to develop the RDA.
Recommended Dietary Allowance (RDA): The average daily dietary nutrient intake level sufficient to meet the nutrient requirements of nearly all (97% to 98%) healthy individuals in a particular life stage or gender group. RDA can also be used as intake goals for individuals.
Adequate Intake (AI): The recommended average daily intake level based on observed or experimentally determined approximations of nutrient intake by a group (or groups) of apparently healthy people that are assumed to be adequate—used when an RDA cannot be determined. AI can also be used as intake goals for individuals.
Tolerable Upper Intake Level (UL): The highest average daily nutrient intake level that is likely to pose no risk of adverse health effects to almost all individuals in the general population. As intake increases above the UL, the potential risk of adverse effects may increase.
Acceptable Macronutrient Distribution Range (AMDR): Ranges of macronutrient intakes (as a percentage of calories) that are associated with reduced risk of chronic disease while providing recommended intakes of other essential nutrients. Little data on the consequences of exceeding
AMDR in young children exist, however.
Estimated Energy Requirement (EER): The average dietary energy intake that is predicted to maintain energy balance in a healthy adult of a defined age, gender, weight, height and level of physical activity, consistent with good health. In children, the EER is taken to include the needs associated with the deposition of tissues consistent with good health.
Limitations of the data on toddler nutrition made defining toddlers’ nutrient requirements extremely challenging. For most nutrients there are no data on toddlers’ physiological requirements resulting from direct assessment. Most nutrient intake recommendations for toddlers come from observations of intake. In addition, there are few nutritional status indicators specific for this age group. It is not clear if nutritional status indicators used for older children and adults are valid for toddlers. There are little data on the adverse or beneficial effects of high nutrient intakes in children. Finally, there are few data on physical activity patterns of young children and how they affect nutrient requirements and growth. Despite the limitations, the DRI are the best standards available based on current evidence for evaluating toddlers’ macronutrient and micronutrient intakes.
MACRONUTRIENTS
In 2002, DRI were established for energy, carbohydrate, protein, and fat.
9 Data indicate that young children consume more energy than estimated requirements, and intakes meet recommendations for carbohydrate and protein. Fiber intakes, however, rarely meet recommendations.
Total Energy
Calculations for estimated energy requirements (EER) for young children were based on research in which energy needs were determined using the doubly labeled water method. This method is more accurate than factorial methods and measurements of basal metabolic rate used for making past energy estimates. The doubly labeled water method allows measurement of energy output under normal everyday conditions; it represents patterns of energy expenditure over several days; it reflects differences in basal metabolic rate during awake and sleep states; and it includes the energy cost of all physical activities.
EER for children equals total energy expenditure plus energy deposition. Total energy expenditure is influenced by age, sex, height, weight, and physical activity level and these variables are included in the calculations. The energy deposition value is an estimate of the amount of daily energy required for growth.
9 The new equations are provided in Table 2.
9
Table 2. Equations for Estimating Energy Requirements
9
Children 13 to 35 months (boys and girls)
EER = (89 x weight in kg-100) + 20 [the estimated kcal needed for energy deposition]
Boys 3 through 8 years
EER = 88.5-61.9 x age in years + physical activity level x (26.7 x wt in kg + 903 x ht in m) + 20 [the estimated kcal needed for energy deposition]
Physical activity levels: 1.00 for sedentary; 1.13 for low active; 1.26 for active; 1.42 for very active
Girls 3 through 8 years
EER = 135.3-30.8 x age in years + physical activity level x (10.0 x wt in kg + 934 x ht in m) + 20 [the estimated kcal needed for energy deposition]
Physical activity levels: 1.00 for sedentary; 1.16 for low active; 1.31 for active; 1.56 for very active
N U T R I E N T I N TA K E S O F T O D D L E R S V S R E C O M M E N D AT I O N S 11 10 N U T R I E N T I N TA K E S O F T O D D L E R S V S R E C O M M E N D AT I O N S
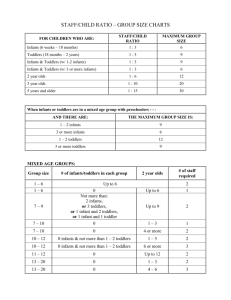
As part of the Feeding Infants and Toddlers Study, Devaney and colleagues evaluated energy intakes of toddlers ages 12 to 24 months.
13 They found that usual energy intakes exceed EER for children in all percentiles of usual intake (Figure 1). Average intake was 1249 kilocalories per day while average EER was 950 kilocalories per day.
13 In general this is consistent with other surveys that indicate that children consume more than estimated requirements.
9
Figure 1. Energy Intakes and Estimated Energy Requirements of 1- to 2-Year-Old Toddlers
(adapted from
7
)
Fat
Table 3. Acceptable Macronutrient Distribution Ranges for Fat
9
1 to 3 years: 30% to 40% of energy from fat
4 to 18 years: 25% to 35% of energy from fat
The DRI committee did not establish an EAR, RDA, AI, or UL for total fat for children 9 because there was insufficient evidence for defining a total fat intake in childhood that would support growth while decreasing the risk of obesity, diabetes, or coronary heart disease. The committee did, however, establish AMDR for fat. The higher range for fat for children ages 1 to 3 years reflects the transition from a diet primarily consisting of breast milk and/or infant formula, both which provide about 50% of calories from fat, to a diet primarily consisting of solid foods. The lower range for children over the age of 3 years is similar to recommendations for adults.
Devaney et al. reported that 29% of toddlers between the ages of 1 and 2 years had fat intakes less than 30% of calories and 9% had fat intakes exceeding 40% of calories.
13 Although reduced fat intakes have been linked to lower intakes of certain micronutrients in other studies, 14 intakes of most micronutrients in the Feeding Infants and Toddlers Study were adequate.
13
12 N U T R I E N T I N TA K E S O F T O D D L E R S V S R E C O M M E N D AT I O N S
Table 4. Recommended Intakes (AI) and Acceptable Macronutrient Distribution
Ranges for n-6 and n-3 Fatty Acids
9
Linoleic acid and n-6 fatty acids
AI : 7 to 10 g/day of linoleic acid
AMDR for n-6 fatty acids: 5% to 10% of total energy
α -Linolenic acid and n-3 fatty acids
AI: 0.7 to 0.9 g/day of α -linolenic acid (includes small amounts of eicosapentaenoic acid [EPA] and docosahexaenoic acid [DHA])
AMDR for α -linolenic acid: 0.6% to 1.2% of total energy. Up to 10% of this can come from EPA and DHA.
Recommended adequate intakes (AI) for the essential fatty acids, linoleic acid (C18:2n-6; an 18 carbon, 2-double bond, n-6 fatty acid), and α -linolenic acid (C18:3n-3; an 18-carbon, 3-double bond, n-3 fatty acid) were established
(Table 4). AMDR were also established for n-6 and n-3 fatty acids.
9
Carbohydrate
Table 5. Recommended Intakes (RDA or AI) and Acceptable Macronutrient Distribution
Ranges for Carbohydrate, Fiber, and Added Sugars
9
Carbohydrate
Fiber
Added Sugars
1- to 3-year-olds
130 g/day
~19 g/day
Not determined
4- to 8-year-olds
130 g/day
~25 g/day
Not determined
45% to 65% of energy
Not determined
25% of energy*
*AMDR for added sugars not determined. Value is maximal intake level.
Total Carbohydrate
The recommended intake (RDA) for total carbohydrate by young children is 130 grams per day 9 and is the same as the RDA for adults, which was based on a carbohydrate intake that was associated with blood ketone levels that were no higher than ketone levels after an overnight fast. No UL for carbohydrate was established because there was no definitive evidence that a high carbohydrate diet leads to obesity, diabetes, or coronary heart disease in children. Data indicate that toddlers’ intakes meet the RDA for carbohydrate. Devaney and colleagues found that average carbohydrate intake of 1- to 2-year-olds was 165 g/day.
13 The USDA Continuing Survey of Food Intakes by
Individuals 1994-96, 1998 (CSFII) found that the average carbohydrate intakes of 1- to 2-year-olds and 3- to 5-yearolds were 179 g/day and 227 g/day, respectively.
15
N U T R I E N T I N TA K E S O F T O D D L E R S V S R E C O M M E N D AT I O N S 13
Definitions of Fiber were established in 2000
16
:
Dietary fiber: fiber naturally present in foods of plant origin, such as cellulose and the fibers in oat and wheat bran.
Functional fiber: fiber that has been isolated, extracted, or synthesized and has proven beneficial effects in humans, such as resistant starch.
Total fiber: the sum of dietary fiber and functional fiber.
Fiber
Recommendations (AI) for total fiber intakes for children were established at 14 grams of fiber/1000 kilocalories.
9 The Feeding
Infants and Toddlers Study, however, found that average fiber intake of toddlers between the ages of 1 and 2 years was below the recommendation and was 8 g/day.
13 Children in the 90th percentile of fiber consumption consumed 12 g/day. In the USDA
Continuing Survey of Food Intakes by Individuals 1994-96, 1998
(CSFII), 1- to 2-year-old children consumed 9 grams of fiber daily and 3-to 5-year-old children consumed 11 grams.
15
Added Sugars
Added sugars are a potential nutritional concern because high intakes may dilute the nutrient density of children’s diets. A maximal intake level for added sugars was suggested at no more than 25% of energy.
9
“Added sugars are defined as sugars and syrups that are added to foods during processing or preparation.”
Examples of added sugars include white sugar, raw sugar, corn syrup, high-fructose corn syrup, malt syrup, honey and molasses.
13
Protein
Table 6. Recommended Intakes (RDA) and Acceptable Macronutrient Distribution
Ranges for Protein
13
1- to 3-year-olds
4- to 8-year-olds
RDA
1.10 g/kg/day (~13 g/day)
0.95 g/kg/day (~19 g/day)
AMDR
5% to 20% of energy
10% to 30% of energy
The 2002 DRI protein intake recommendations decreased slightly from the 1989 RDA.
6, 13 Protein intake recommendations were based on data indicating nitrogen intakes required for maintenance, replacement of losses and growth. No UL was established for protein because there was insufficient evidence of adverse health effects from humans consuming high levels. Dietary intakes of protein by young children typically exceed estimated needs.
MICRONUTRIENTS
Nutrient intake data indicate that toddlers between the ages of 1 and 5 get recommended amounts of most micronutrients (Tables 7 and 8).
7, 10-13, 15 Despite data indicating that young children are consuming recommended intakes for most micronutrients, iron deserves continued attention since iron deficiency in the first years of life is relatively common and may have irreversible negative consequences on development.
17 In addition, calcium and vitamin D are critical for bone health and peak bone mass and should receive continued emphasis. Nutrient intake data indicate that vitamin E intakes by young children are low and should be considered. Possible over consumption of some micronutrients may be an issue for some young children.
14 N U T R I E N T I N TA K E S O F T O D D L E R S V S R E C O M M E N D AT I O N S
Table 7. Recommended Nutrient Intakes vs Average Nutrient Intakes for Children
1 to 3 Years of Age
7,10-13,15,18
Nutrient
RDA/AI Average intakes, Average intakes, Average intakes, UL, 1-to
1- to 31- to 21- to 2year-olds year-olds, FITS year-olds, CSFII
3-year-olds,
CSFII
3-yearolds
Vitamin A, mcg RE
Vitamin D, mcg
Vitamin E, mg TE
Vitamin C, mg
Thiamin, mg
Riboflavin, mg
Niacin, mg
Vitamin B-6, mg
Folate, mcg
Vitamin B-12, mcg
300
5
6
15
0.5
0.5
6
0.5
150
0.9
694
8.7
5
91
1.2
13
1.8
318
1.3
3.7
739
6.0
(1- to 3-year-olds)
4.8
782
5.4
103
1.13
1.71
12.8
106
1.32
1.82
15.5
198
1.3
3.2
263
1.47
3.54
600
50
*200
400
ND
ND
*10
30
*300
ND
Calcium, mg
Phosphorus, mg
Magnesium, mg
Iron, mg
Zinc, mg
Copper, mg
Selenium, mcg
500
460
80
7
3
0.34
20
939
968
184
9.8
6.9
Not reported
Not reported
854
966
187
10.8
7.4
0.7
59.8
843
1034
201
12.3
8.5
0.8
68.9
Values in bold type are RDA.
*UL for vitamin E, niacin, and folate apply to synthetic forms obtained from supplements, fortified foods, or a combination of the two. UL for magnesium represents intake from a pharmacological agent only and does not include intake from food or water.
ND=not determined.
2500
3000
*65
40
7
1
90
Iron
The prevalence of iron deficiency in toddlers ages 1 to 2 years in the United States has decreased in the past decade from 9% to 7%.
19 For children ages 3 to 5 years, however, iron deficiency increased from 3% to 5%.
19 The most severe form of iron deficiency, iron deficiency anemia, occurs in about 2% of 1- to 2-year-olds in the U.S.
19
Infants and toddlers are at greater risk of iron deficiency in the first two years of life than older and preadolescent children due to rapid growth.
20 Children in households with inadequate financial resources were more likely to have iron deficiency anemia.
21 In a study involving 12–36 month old children from WIC clinics in
California, Schneider et al., noted a prevalence of iron deficiency and anemia in the population.
22 Females in this study population demonstrated lower iron stores than boys. Early iron deficiency can adversely affect mental and motor development and behavior, 23-25 and some effects are not reversible with iron therapy, persisting several years after the deficiency is corrected.
17
Toddlers who may be at greatest risk of iron deficiency include those who were born with low iron stores due to prematurity, who experienced intrauterine growth retardation, or who had a mother with gestational diabetes.
20
Toddlers who did not receive adequate dietary iron in the first year of life are also at greater risk. Inadequate iron intakes during infancy can result from feeding low iron infant formula, feeding milk (cow, goat and/or soy)
N U T R I E N T I N TA K E S O F T O D D L E R S V S R E C O M M E N D AT I O N S 15
Table 8. Recommended Nutrient Intakes vs Average Nutrient Intakes for Children
4 and 5 Years of Age
7,10-12,15
Nutrient
Vitamin A, mcg RE
Vitamin D, mcg
Vitamin E, mg TE
Vitamin C, mg
Thiamin, mg
Riboflavin, mg
Niacin, mg
Vitamin B-6, mg
Folate, mcg
Vitamin B-12, mcg
RDA/AI,
4- to 8year-olds
400
5
7
25
0.6
0.6
8
0.6
200
1.2
Average intakes,
Average intakes,
4-year-olds, CSFII 5-year-olds, CSFII
834
Not reported
5.9
106
1.42
1.9
17
283
1.54
3.73
832
Not reported
6.3
99
1.47
1.97
18.1
279
1.61
3.84
UL,
4- to 8year-olds
900
50
*300
650
ND
ND
*15
40
*400
ND
Calcium, mg
Phosphorus, mg
Magnesium, mg
Iron, mg
Zinc, mg
Copper, mg
Selenium, mcg
800
500
130
10
5
0.44
30
864
1085
212
13.4
9.3
0.9
75.1
887
1136
222
13.9
9.7
0.9
80.7
Values in bold type are RDA.
*UL for vitamin E, niacin, and folate apply to synthetic forms obtained from supplements, fortified foods, or a combination of the two. UL for magnesium represents intake from a pharmacological agent only and does not include intake from food or water.
ND=not determined.
2500
3000
*110
40
12
3
150 instead of breast milk or iron fortified infant formula, and not providing supplemental iron source to a breastfed infant.
20 Data also indicate that iron density of the diet decreases as toddlers transition away from an infant diet.
1
Toddlers who do not consume iron from meat or other food sources may also be at risk.
The American Academy of Pediatrics (AAP) recommends several steps for preventing iron deficiency.
20 Infants should be breastfed and breastfed infants should receive a supplemental iron source by 4 to 6 months of age.
If infants receive infant formula as a supplement to or in place of breast milk, only iron-fortified formula should be used during the first 12 months of life. Milk (cow, goat, soy) should not be introduced before 12 months of age.
Iron-rich foods, such as iron fortified cereal and meats should be introduced at weaning.
20 Physicians should screen infants and toddlers at risk of developing iron deficiency by measuring hemoglobin or hematocrit levels between 9 and 12 months of age, and 6 months later at 15 to 18 months of age.
20 The AAP recommends that children ages 1 to 5 years should avoid consuming more than 24 ounces of milk per day because large amounts of milk may displace iron-rich foods in the diet.
20
Calcium and Vitamin D
Little data on the calcium requirements of toddlers and young children exist. Lack of data prevented the DRI committee from setting an RDA for calcium. Only AI have been established for this nutrient. The AI for calcium
16 N U T R I E N T I N TA K E S O F T O D D L E R S V S R E C O M M E N D AT I O N S for children ages 1 through 3 is 500 mg per day, and for children ages 4 through 8 is 800 mg per day.
7 The optimal calcium intake for young children, however, has not been determined.
Nutrient intake data indicate that average calcium intakes by 1- to 3-year-old toddlers exceed the AI of
500 mg per day. Reported average calcium intakes were 939 mg 13 and 854 mg per day for 1- to 2-year-olds 15 and 843 mg per day for 3-year-olds.
15 Intake data indicate that average calcium consumption by 4- and 5-year-old children exceeds the AI of 800 mg per day, with 864 mg per day consumed by 4-year-olds, and 887 mg per day consumed by 5-year-olds.
15
Lack of data also prevented the DRI committee from establishing an RDA for vitamin D for children 1 to 8 years of age. The AI for toddlers 1 to 3 years and children ages 4 to 8 years is 5 mcg (200 IU) per day.
7
The Feeding Infants and Toddlers Study evaluated vitamin D intakes by 1- to 2-year-old toddlers and reported average intakes of 8.7 mcg (348 IU) per day.
13 Moore and colleagues summarized vitamin D data from CSF II and
NHANES III and report intakes of 6.0 and 5.7 mcg/d for children 1 to 3 years of age, respectively.
18 Data from both studies indicate that approximately 50%–60% of this age group is meeting the adequate intake level (5 mcg/day) established for vitamin D.
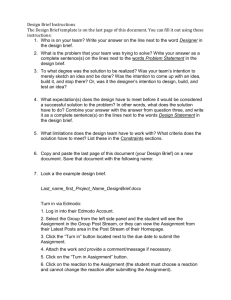
Specker and colleagues conducted a preliminary analysis of calcium and vitamin D intakes of 5449 1- to 5-year-old children in NHANES III. The unpublished results were based on raw data and did not take into account the sampling scheme used by NHANES III (Figure 2). They found that among children 1 to 5 years of age, the lowest calcium intakes (747 mg/day) were by toddlers ages 24 to 35 months. Children 36 to 47 months had an average calcium intake of 768 mg per day, while children 48 to 60 months had an average intake of 803 mg per day. About 50% of the children in these older age groups, however, had calcium intakes below the AI of 800 mg.
Average vitamin D intakes were lowest for toddlers ages 24 to 35 months (5.31 mcg/day). About 50% of children ages 24 to 60 months had vitamin D intakes less than the AI of 5 mcg per day, which is in agreement with Moore and colleagues findings for 1- to 3-year-olds.
18
In their evaluation of NHANES III data, Specker and colleagues noted sex, regional, and ethnic differences in calcium and vitamin D intakes: females have lower intakes than males; toddlers in the South have lower intakes than toddlers in other regions; and, non-Hispanic blacks have lower intakes than other ethnic groups. Fulgoni and colleagues reported calcium intakes for 0- to 3-year-olds were significantly lower in African-American children than in children of other races (CSFII: Female: 614 vs 818*; Male: 724 vs 869*; NHANES [1999-2000]: Female 682 vs
809; Male: 756 vs 981*; * P <0.05).
26
Low intake of milk, which serves as a source of calcium and vitamin D in the diet, in childhood and adolescence was associated with a decrease in bone mineral content and density, as well as an increased risk of fracture in women.
27 NHANES III data on children and adolescents aged 8 to 18 years indicate that a higher intake of lownutrient dense foods is related to a lower intake of several micronutrients, including calcium.
28 Greer et al., in the recent AAP position on calcium, provide a summary of data sets regarding calcium intakes and demonstrate that, with an increase in age, the percentage of children and adolescents achieving the recommended intakes of calcium decreases from approximately 93% at less than a year of age to 30% between the ages of 12 and 19.
29
N U T R I E N T I N TA K E S O F T O D D L E R S V S R E C O M M E N D AT I O N S 17
Figure 2. NHANES III Preliminary Results. Calcium (upper panel) and Vitamin D (lower panel)
Intake by Age (Specker et al., unpublished)
Vitamin D fortified liquid milk is a primary source of calcium and vitamin D in toddlers’ diets, and as milk intakes decrease, dietary intakes of calcium and vitamin D decrease. Skinner and colleagues reported that 100% juice, fruit drinks, and carbonated beverages may displace milk in the diets of 1- to 2-year-old toddlers leading to diets with lower calcium density.
30 In addition, toddlers who consume more energy from table food consume less milk leading to lower calcium intakes.
31
18 N U T R I E N T I N TA K E S O F T O D D L E R S V S R E C O M M E N D AT I O N S
These observations, along with research reporting that milk intakes decrease as other beverages and table foods are added to the diet, indicate that appropriate calcium and vitamin D intakes should receive continued emphasis. The establishment of dietary practices ensuring adequate calcium intake is important in childhood.
29
Adequate calcium intake during childhood and adolescence contributes to the attainment of peak bone mass, an important factor in reducing the risk of skeletal disorders such as fractures and osteoporosis.
29
Vitamin E
Vitamin E functions as an antioxidant and helps protect cells from free radical damage and is needed for normal cellular structure and function. The Feeding Infants and Toddlers Study reported that 58% of toddlers ages 12 to
24 months had vitamin E intakes less than the estimated average requirement of 5 mg per day.
13 Data from the
USDA Continuing Survey of Food Intakes by Individuals 1994-96, 1998 also indicate that vitamin E intakes for children ages 1 to 5 years are lower than recommended levels (Tables 7 and 8).
15 Researchers with Feeding Infants and Toddlers Study requested readers to interpret vitamin E findings with caution.
13 Vitamin E intake recommendations (DRI) for children over 1 year were extrapolated from adult values and may be imprecise.
13 In addition, it is difficult to assess vitamin E added to foods through fats and cooking oils, and there is variability in reported vitamin E content of foods among food composition databases.
13
OVER CONSUMPTION OF MICRONUTRIENTS
Nutrient intake data indicate that 1- to 2-year-old toddlers may have vitamin A and zinc intakes above the UL of
600 mcg per day and 7 mg per day, respectively.
13, 15 Average vitamin A intake by 1- to 2-year-old toddlers in the
Feeding Infants and Toddlers study was 694 mcg per day with 35% of the toddlers having vitamin A intakes above the UL.
13 The USDA Continuing Survey of Food Intakes by Individuals 1994-96, 1998 (CSFII) data indicate that 1- to
2-year-olds consumed an average of 739 mcg per day and 3-year-olds consumed an average of 782 mcg per day.
15
Devaney and colleagues pointed out that there is a narrow margin between the RDA for vitamin A and the UL.
13
They concluded that there is a need to avoid unnecessary vitamin A supplementation, and there is also a need for better data to use for setting UL for young children.
13 In the Feeding Infants and Toddlers study, 43% of the toddlers had zinc intakes above the UL of 7 mg/day.
13 Average zinc intakes of children ages 1 to 3 ranged from 6.9
mg 13 to 8.5 mg per day.
15 Devaney and colleagues concluded that the UL for zinc needs further substantiation since it was based on one study of full-term infants who received infant formula that provided about 4.5 mg zinc per day.
13 No adverse effects on copper status due to zinc intakes were documented in that study. Despite the lack of adverse effects, the study was used to determine the UL.
Intakes of niacin and magnesium by children 1 to 5 years of age may appear to be above the UL for these nutrients.
13,15 The UL for niacin, however, is specific to synthetic forms found in supplements and fortified foods.
10
Food composition databases do not distinguish between naturally occurring niacin and synthetic forms added to foods.
13 Therefore, Devaney and colleagues could not determine the percentage of children who exceed the UL for synthetic niacin.
13 The UL for magnesium is specific to supplements and pharmacological agents and does not include magnesium in food or water.
7
N U T R I E N T I N TA K E S O F T O D D L E R S V S R E C O M M E N D AT I O N S 19
REFERENCES
1.
Skinner JD, Ziegler P, Pac S, et al. Meal and snack patterns of infants and toddlers.
J Am Diet Assoc.
2004;104(suppl):
S65-S70.
2.
Carruth BR, Ziegler PJ, Gordon A, et al. Developmental milestones and self-feeding behaviors in infants and toddlers.
J Am Diet Assoc.
2004;104(suppl):S51-S56.
3.
Birch LL, McPhee L, Shoba BC, et al. What kind of exposure reduces children's food neophobia? Looking vs tasting.
Appetite.
1987;9:171-178.
4.
Carruth BR, Ziegler PJ, Gordon A, et al. Prevalence of picky eaters among infants and toddlers and their caregivers' decisions about offering a new food.
J Am Diet Assoc.
2004;104(suppl):S57-S64.
5.
Ong KK, Loos RJ. Rapid infancy weight gain and subsequent obesity: systematic reviews and hopeful suggestions.
Acta Paediatr.
2006;95:904-908.
6.
Institute of Medicine.
Recommended Dietary Allowances.
10th Edition. Washington, D.C.: National Academy Press; 1989.
7.
Institute of Medicine.
Dietary Reference Intakes for Calcium, Phosphorus, Magnesium, Vitamin D, and Fluoride.
Washington, D.C.: National Academy Press; 1997.
8.
Yates AA, Schlicker SA, Suitor CW. Dietary Reference Intakes: the new basis for recommendations for calcium and related nutrients, B vitamins, and choline.
J Am Diet Assoc.
1998;98:699-706.
9.
Institute of Medicine.
Dietary Reference Intakes for Energy, Carbohydrate, Fiber, Fat, Fatty Acids, Cholesterol, Protein, and
Amino Acids.
Washington, D.C.: National Academy Press; 2002.
10. Institute of Medicine.
Dietary Reference Intakes for Thiamin, Riboflavin, Niacin, Vitamin B6, Folate, Vitamin B12,
Pantothenic Acid, Biotin, and Choline.
Washington, D.C.: National Academy Press; 2000.
11.
Institute of Medicine.
Dietary Reference Intakes for Vitamin C, Vitamin E, Selenium, and Carotenoids.
Washington, D.C.:
National Academy Press; 2000.
12. Institute of Medicine.
Dietary Reference Intakes for Vitamin A, Vitamin K, Arsenic, Boron, Chromium, Copper, Iodine, Iron,
Manganese, Molybdenum, Nickel, Silicon, Vanadium, and Zinc.
Washington, D.C.: National Academy Press; 2001.
13.
Devaney B, Ziegler P, Pac S, et al. Nutrient intakes of infants and toddlers.
J Am Diet Assoc.
2004;104(suppl):S14-S21.
14. Nicklas TA, Webber LS, Koschak M, et al. Nutrient adequacy of low fat intakes for children: the Bogalusa Heart Study.
Pediatrics.
1992;89:221-228.
15. U.S. Department of Agriculture, Agricultural Research Service.
Food and Nutrient Intakes by Children.
1994-96, 1998. 1999.
Available at: http:www.barc.usda.gov/bhnrc/foodsurvey/home.htm. Accessed March 1, 2004.
16. Institute of Medicine.
Dietary Reference Intakes Proposed Definition of Dietary Fiber.
Washington, D.C.: National Academy
Press; 2001.
17.
Lozoff B, Jimenez E, Hagen J, et al. Poorer behavioral and developmental outcome more than 10 years after treatment for iron deficiency in infancy.
Pediatrics.
2000;105:E51.
18. Moore C, Murphy MM, Keast DR, et al. Vitamin D intake in the United States.
J Am Diet Assoc.
2004;104:980-983.
19. Looker AC, Cogswell ME, Gunter EW. Iron Deficiency–United States, 1999-2002.
MMWR.
2002;51:897-899.
20. Iron Deficiency. In: Kleinman R, ed.
Pediatric Nutrition Handbook.
5th ed: American Academy of Pediatrics. 2004:299-312.
21. Skalicky A, Meyers AF, Adams WG, et al. Child Food Insecurity and Iron-Deficiency Anemia in Low-Income Infants and
Toddlers in the United States.
Matern Child Health J.
2006;10:177-185.
22. Schneider JM, Fujii ML, Lamp CL, et al. Anemia, iron deficiency, and iron deficiency anemia in 12-36-mo-old children from low-income families.
Am J Clin Nutr.
2005;82:1269-1275.
23. Lozoff B, Klein NK, Nelson EC, et al. Behavior of infants with iron-deficiency anemia.
Child Dev.
1998;69:24-36.
24. Walter T, Kovalskys J, Stekel A. Effect of mild iron deficiency on infant mental development scores.
J Pediatr.
1983;102:
519-522.
25. Walter T, De Andraca I, Chadud P, et al. Iron deficiency anemia: adverse effects on infant psychomotor development.
Pediatrics.
1989;84:7-17.
26. Fulgoni V III, Nicholls J, Reed A, et al. Dairy consumption and related nutrient intake in African-American adults and children in the United States: continuing survey of food intakes by individuals 1994-1996, 1998, and the National Health and Nutrition Examination Survey 1999-2000.
J Am Diet Assoc.
2007;107:256-264.
27. Kalkwarf HJ, Khoury JC, Lanphear BP. Milk intake during childhood and adolescence, adult bone density, and osteoporotic fractures in US women.
Am J Clin Nutr.
2003;77:257-265.
28. Kant AK. Reported consumption of low-nutrient-density foods by American children and adolescents: nutritional and health correlates, NHANES III, 1988 to 1994.
Arch Pediatr Adolesc Med.
2003;157:789-796.
29. Greer FR, Krebs NF, Committee on Nutrition. Optimizing bone health and calcium intakes of infants, children, and adolescents.
Pediatrics.
2006;117:578-585.
30. Skinner JD, Ziegler P, Ponza M. Transitions in infants' and toddlers' beverage patterns.
J Am Diet Assoc.
2004;104:S45-S50.
31.
Briefel RR, Reidy K, Karwe V, et al. Toddlers' transition to table foods: Impact on nutrient intakes and food patterns.
J Am Diet Assoc.
2004;104(suppl):S38-S44.
20 N U T R I E N T I N TA K E S O F T O D D L E R S V S R E C O M M E N D AT I O N S N U T R I E N T I N TA K E S O F T O D D L E R S V S R E C O M M E N D AT I O N S 21
Metabolic Programming
Contributor:
Rebecca Simmons, MD
Professor of Pediatrics
Center for Research on Reproduction and Women’s Health
Children’s Hospital of Philadelphia
University of Pennsylvania Medical Center
22 M E TA B O L I C P R O G R A M M I N G
Medical and drug information is constantly evolving because of ongoing research and clinical experience that are often subject to interpretation. While care has been taken to ensure the accuracy of the information presented, the reader is advised that Mead Johnson & Company, and the authors, editors, reviewers, contributors, and publishers of this material are not responsible for the continued currency of the information contained in this material, or any errors or omissions that might appear in this material, or for any consequences arising out of, or resulting from, the use of the material for any purpose or reason whatsoever.
Because of the dynamic nature of medical and drug information, readers are advised that decisions regarding drug or any other therapy must be based on the independent judgment of the clinician, information about a drug (eg, as reflected in the literature), and changing medical practices.
The Editors and Mead Johnson & Company
M E TA B O L I C P R O G R A M M I N G 23
In 1990, Barker proposed that “the womb may be more important than the home.” 1 The period from conception to birth is a time of rapid growth, cellular replication and differentiation, and functional maturation of organ systems. These processes are very sensitive to alterations in the intrauterine milieu. Programming describes the mechanisms whereby a stimulus or insult at a critical period of development has lasting or lifelong effects. It has been recognized for nearly 70 years that the environment in which a child grows and develops could have longterm effects on subsequent health and survival. Multiple epidemiology studies have linked low birth weight to the later development of a number of adult diseases, including hypertension, coronary artery disease, stroke, diabetes, kidney disease, and breast cancer. Although there are little data on the effects of toddler nutrition on later health, the toddler years are characterized by continued physiological development. Experts now suggest that this hypothesis be expanded to include evaluation of the early years of childhood.
THE INTRAUTERINE ENVIRONMENT
An abnormal intrauterine environment due to placental insufficiency or metabolic conditions of the mother, such as diabetes mellitus, appears to increase the risk of obesity and type 2 diabetes in her offspring. Placental insufficiency results in decreased levels of energy, nutrients, hormones and growth factors supplied to the fetus via the placenta, while diabetes mellitus results in increased levels. Experts hypothesize that both scenarios cause changes in gene expression, structure, and/or function of rapidly developing fetal cells with the alterations contributing to health consequences in later childhood and adulthood.
BIRTH WEIGHT
Birth weight may reflect conditions in the intrauterine environment. Placental insufficiency results in an infant with growth retardation while maternal diabetes often results in a large for gestational age neonate. Low birth weight due to small for gestational status at birth (rather than appropriately sized preterm infants) is linked to increased risk for developing obesity and type 2 diabetes.
The Dutch famine study reported by Ravelli and colleagues in 1976 suggested long-term implications of an altered intrauterine environment and resulting low birth weight.
2 The Dutch famine occurred in the western
Netherlands from October 1944 until May 1945. During this time, daily food rations provided as little as 580 kilocalories per day. Ravelli et al. reported on their evaluation of 94,800 19-year-old men who had been exposed to the famine in utero or early infancy. Infants who had been exposed to the famine in utero frequently had fetal growth retardation and abnormally low birth weight. At 19 years of age, men who had been exposed to the famine in utero during the first 2 trimesters of pregnancy had significantly higher rates of obesity than men in the eastern Netherlands who were not exposed to the famine. The researchers speculated that early nutritional deprivation affected the differentiation of hypothalamic centers that regulated food intake and growth.
2 In later studies, lighter birth weight was linked to the development of type 2 diabetes in adult men 3 and women, 4 Pima
Indian children, 5 Taiwanese children, 6 and both monozygotic and dizygotic twins.
7
While lighter birth weight appears to increase the risk of obesity and type 2 diabetes, very high birth weights may also increase risk. A study of Pima Indians found that infants with lower birth weights (<2.5 kg) and those with high birth weights (>4.5 kg) had higher prevalence of diabetes at ages 10 to 14 and 15 to 19 years.
5 Wei and colleagues 6 also reported a “U-shaped” relationship between birth weight and development of type 2 diabetes during childhood. Infants in Taiwan with birth weights less than 2.5 kg or greater than 4.0 kg when delivered at term were more likely to develop type 2 diabetes between 6 to 18 years of age than children with birth weights between these values.
24 M E TA B O L I C P R O G R A M M I N G
MATERNAL DIABETES
Studies of the offspring of mothers with pregestational (type 1 or type 2) and/or gestational diabetes also indicate that an abnormal intrauterine environment results in long-term health consequences. Children and adults born to mothers with diabetes have increased obesity in adolescence, 8 more often experience impaired glucose tolerance 9,10 and impaired insulin secretion, 11,12 and have increased prevalence of type 2 diabetes.
8
GROWTH
Patterns of growth in infancy and childhood may influence later health. Soto and colleagues evaluated infants with gestational ages of 37 to 41 weeks. They reported that small for gestational age (SGA) babies whose weights crossed percentile lines on a standard growth chart had significantly higher fasting insulin levels at 1 year of age than appropriate for gestational age (AGA) or SGA babies who did not exhibit this weight pattern.
13 SGA babies whose lengths crossed percentile lines on standard growth charts had higher insulin secretion than AGA babies or SGA babies who did not exhibit this length pattern.
13 It is not known, however, whether these findings at 1 year of age persist throughout life. Bavdekar and colleagues reported that 8-year-old children who were low-birthweight infants but were heavy at age 8 had higher insulin concentrations, insulin resistance, and high levels of total and LDL cholesterol. In this study, the most adverse cardiovascular risk profiles were found for children who were light at birth but who had grown relatively heavy and tall at age 8.
14 Law and colleagues found that 22-yearold adults who had been small at birth but who gained weight rapidly between the ages of 1 and 5 years had the highest adult blood pressures.
15 Forsen et al. found that for both men and women, low birth weight followed by high growth rates after age 7 increased the risk of type 2 diabetes.
16
Not all research supports the hypothesis that low birth weight and post-natal growth pattern contribute to later health consequences. For example, Wilkin and colleagues concluded that insulin resistance at age 5 years is a function of excess current weight rather than low birth weight or weight change.
17
Rapid weight gain in which healthy infants gain beyond their expected growth channel has been linked to increased risk of overweight later in life. Healthy infants who gained weight unusually rapidly during the first 4 months of life were more likely to be overweight at 7 18 and 20 years of age, 19 and rapid growth of healthy infants during the first 12 months of life has also been linked to increased body mass index at 6 years of age.
20 While these studies indicate that unusually rapid growth during infancy may increase risk of obesity later in life, there are no known safe and effective interventions in early infancy for preventing childhood and adult obesity.
19 In addition, more rapid growth may be an appropriate goal for infants with chronic illness and/or failure to thrive.
TODDLERS
Little data on the long-term health consequences of toddler food and nutrient intakes exist; therefore, this area deserves further scrutiny. Moreover, the toddler years may be an opportune time to implement appropriate or specific dietary interventions in children exposed to an abnormal intrauterine environment, or in those who experienced unusually rapid growth, in order to help influence future health. Unfortunately, however, no human studies have determined whether dietary interventions in these at-risk children are appropriate or effective.
Clearly, more research is needed.
M E TA B O L I C P R O G R A M M I N G 25
REFERENCES
1.
Barker DJ. The fetal and infant origins of adult disease.
BMJ.
1990;301:1111.
2.
Ravelli GP, Stein ZA, Susser MW. Obesity in young men after famine exposure in utero and early infancy.
N Engl J Med.
1976;295:349-353.
3.
Hales CN, Barker DJ, Clark PM, et al. Fetal and infant growth and impaired glucose tolerance at age 64.
BMJ.
1991;303:
1019-1022.
4.
Rich-Edwards JW, Colditz GA, Stampfer MJ, et al. Birthweight and the risk for type 2 diabetes mellitus in adult women.
Ann Intern Med.
1999;130:278-284.
5.
Dabelea D, Pettitt DJ, Hanson RL, et al. Birth weight, type 2 diabetes, and insulin resistance in Pima Indian children and young adults.
Diabetes Care.
1999;22:944-950.
6.
Wei JN, Sung FC, Li CY, et al. Low birth weight and high birth weight infants are both at an increased risk to have type 2 diabetes among schoolchildren in Taiwan.
Diabetes Care.
2003;26:343-348.
7.
Poulsen P, Vaag AA, Kyvik KO, et al. Low birth weight is associated with NIDDM in discordant monozygotic and dizygotic twin pairs.
Diabetologia.
1997;40:439-446.
8.
Dabelea D, Knowler WC, Pettitt DJ. Effect of diabetes in pregnancy on offspring: follow-up research in the Pima Indians.
J Matern Fetal Med.
2000;9:83-88.
9.
Silverman BL, Metzger BE, Cho NH, et al. Impaired glucose tolerance in adolescent offspring of diabetic mothers.
Relationship to fetal hyperinsulinism.
Diabetes Care.
1995;18:611-617.
10. Plagemann A, Harder T, Kohlhoff R, et al. Glucose tolerance and insulin secretion in children of mothers with pregestational IDDM or gestational diabetes.
Diabetologia.
1997;40:1094-1100.
11.
Sobngwi E, Boudou P, Mauvais-Jarvis F, et al. Effect of a diabetic environment in utero on predisposition to type 2 diabetes.
Lancet.
2003;361:1861-1865.
12. Gautier JF, Wilson C, Weyer C, et al. Low acute insulin secretory responses in adult offspring of people with early onset type 2 diabetes.
Diabetes.
2001;50:1828-1833.
13.
Soto N, Bazaes RA, Pena V, et al. Insulin sensitivity and secretion are related to catch-up growth in small-for-gestationalage infants at age 1 year: results from a prospective cohort.
J Clin Endocrinol Metab.
2003;88:3645-3650.
14. Bavdekar A, Yajnik CS, Fall CH, et al. Insulin resistance syndrome in 8-year-old Indian children: small at birth, big at 8 years, or both? Diabetes.
1999;48:2422-2429.
15. Law CM, Shiell AW, Newsome CA, et al. Fetal, infant, and childhood growth and adult blood pressure: a longitudinal study from birth to 22 years of age.
Circulation.
2002;105:1088-1092.
16. Forsen T, Eriksson J, Tuomilehto J, et al. The fetal and childhood growth of persons who develop type 2 diabetes.
Ann Intern Med.
2000;133:176-182.
17.
Wilkin TJ, Metcalf BS, Murphy MJ, et al. The relative contributions of birth weight, weight change, and current weight to insulin resistance in contemporary 5-year-olds: the EarlyBird Study.
Diabetes.
2002;51:3468-3472.
18. Stettler N, Zemel BS, Kumanyika S, et al. Infant weight gain and childhood overweight status in a multicenter, cohort study.
Pediatrics.
2002;109:194-199.
19. Stettler N, Kumanyika SK, Katz SH, et al. Rapid weight gain during infancy and obesity in young adulthood in a cohort of
African Americans.
Am J Clin Nutr.
2003;77:1374-1378.
20. Gunnarsdottir I, Thorsdottir I. Relationship between growth and feeding in infancy and body mass index at the age of
6 years.
Int J Obes Relat Metab Disord.
2003;27:1523-1527.
Overweight Status and Risk
Contributor:
Barbara A. Dennison, MD
Clinical Professor of Epidemiology
State University of New York at Albany
Director, Bureau of Health Risk Reduction
Division of Chronic Disease Prevention and Adult Health
New York State Department of Health
Medical and drug information is constantly evolving because of ongoing research and clinical experience that are often subject to interpretation. While care has been taken to ensure the accuracy of the information presented, the reader is advised that Mead Johnson & Company, and the authors, editors, reviewers, contributors, and publishers of this material are not responsible for the continued currency of the information contained in this material, or any errors or omissions that might appear in this material, or for any consequences arising out of, or resulting from, the use of the material for any purpose or reason whatsoever.
Because of the dynamic nature of medical and drug information, readers are advised that decisions regarding drug or any other therapy must be based on the independent judgment of the clinician, information about a drug (eg, as reflected in the literature), and changing medical practices.
The Editors and Mead Johnson & Company
O V E R W E I G H T S TAT U S A N D R I S K 27 26 M E TA B O L I C P R O G R A M M I N G
INTRODUCTION
Changing environment and lifestyles have led to an imbalance in energy intake and expenditure resulting in an epidemic of overweight and obesity among adults, adolescents, and children, including toddlers. It is important to understand characteristics and behaviors associated with the development of overweight in toddlers, so children at risk can be identified and steps taken to prevent or slow the progression of childhood overweight.
PREVALENCE OF OVERWEIGHT IN CHILDREN
The prevalence of overweight among children 2 to 19 years of age has tripled in the past three decades, increasing from 5.1% in 1971–1974 to 17.1% in 2003–2004. During this same period, the prevalence of those “at risk of overweight” has increased from 10.2% to 16.5%.
1 For children ages 2 to 5 years the prevalence of overweight has more than doubled from 4.9% in 1971–1974 to 13.9% in 2003–2004.
1,2 In addition to the increasing prevalence of overweight, the degree of overweight in childhood has increased. That is, overweight children have become even more overweight.
2,3
Ogden and colleagues compared NHANES data from 2003–2004 with that from 1999–2000 and 2001–2002.
1
The sample included almost 4,000 subjects between 2 and 19 years of age. The percentage of 2- to 19-year-olds who was overweight increased from 13.9% and 15.4% in 1999–2000 and 2001–2002, respectively, to 17.1% in
2003–2004. Among subjects aged 2 to 5 years the percentage that was overweight increased from 10.3% in
1999–2000 to 13.9% in 2003–2004. Further results from this study are presented in Table 1.
Thompson and colleagues report that in the National Heart, Lung, and Blood Institute Growth and Health
Study, the incidence of overweight in females was greater between the ages of 9 and 12 years than in later adolescence.
4 Furthermore, girls who were overweight in childhood were 11 to 30 times more likely to be obese in early adulthood. Overweight in this study was associated with both elevated blood pressure and unhealthy blood lipid profiles.
Table 1. Prevalence (%) of Risk of Overweight and Overweight*
Age (years)
At risk of overweight or overweight †
All
2–19 2–5 6–11 12–19
1999–2000 28.2
22.0
29.8 30.0
2001–2002 30.0
23.5
32.2
31.1
2003–2004 33.6
26.2
37.2
34.3
Overweight ‡
1999–2000
2001–2002
2003–2004
13.9
15.4
17.1
10.3
10.6
13.9
15.1
16.3
18.8
14.8
16.7
17.4
Male
2–19 2–5 6–11 12–19
28.9 21.9
31.9 30.0
30.6 24.2
32.6
31.5
34.8
27.3
36.5
36.8
14.0
9.5
15.7
14.8
16.4 10.7
17.5
17.6
18.2
15.1
19.9
18.3
*Adapted from 21.
†BMI for age at 85th percentile or higher.
‡BMI for age at 95th percentile or higher.
Female
2–19 2–5 6–11 12–19
27.4
22.2
27.4 30.0
29.4 22.8
31.6 30.6
32.4
25.2
38.0
31.7
13.8
11.2
14.3
14.8
14.4
10.5
14.9
15.7
16.0
12.6
17.6
16.4
28 O V E R W E I G H T S TAT U S A N D R I S K
DEFINITIONS OF OVERWEIGHT
Health experts recommend evaluating body mass index (BMI) as a screening tool to determine if children are overweight or at risk of overweight.
5 When there is a question or uncertainty whether the excess weight reflects excess body fat, additional assessment such as measurement of triceps skin-fold thickness may be indicated. BMI is expressed as body weight in kilograms divided by the square of height in meters (kg/m 2 ). This is a weight for height index that tends to reflect excess body fat and is relatively easy to use. The U.S. Department of Health and
Human Services Centers for Disease Control and Prevention (CDC) publishes sex-specific growth charts of BMI by age.
6 The BMI percentiles indicated on the charts are derived from a nationally representative sample of children.
Once BMI is calculated, it is plotted against age on the sex-specific charts and the BMI percentile-for-age is determined. Children with a BMI at or above the 85th but less than the 95th sex-specific percentile-for-age are considered to be at risk of overweight. Children with a BMI at or above the 95th sex-specific percentile-for-age are considered “overweight.”
HEALTH RISKS ASSOCIATED WITH OVERWEIGHT
IN CHILDHOOD
Overweight in childhood warrants concern because it tends to persist over time and the greater the degree of overweight, the greater the risk and degree of overweight in adulthood.
7 Moreover, overweight is associated with increased health problems in childhood 8 (Table 2) as well as increased morbidity 9,10 and mortality in adulthood.
11
Table 2. Health Problems Associated With Overweight in Childhood
8
Cardiovascular
• Hypercholesterolemia
• Dyslipidemia
• Hypertension
Pulmonary
• Asthma
• Obstructive sleep apnea syndrome
• Pickwickian syndrome
Endocrine
• Hyperinsulinism
• Insulin resistance
• Impaired glucose tolerance
• Type 2 diabetes
Mental Health
• Depression
• Low self-esteem
Orthopedic
• Genu verum
• Slipped capital femoral epiphysis
• Arthritis
Gastrointestinal/hepatic
• Nonalcoholic steatohepatitis
• Gall bladder disease
ENERGY IMBALANCE
Energy imbalance contributes to overweight: children who consume more energy (calories) than needed for activities of daily life, physical activity plus growth, become overweight. Research indicates that over consumption of calories by toddlers may be a bigger problem than previously realized.
12,13 Devaney and colleagues found that reported energy intakes of toddlers ages 12 to 24 months exceeded estimated energy requirements by 31%.
12 While over consumption is probably an important issue for toddlers, it is unlikely that the discrepancy
O V E R W E I G H T S TAT U S A N D R I S K 29
30 between calorie intakes and estimated energy requirements are actually this high since the prevalence of overweight would be even higher than reported.
12 The authors speculate that the discrepancy may have been caused, in part, by parents over-estimating the amount of food actually consumed by the child. Alternately, the estimated energy requirements might be underestimated secondary to parents underestimating the child’s weight. For example, parents might have reported the child’s weight at the most recent checkup instead of the child’s current weight. Nevertheless, these researchers stated that the high energy intakes relative to estimated requirements “reinforce the importance of encouraging health professionals to monitor the weight gain of infants and toddlers….” 12
Several food consumption trends could contribute to over consumption of calories and to overweight: increasing portion sizes, frequent use of fast foods, consumption of sweet beverages, and decreased consumption of vegetables, to name a few. Typical food portion sizes have increased dramatically over the past 20 years 14 and larger portion sizes promote increased food consumption by children.
15,16 Bowman and colleagues reported that on a typical day, about 30% of children 4 to 19 years of age consumed food from a fast food restaurant.
17 Children who consumed fast foods ate almost 200 calories more per day than children who did not consume fast foods and their diets were of poorer quality. Children who consumed fast foods also consumed higher amounts of sugar-sweetened beverages, less milk, and fewer fruits and vegetables.
17
Intake of sweet beverages has been linked to weight gain and overweight in children.
18 Ludwig and colleagues reported that for each additional serving of a sweetened beverage consumed by 6th- and 7th-grade children, BMI increased by
The AAP CON has stated,
“
Early recognition of excessive weight gain relative to linear
0.24 kg/m 2 and the incidence of obesity increased by about
60% (odds ratio 1.6).
18 Dennison and colleagues evaluated
growth should become routine in pediatric ambulatory care settings.
toddlers ages 2 through 5 years and reported that children who consumed more than 12 ounces per day of fruit juice were more likely to have BMI above the 75th and the 90th percentiles than children who consumed less than 12 ounces
BMI…should be calculated and plotted periodically.
”
18 per day.
19 Since then, other research has also noted an association between higher fruit juice intakes among children and being overweight.
20 One study, however, noted a trend but did not find a statistically significant difference.
21
In response to the totality of findings, the American Academy of Pediatrics (AAP) Committee on Nutrition recommends that fruit juice consumption by children 1 to 6 years old be limited to no more than 4 to 6 ounces per day.
22
Sweet beverages may be particularly problematic when it comes to weight control because they provide significant calories, and people do not compensate for calories consumed from liquid foods as well as they compensate for calories from solid foods.
23 Sweet beverages, including 100% juice, fruit drinks and carbonated beverages, may also potentially contribute to overweight by displacing milk in toddlers’ diets, an excellent source of dietary calcium.
24 Although more studies are needed, 25 research indicates that there is a significant negative relationship between children’s average calcium intake over several years and their body fat at 6 years 26 and 8 years of age.
24 Skinner et al. suggested that children could potentially reduce their body fat by about 0.4% by increasing their calcium intake with one 8-ounce glass of skim milk or 8 ounces of yogurt per day (about 300 mg calcium in each).
24
O V E R W E I G H T S TAT U S A N D R I S K
Studies in adults find that consuming a wide variety of vegetables is associated with reduced body fat.
27 Many toddlers, however, do not consume vegetables. One-fifth (18% to 23%) of toddlers between the ages of 12 and 24 months in the Feeding Infants and Toddlers Study did not consume any vegetables on the day of the survey.
28 In another study, only one-fifth of children ages 2 to 9 years consumed the recommended three or more servings per day of vegetables.
29
Regular physical activity promotes maintenance of a healthy weight, while physical inactivity has been linked to increased body fat 40 and increased BMI 51 in toddlers. The Institute of Medicine 23 recommends that children participate in at least 1 hour of moderately vigorous physical activity per day, while the American Alliance of
Health, Physical Education, Recreation, and Dance 32 recommends that preschool-age children participate in at least 60 minutes of structured physical activity and at least 60 minutes of unstructured physical activity daily.
Furthermore, they recommend that preschoolers should not be sedentary for more than 60 minutes at a time except when sleeping.
FAMILY AND ENVIRONMENT
Characteristics of the child’s family and environment may be important predictors of overweight. A child with an obese parent has a significantly higher risk of being overweight than a child whose parents are not obese.
33
Having a mother who is obese appears to be a stronger predictor of childhood overweight than having a father who is obese (odds ratio 2.8–3.6 vs 2.4–2.9, respectively).
33 Strauss and Knight reported that children whose mothers were obese had more than three times the risk of overweight than children whose mothers were not obese.
34 Parental obesity is a more powerful predictor of a child’s risk of being obese as a young adult among younger children (1 to 5 years of age) than older children (6 to 17 years of age), while the risk associated with the child’s overweight status increases with increasing child age.
33 Among children, aged 1 to 5 years, those with two obese parents are 13.6–15.3 times more likely to be obese as a young adult compared to those with no obese parents. Among 6- to 17-year-old children, those with two obese parents compared with those with no obese parents, are 2.0–5.6 times as likely to be obese as a young adult. For children of all ages, those with one obese parent compared with those with no obese parents, have an increased odds of 2.2–3.2 of being obese as a young adult.
33 Children who live with a single parent, whose mothers have less than a high school education, whose parents do not work, and whose families have low incomes are at greater risk of being overweight.
34 In addition, after adjustment for these factors, children who received the least amount of cognitive stimulation at home were twice as likely to become overweight as children who received the highest amount of cognitive stimulation at home.
34
Television viewing appears to be an important predictor of overweight status among children as well as adults. Andersen and colleagues found that children (ages 8 to 16 years) who watched 4 or more hours per day of television had significantly greater body fat and a higher BMI than children who watched less than
2 hours.
35 Television viewing also increases the risk of being overweight for toddlers.
36 Dennison and colleagues found that 40% of toddlers (ages 1 to 5 years) had a television in their bedroom, and those with a television in their bedroom were significantly more likely to be overweight or at a risk of overweight (have a BMI above the
85th percentile) than toddlers without a television in the bedroom (odds ratio 1.31).
36
O V E R W E I G H T S TAT U S A N D R I S K 31
Television viewing may affect weight by influencing eating behaviors, food choices, and activity patterns.
Unpublished data from Dennison and colleagues indicate that over 50% of children who watch television in their bedrooms always or usually snack while watching television.
37 Viewing television during meals is associated with higher intakes of meat, pizza, salty snacks, and soda and lower intakes of fruits, vegetables, and juice.
38 Foods most frequently advertised to young children tend to be relatively high in calories, and a study finds that children exposed to a television commercial twice in a 30-minute cartoon were 3 times more likely to request the advertised item.
39 The amount of time children watch television is also positively related to how frequently they request advertised food items, and the more often they requested these items, the more likely their parents were to purchase them.
40 The relationship between television viewing and physical activity in toddlers is less clear. One study of preschool children, however, found a weak, negative association with physical activity levels.
41 Due to the relationship between television viewing and adverse health effects, such as aggressive behavior and overweight in children, the AAP Committee on Public Education recommends that children over 2 years of age limit their viewing to no more than 1 to 2 hours per day of non-violent, educational television or other media.
42
INFANT NUTRITION AND GROWTH PATTERN
Infant nutrition appears to have an important potential impact on weight status. Several research studies indicate that breastfed infants are less likely than infants fed formula to become overweight as children or adults.
43-45 Studies also found that the longer the duration of breastfeeding and the greater the period of exclusive breastfeeding (feeding no other foods or beverages), the lower the subsequent risk of being overweight.
45 Since the decision to breastfeed, the duration of breastfeeding, and the period of exclusive breastfeeding are not random occurrences and cannot be randomized in research studies, it is difficult to know exactly what is responsible for the observed differences between breastfed and formula-fed infants.
The decreased risk of overweight might be due to decreased caloric intake secondary to mode of feeding
(breastfeeding vs formula feeding), the number of people feeding the infant (one vs many), biological or physiological factors in human milk, differences in characteristics of mothers who breastfeed compared with those who formula feed, and/or differences in maternal feeding and parenting practices. Mothers who breastfeed and mothers who do not often differ with respect to educational attainment, race/ethnicity, personal nutrition practices, and/or other lifestyle behaviors that may lead to biased estimates of the beneficial effects associated with breastfeeding.
Rapid weight gain, in which healthy infants gain beyond their expected growth channel, has been linked to increased risk of overweight later in life. Healthy infants who gained weight unusually rapidly during the first 4 months of life were more likely to be overweight at 7 years 18 or 20 years of age, 19 and rapid growth of healthy infants during the first 12 months of life has also been linked to increased body mass index at 6 years of age.
20
While these studies indicate that unusually rapid growth during infancy may increase risk of obesity later in life, there are no known safe and effective interventions in early infancy for preventing childhood and adult obesity.
19
WHAT TO DO?
One of the first steps in preventing childhood overweight is early recognition of the child at increased risk of becoming overweight. Only about one-fifth of parents recognize when their own child is overweight.
49
Unfortunately, many pediatric health practitioners often fail to identify children who are overweight or at risk of overweight because they do not determine BMI or assess BMI percentile for age. The AAP Committee on
Nutrition recommends that physicians/pediatric care providers calculate and plot BMI by age once a year in all children and adolescents, and that they use the BMI percentile-for-age as well as change in BMI percentile, to determine if the weight gain is excessive relative to linear growth.
8 BMI charts and online training modules on usage are available at www.cdc.gov/growthcharts/. Other recommendations related to preventing overweight in children are summarized in Table 3.
Table 3. Physician Measures to Help Prevent Overweight in Children
8,13,42,47
• Identify and track patients at increased risk due to family, socioeconomic, ethnic, cultural and/or environmental factors
• Promote healthy eating patterns; The USDA Food Guide Pyramid for Young Children is a useful tool
• Calculate and plot BMI-for-age yearly
• Promote physical activity; The Institute of Medicine recommends 1 hour of physical activity per day for children
• Identify excessive weight gain relative to linear growth using change in BMI percentile-for-age
• Recommend limiting television and video viewing to no more than 1 to 2 hours per day for children older than 2 years of age, and discourage any television viewing for children less than 2 years of age
• Promote breastfeeding of infants and advocate for paid maternity leave supportive worksite policies/practices
• Recognize and monitor obesity-associated disorders/diseases
If BMI percentile-for-age indicates that a child is at risk of overweight or is overweight, discussion with the family and weight goals become important. For toddlers with BMI measurements between the 85th and 94th percentiles, or BMI measurements greater than the 95th percentile and no secondary complications, experts recommend that maintaining baseline body weight is the primary weight goal.
5 As children maintain their weight while growing in height, BMI will decrease.
5 Improving dietary and physical activity patterns will help achieve these goals. Toddlers who are overweight (BMI greater than the 95th percentile) and experiencing secondary complications may be better served by referral to health care professionals specializing in pediatric weight control.
The American Heart Association (AHA) policy on dietary recommendations for children and adolescents has been endorsed by the AAP.
48 Recommendations are food based, not nutrient based. Thus, the recommended number of servings for grains, fruits, vegetables, milk/dairy, and lean meats/beans are given for children between the ages of
32 O V E R W E I G H T S TAT U S A N D R I S K O V E R W E I G H T S TAT U S A N D R I S K 33
1 and 18 years by gender. In addition, the statement provides guidelines for improving the nutritional quality of the diet after weaning, tips for parents to improve nutrition in young children, and strategies for schools to promote health and nutrition.
The North American Society for Pediatric Gastroenterology, Hepatology, and Nutrition suggests several approaches to treating overweight including behavioral reinforcement, dietary modification, strategies to increase physical activity, therapeutic approaches, and parenting skills to support weight control efforts.
49
In 2006 the American Dietetic Association released their position on pediatric overweight following an extensive literature review.
50 They found:
“…that pediatric overweight intervention requires a combination of family-based and schoolbased multicomponent programs that include the promotion of physical activity, parent training/modeling, behavioral counseling, and nutrition education. Furthermore…communitybased and environmental interventions are recommended as among the most feasible ways to support healthful lifestyles for the greatest numbers of children and their families.”
REFERENCES
1.
Ogden CL, Carroll MD, Curtin LR, et al. Prevalence of overweight and obesity in the United States, 1999-2004.
JAMA.
2006;295:1549-1555.
2.
Jolliffe D. Extent of overweight among US children and adolescents from 1971 to 2000.
Int J Obes Relat Metab Disord.
2004;28:4-9.
3.
Edmunds LS, Woelfel ML, Dennison BA, et al. Overweight trends among children enrolled in the New York State special supplemental nutrition program for women, infants, and children.
J Am Diet Assoc.
2006;106:113-117.
4.
Thompson DR, Obarzanek E, Franko DL, et al. Childhood Overweight and Cardiovascular Disease Risk Factors: The National
Heart, Lung, and Blood Institute Growth and Health Study.
J Pediatr.
2007;150:18-25.
5.
Barlow SE, Dietz WH. Obesity evaluation and treatment: Expert Committee recommendations. The Maternal and Child
Health Bureau, Health Resources and Services Administration and the Department of Health and Human Services.
Pediatrics.
1998;102:E29.
6.
U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Health
Statistics.
CDC Growth Charts.
2000. Available at: http:www.cdc.gov/growthcharts. Accessed June 2, 2004.
7.
Serdula MK, Ivery D, Coates RJ, et al. Do obese children become obese adults? A review of the literature.
Prev Med.
1993;22:167-177.
8.
American Academy of Pediatrics Committee on Nutrition. Prevention of pediatric overweight and obesity.
Pediatrics.
2003;112:424-430.
9.
Must A, Strauss RS. Risks and consequences of childhood and adolescent obesity.
Int J Obes Relat Metab Disord.
1999;23(suppl 2):S2-S11.
10. Must A, Jacques PF, Dallal GE, et al. Long-term morbidity and mortality of overweight adolescents. A follow-up of the
Harvard Growth Study of 1922 to 1935.
N Engl J Med.
1992;327:1350-1355.
11.
Gunnell DJ, Frankel SJ, Nanchahal K, et al. Childhood obesity and adult cardiovascular mortality: a 57-y follow-up study based on the Boyd Orr cohort.
Am J Clin Nutr.
1998;67:1111-1118.
12. Devaney B, Ziegler P, Pac S, et al. Nutrient intakes of infants and toddlers.
J Am Diet Assoc.
2004;104(suppl):S14-S21.
13.
Institute of Medicine.
Dietary Reference Intakes for Energy, Carbohydrate, Fiber, Fat, Fatty Acids, Cholesterol, Protein, and
Amino Acids.
Washington, D.C.: National Academy Press .
2002.
14. Young LR, Nestle M. Expanding portion sizes in the US marketplace: implications for nutrition counseling.
J Am Diet Assoc.
2003;103:231-234.
15. Rolls BJ, Engell D, Birch LL. Serving portion size influences 5-year-old but not 3-year-old children's food intakes.
J Am Diet
Assoc.
2000;100:232-234.
16. Orlet FJ, Rolls BJ, Birch LL. Children's bite size and intake of an entree are greater with large portions than with ageappropriate or self-selected portions.
Am J Clin Nutr.
2003;77:1164-1170.
17.
Bowman SA, Gortmaker SL, Ebbeling CB, et al. Effects of fast-food consumption on energy intake and diet quality among children in a national household survey.
Pediatrics.
2004;113:112-118.
18. Ludwig DS, Peterson KE, Gortmaker SL. Relation between consumption of sugar-sweetened drinks and childhood obesity: a prospective, observational analysis.
Lancet.
2001;357:505-508.
34 O V E R W E I G H T S TAT U S A N D R I S K
19. Dennison BA, Rockwell HL, Baker SL. Excess fruit juice consumption by preschool-aged children is associated with short stature and obesity.
Pediatrics.
1997;99:15-22.
20. Tanasescu M, Ferris AM, Himmelgreen DA, et al. Biobehavioral factors are associated with obesity in Puerto Rican children.
J Nutr.
2000;130:1734-1742.
21. Skinner JD, Carruth BR, Moran J, Iii, et al. Fruit juice intake is not related to children's growth.
Pediatrics.
1999;103:58-64.
22. American Academy of Pediatrics Committee on Nutrition. The use and misuse of fruit juice in pediatrics.
Pediatrics.
2001;107:1210-1213.
23. Mattes RD. Dietary compensation by humans for supplemental energy provided as ethanol or carbohydrate in fluids.
Physiol Behav.
1996;59:179-187.
24. Skinner JD, Bounds W, Carruth BR, et al. Longitudinal calcium intake is negatively related to children's body fat indexes.
J Am Diet Assoc.
2003;103:1626-1631.
25. Weaver CM, Boushey CJ. Milk–good for bones, good for reducing childhood obesity? J Am Diet Assoc.
2003;103:1598-1599.
26. Carruth BR, Skinner JD. The role of dietary calcium and other nutrients in moderating body fat in preschool children.
Int J Obes Relat Metab Disord.
2001;25:559-566.
27. McCrory MA, Fuss PJ, McCallum JE, et al. Dietary variety within food groups: association with energy intake and body fatness in men and women.
Am J Clin Nutr.
1999;69:440-447.
28. Fox MK, Pac S, Devaney B, et al. Feeding infants and toddlers study: What foods are infants and toddlers eating?
J Am Diet Assoc.
2004;104(suppl):S22-S30.
29. Nicklas T, Johnson R. Position of the American Dietetic Association: Dietary guidance for healthy children ages 2 to 11 years.
J Am Diet Assoc.
2004;104:660-677.
30. Li R, O'Connor L, Buckley D, et al. Relation of activity levels to body fat in infants 6 to 12 months of age.
J Pediatr.
1995;126:353-357.
31.
Klesges RC, Klesges LM, Eck LH, et al. A longitudinal analysis of accelerated weight gain in preschool children.
Pediatrics.
1995;95:126-130.
32. National Association for Sport and Physical Education.
Active Start: A Statement of Physical Activity Guidelines for Children
Birth to Five Years.
Reston, VA: American Alliance for Health, Physical Education, Recreation and Dance; 2002.
33. Whitaker RC, Wright JA, Pepe MS, et al. Predicting obesity in young adulthood from childhood and parental obesity.
N Engl J Med.
1997;337:869-873.
34. Strauss RS, Knight J. Influence of the home environment on the development of obesity in children.
Pediatrics.
1999;103:e85.
35. Andersen RE, Crespo CJ, Bartlett SJ, et al. Relationship of physical activity and television watching with body weight and level of fatness among children: results from the Third National Health and Nutrition Examination Survey.
JAMA.
1998;279:938-942.
36. Dennison BA, Erb TA, Jenkins PL. Television viewing and television in bedroom associated with overweight risk among low-income preschool children.
Pediatrics.
2002;109:1028-1035.
37. Fitzpatrick E, Edmunds LS, Dennison BA. Positive effects of family dinner are undone by television viewing.
J Am Diet
Assoc.
2007;107:666-671.
38. Coon KA, Goldberg J, Rogers BL, et al. Relationships between use of television during meals and children's food consumption patterns.
Pediatrics.
2001;107:E7.
39. Borzekowski DL, Robinson TN. The 30-second effect: an experiment revealing the impact of television commercials on food preferences of preschoolers.
J Am Diet Assoc.
2001;101:42-46.
40. Taras HL, Sallis JF, Patterson TL, et al. Television's influence on children's diet and physical activity.
J Dev Behav Pediatr.
1989;10:176-180.
41. Durant RH, Baranowski T, Johnson M, et al. The relationship among television watching, physical activity, and body composition of young children.
Pediatrics.
1994;94:449-455.
42. American Academy of Pediatrics Committee on Public Education. Children, adolescents, and television.
Pediatrics.
2001;107:423-426.
43. von Kries R, Koletzko B, Sauerwald T, et al. Breastfeeding and obesity: cross sectional study.
BMJ.
1999;319:147-150.
44. Hediger ML, Overpeck MD, Kuczmarski RJ, et al. Association between infant breastfeeding and overweight in young children.
JAMA.
2001;285:2453-2460.
45. Dewey KG. Is breastfeeding protective against child obesity? J Hum Lact.
2003;19:9-18.
46. Baughcum AE, Chamberlin LA, Deeks CM, et al. Maternal perceptions of overweight preschool children.
Pediatrics.
2000;106:1380-1386.
47. U.S. Department of Agriculture, Center for Nutrition Policy and Promotion.
The Food Guide Pyramid for Young Children.
2003. Available at: http:www.usda.gov/cnpp/KidsPyra/. Accessed June 2, 2004.
48. American Heart Association, Gidding SS, Dennison BA, et al. Dietary recommendations for children and adolescents: a guide for practitioners.
Pediatrics.
2006;117:544-559.
49. Baker S, Barlow S, Cochran W, et al. Overweight children and adolescents: a clinical report of the North American Society for Pediatric Gastroenterology, Hepatology and Nutrition.
J Pediatr Gastroenterol Nutr.
2005;40:533-543.
50. American Dietetic Association. Position of the American Dietetic Association: individual-, family-, school-, and communitybased interventions for pediatric overweight.
J Am Diet Assoc.
2006;106:925-945.
O V E R W E I G H T S TAT U S A N D R I S K 35
36
DHA in Toddler Nutrition
Contributor:
Sheila M. Innis, PhD, MSc
Professor, Department of Pediatrics
Director, Nutrition Research Program
BC Research Institute for Children’s and Women’s Health
University of British Columbia
Medical and drug information is constantly evolving because of ongoing research and clinical experience that are often subject to interpretation. While care has been taken to ensure the accuracy of the information presented, the reader is advised that Mead Johnson & Company, and the authors, editors, reviewers, contributors, and publishers of this material are not responsible for the continued currency of the information contained in this material, or any errors or omissions that might appear in this material, or for any consequences arising out of, or resulting from, the use of the material for any purpose or reason whatsoever.
Because of the dynamic nature of medical and drug information, readers are advised that decisions regarding drug or any other therapy must be based on the independent judgment of the clinician, information about a drug (eg, as reflected in the literature), and changing medical practices.
The Editors and Mead Johnson & Company
D H A I N T O D D L E R N U T R I T I O N 37
INTRODUCTION
The study of the roles of docosahexaenoic acid (DHA; 22:6n-3; a 22-carbon, 6-double bond, n-3 fatty acid) in human development, neurologic and visual function, and in reducing the incidence and severity of a variety of diseases is a rapidly moving field of research. Dietary DHA has been associated with improvements in visual and cognitive function through epidemiological studies with breastfed 1,2 and, in some randomized, controlled studies, formula-fed infants.
3-5 In adults, the role of n-3 fatty acids, including DHA, in promoting cardiovascular health, is becoming increasingly recognized, and is receiving more public emphasis.
6-8 The importance of dietary n-3 fatty acids for infant brain and retinal development and in adult health highlights the need to also consider DHA status and n-3 fatty acid nutrition in children, particularly those between the ages of 1 and 5 years, at which time considerable brain development is continuing.
9
SOURCES OF DHA
Humans can make DHA from the essential dietary fatty acid, α -linolenic acid (18:3n-3, LNA), 10 which is an 18carbon polyunsaturated fatty acid with 3 double bonds found in some vegetable oils (like canola, soybean, and flax), nuts, and seeds (such as walnuts). Synthesis of DHA from LNA occurs largely in the liver through a series of desaturation, elongation, and oxidation reactions that convert LNA via eicosapentaenoic acid (20:5n-3, EPA) to DHA (Figure 1).
11 Despite the ability to convert LNA to DHA, the activity of the desaturase pathway in humans appears to be low and variable. Estimates derived from studies with stable isotope tracers indicate that the amount of LNA converted to DHA varies from <1% to about 9%; the conversion is higher in less mature infants than in older infants, and in pregnant women compared to non-pregnant women.
12-15 In addition to LNA, DHA is also consumed in the diet. However, because the desaturase enzymes required for conversion of LNA to DHA are present only in animal cells, DHA is present in the diet only in animal foods (fish, meats, and eggs) and is not found in foods of vegetable origin (except certain formulated foods and dietary supplements that contain supplemented DHA). In addition, cow and other animal milks and dairy products contain very low amounts of
DHA. Soy and other milk substitutes based on vegetable products are also devoid of DHA. Both human milk and
LCPUFA-supplemented infant formula provide DHA.
Figure 1. Essential Fatty Acid Metabolism
PHYSIOLOGICAL ROLES FOR DHA
The high concentration of DHA in membrane phospholipids (such as phosphatidylserine and phosphatidylethanolamine) of the brain gray matter, retina, and heart indicates that this fatty acid is vital to the development and function of these tissues. Reduced amounts of DHA in nerve cell membranes and in the visual elements of the retina are associated with decreased scores on tests of learning, photoreceptor cell function, and visual resolution acuity.
10 DHA is also a precursor for 17S-hydroxy-containing docosanoids (docosatrienes and 17S-series resolvins) that appear to be important mediators of inflammation and link DHA to immunological function.
16
In addition, n-3 fatty acids have been shown to be involved in regulation of gene expression in the brain and other organs.
17,18
DHA AND THE GROWING BRAIN
Studies of autopsy material from human infants have provided evidence that the dietary intake of DHA influences the amount of DHA accumulated in the developing infant brain.
19 Large amounts of DHA are needed during brain growth and development to support the synthesis of new membrane lipids. Although the rate of
DHA accretion relative to body weight is highest during the third trimester of pregnancy and first few months after birth, 20 human brain growth and remodeling continue well beyond this time. DHA is particularly enriched in synaptic membranes, where it is involved in neurotransmitter metabolism and receptor function.
10 Only about
1% of the adult number of synapses are present in the human brain at birth, and considerable growth and reorganization of synapses occurs through early childhood.
21
The concept of critical periods in development at which the fetus or young child is susceptible to long-lasting effects of early nutritional deficiencies or other environmental stressors is well established. The effects of early iron deficiency, iodine deficiency, and alcohol exposure all provide excellent examples of the long-lasting effects of early nutrient deficiency or exposure to toxic compounds. One of the effects of reduced DHA in the brain is altered metabolism of the neurotransmitters dopamine and serotonin.
10 A working model, similar to that developed to explain the effects of iron deficiency on cognitive and behavioral development in infants, 22 can be proposed to explain how poor dietary fat choices may adversely affect infant and child development.
Figure 2. Proposed Model to Explain How Poor Dietary Fat Choices May Affect Infant and Child Development
D H A I N T O D D L E R N U T R I T I O N 39 38 D H A I N T O D D L E R N U T R I T I O N
40
INDICATORS OF DHA STATUS
Clinical signs of inadequate levels of DHA will clearly reflect the functional roles of DHA in the central nervous system. These include altered performance on a variety of tests of learning and changes in electroretinograph
(ERG) recordings and measures of visual resolution acuity.
10 Of importance, there are no overt signs of n-3 fatty acid deficiency, such as growth failure or skin lesions. Measures of the amount of DHA in red blood cell phospholipids or plasma lipids reflect the dietary intake of DHA in infants, as they do in adults.
23-26 Biochemical markers of DHA status, or the blood level of DHA at which functional impairment of the central nervous system, heart, or other organs requiring n-3 fatty acids occurs, have not been identified.
DHA INTAKES OF TODDLERS
Breastfed infants and infants fed formulas with DHA receive a source of n-3 fatty acids. However, weaning to cow’s milk and the replacement of energy from breast milk and infant formula with cereals, fruits, and vegetables (which are low in fat and have no DHA) will result in a decrease in the amount of n-3 fatty acids consumed. Infants between the ages of 1 and 6 months who consume breast milk or formula with 0.3% of the fatty acids as DHA, and 3.7 g fat/dL will receive 86 mg DHA with an intake of 780 mL breast milk or formula per day. Innis and colleagues have estimated the intakes of n-3 fatty acids, as well as that for n-6 linoleic acid and trans fatty acids among toddlers and young children 18 to 60 months of age (Table 1). In toddlers and children 18 to 60 months of age, the intake of LNA is about 1.7 g/day and the intake of DHA is about 88 mg/day, with the lowest intake of about 40 mg DHA/day occurring at 18 to 24 months of age.
27
The richest dietary source of DHA is fatty fish, which is not
“
If one accepts that formula feeding without DHA confers a DHA status which puts that infant at risk
widely or consistently consumed by many young children. It is also important to note that the intake of LNA among many toddlers is also often low, since at this age many children do not consume significant amounts of LNA from
for lower visual acuity and lower scores on behavioral tests, then the
DHA status of children 18 to 60 months could also place toddlers
polyunsaturated oils in salad dressings and unesterified margarines. In addition, the U.S. Environmental Protection
Agency and Food and Drug Administration have recommended limits on fish consumption for young children
at risk.”
“The DHA status of toddlers is
due to concerns about potential negative effects of methyl mercury, which is a developmental neurotoxin and for which the major source of human exposure is fish 28 . Such concerns over the safety of fish could potentially lower DHA intakes.
comparable to that of infants fed formula without DHA.
”
Table 1. Linoleic Acid,
α
-Linolenic Acid, DHA, and Trans Fatty Acid Intakes of Young
Children Ages 18 to 60 Months in Canada
Total Fat (% Calories) linoleic acid, g a-linolenic acid, g
DHA, mg trans fatty acids, g
All Children
32.7±0.6
8.8±0.4
1.7±0.12
88±10
4.8±3.1
Values are means ± standard error, adapted from Innis.
27
18 to 24 months 24 to 36 months 37 to 60 months
32±1.8
34.6±1.5
32.4±0.8
5.8±0.6
1.16±0.16
9±0.6
2.02±0.23
9.4±0.6
1.72±0.17
41±10
3.5±1.9
95±16
5.3±3.9
96±14
5±3.0
D H A I N T O D D L E R N U T R I T I O N
DHA STATUS OF TODDLERS
In addition to low intakes of DHA during the toddler years, the DHA status of children ages 18 to 60 months is lower than in newborns or breastfed infants or in children of older ages (Figure 3). Innis and colleagues evaluated the red blood cell phosphatidylethanolamine (RBC-PE) DHA concentrations of 84 toddlers 18 to 60 months of age
(Figure 3). The DHA status of the 18- to 60-month-old children was comparable to that of 3-month-old infants fed formula without DHA. Other investigators have reported lower visual resolution acuity and scores on tests of mental development in infants fed formulas without DHA and with comparable blood levels of DHA to those
Innis et al. found in 18- to 60-month-old children.
3-5
Figure 3. Fatty Acids (%) From DHA in RBC-PE
One factor that may influence the DHA status of toddlers is the intake of the n-6 fatty acid, linoleic acid. Linoleic acid (LA, 18:2n-6) is an 18-carbon, 2-double bond, n-6 fatty acid and is an essential dietary fatty acid. LA is metabolized through desaturation and elongation reactions to arachidonic acid (ARA) and is believed to use the same enzymes as those required to convert LNA to DHA (Figure 1). Dietary sources of linoleic acid are vegetable oils (especially corn, soybean, and safflower oil). It has been suggested that the intakes of linoleic acid in Western countries are too high. Further, research in animals has shown that increasing dietary intakes of LA at constant intakes of LNA decreases DHA in tissues.
29 Analysis of the dietary intakes of toddlers and young children in studies by Innis revealed an inverse relation between the dietary intake of LA and DHA status, which could not be explained by differences in the intake of either LNA or DHA. Children in the lowest tertile of RBC-PE DHA had the highest intakes of linoleic acid, and a significant inverse linear trend was present between the intake of LA and
DHA status.
27
D H A I N T O D D L E R N U T R I T I O N 41
42
Table 2. DHA Status Is Inversely Related to Linoleic Acid Intake in Children
18 to 60 Months
Median, g DHA/100 g RBC-PE fatty acids
Diet % kcal from fat
Linoleic acid, g
Linolenic acid, g
DHA, mg
Values are means ± standard error, adapted from Innis.
27
1
1.8
32
9±0.7
1.7±0.2
91±20
Tertile of RBC-PE DHA
2 3
3.2
33
9±0.7
4.5
32
7.5±0.7
1.8±0.2
70±12
1.3±0.13
99±24
4
5.9
33
6.7±1.0
1.5±0.2
92±41
The dietary intake data also showed that the intakes of trans fatty acids in toddlers were greater than the intakes of LNA and also inversely related to DHA status (Table 1). Some investigators have hypothesized that trans fatty acids may adversely affect n-3 fatty acid metabolism, infant development, and learning behavior.
30,31 The LA and trans fatty acid intakes of toddlers deserve further evaluation.
SUMMARY
Rapid brain growth and development continues in the toddler years, and DHA is an important component of lipids in the brain that could potentially affect early cognitive and behavioral development. Research indicates that the DHA status and DHA intakes of toddlers are lower than those of infants and children of older ages. The importance of adequate n-3 fatty acid nutrition and the low DHA status of toddlers indicate that n-3 fatty acid nutrition of children ages 1 to 5 years deserves further scrutiny.
“
Children in the highest tertile of linoleic acid intake had the lowest DHA status.
”
REFERENCES
1.
Innis SM, Gilley J, Werker J. Are human milk long-chain polyunsaturated fatty acids related to visual and neural development in breastfed term infants? J Pediatr.
2001;139:532-538.
2.
Jorgensen MH, Hernell O, Hughes E, et al. Is there a relation between docosahexaenoic acid concentration in mothers’ milk and visual development in term infants? J Pediatr Gastroenterol Nutr.
2001;32:293-296.
3.
Birch EE, Hoffman DR, Uauy R, et al. Visual acuity and the essentiality of docosahexaenoic acid and arachidonic acid in the diet of term infants.
Pediatr Res.
1998;44:201-209.
4.
Birch EE, Hoffman DR, Castañeda YS, et al. A randomized controlled trial of long-chain polyunsaturated fatty acid supplementation of formula in term infants after weaning at 6 wk of age.
Am J Clin Nutr.
2002;75:570-580.
5.
Hoffman DR, Birch EE, Castañeda YS, et al. Visual function in breastfed term infants weaned to formula with or without long-chain polyunsaturates at 4 to 6 months: a randomized clinical trial.
J Pediatr.
2003;142:669-677.
6.
Institute of Medicine.
Dietary Reference Intakes for Energy, Carbohydrate, Fiber, Fat, Fatty Acids, Cholesterol, Protein, and
Amino Acids . Washington, D.C.: National Academy Press .
2002.
7.
Kris-Etherton PM, Harris WS, Appel LJ. Fish consumption, fish oil, omega-3 fatty acids, and cardiovascular disease.
Circulation.
2002;106:2747-2757.
8.
Simopoulos AP, Leaf A, Salem N, Jr. Workshop on the essentiality of and recommended dietary Intakes for omega-6 and omega-3 fatty acids.
J Am Coll Nutr.
1999;18:487-489.
9.
Rice D, Barone S, Jr. Critical periods of vulnerability for the developing nervous system: evidence from humans and animal models.
Environ Health Perspect.
2000;108(suppl 3):511-533.
D H A I N T O D D L E R N U T R I T I O N
10. Innis SM. Perinatal biochemistry and physiology of long-chain polyunsaturated fatty acids.
J Pediatr.
2003;143(suppl):S1-S8.
11.
Sprecher H. Metabolism of highly unsaturated n-3 and n-6 fatty acids.
Biochim Biophys Acta.
2000;1486:219-231.
12. Burdge GC, Wootton SA. Conversion of alpha-linolenic acid to eicosapentaenoic, docosapentaenoic and docosahexaenoic acids in young women.
Br J Nutr.
2002;88:411-420.
13.
Burdge GC, Wootton SA. Conversion of alpha-linolenic acid to palmitic, palmitoleic, stearic and oleic acids in men and women.
Prostaglandins Leukot Essent Fatty Acids.
2003;69:283-290.
14. Uauy R, Mena P, Wegher B, et al. Long chain polyunsaturated fatty acid formation in neonates: effect of gestational age and intrauterine growth.
Pediatr Res.
2000;47:127-135.
15. Pawlosky RJ, Hibbeln JR, Novotny JA, et al. Physiological compartmental analysis of alpha-linolenic acid metabolism in adult humans.
J Lipid Res.
2001;42:1257-1265.
16. Hong S, Gronert K, Devchand PR, et al. Novel docosatrienes and 17S-resolvins generated from docosahexaenoic acid in murine brain, human blood, and glial cells. Autacoids in anti-inflammation.
J Biol Chem.
2003;278:14677-14687.
17.
Kitajka K, Puskas LG, Zvara A, et al. The role of n-3 polyunsaturated fatty acids in brain: modulation of rat brain gene expression by dietary n-3 fatty acids.
Proc Natl Acad Sci USA.
2002;99:2619-2624.
18. Price PT, Nelson CM, Clarke SD. Omega-3 polyunsaturated fatty acid regulation of gene expression.
Curr Opin Lipidol.
2000;11:3-7.
19. Makrides M, Neumann MA, Byard RW, et al. Fatty acid composition of brain, retina, and erythrocytes in breast- and formula-fed infants.
Am J Clin Nutr.
1994;60:189-194.
20. Martinez M. Tissue levels of polyunsaturated fatty acids during early human development.
J Pediatr.
1992;120(suppl):
S129-138.
21. Levitt P. Structural and functional maturation of the developing primate brain.
J Pediatr.
2003;143(suppl):S35-S45.
22. Lozoff B, Wachs TD. Functional correlates of nutritional anemias in infancy and early childhood–child development and behavior. In: Ramakrishnan U, ed.
Nutritional Anemias.
Boca Raton, FL: CRC Press; 2001:69-88.
23. Auestad N, Montalto MB, Hall RT, et al. Visual acuity, erythrocyte fatty acid composition, and growth in term infants fed formulas with long chain polyunsaturated fatty acids for one year. Ross Pediatric Lipid Study.
Pediatr Res.
1997;41:1-10.
24. Jensen CL, Maude M, Anderson RE, et al. Effect of docosahexaenoic acid supplementation of lactating women on the fatty acid composition of breast milk lipids and maternal and infant plasma phospholipids.
Am J Clin Nutr.
2000;71(suppl):S292-S299.
25. Innis SM. Plasma and red blood cell fatty acid values as indexes of essential fatty acids in the developing organs of infants fed with milk or formulas.
J Pediatr.
1992;120(suppl):S78-S86.
26. Balk E, Chung M, Lichtenstein A, et al.
Effects of Omega-3 Fatty Acids on Cardiovascular Risk Factors and Intermediate
Markers of Cardiovascular Disease.
Summary, Evidence Report/Technology Assessment: Number 93. AHRQ Publication
Number 04-E0101-1, March 2004. Rockville, MD: Agency for Healthcare Research and Quality; 2004.
27. Innis SM, Vaghri Z, King DJ. n-6 Docosapentaenoic acid is not a predictor of low docosahexaenoic acid status in Canadian preschool children.
Am J Clin Nutr.
2004;80:768-773.
28. U.S. Department of Health and Human Services & U.S. Environmental Protection Agency. What You Need to Know About
Mercury in Fish and Shellfish.
2004 EPA and FDA Advice for: Women Who Might Become Pregnant, Women Who are
Pregnant, Nursing Mothers, Young Children.
2004. Available at: http://www.cfsan.fda.gov/~dms/admeng3.html. Accessed
April 7, 2004.
29. Bourre JM, Piciotti M, Dumont O, et al. Dietary linoleic acid and polyunsaturated fatty acids in rat brain and other organs.
Minimal requirements of linoleic acid.
Lipids.
1990;25:465-472.
30. Koletzko B. Trans fatty acids may impair biosynthesis of long-chain polyunsaturates and growth in man.
Acta Paediatr.
1992;81:302-306.
31.
Wauben IP, Xing HC, McCutcheon D, et al. Dietary trans fatty acids combined with a marginal essential fatty acid status during the pre- and postnatal periods do not affect growth or brain fatty acids but may alter behavioral development in
B6D2F(2) mice.
J Nutr.
2001;131:1568-1573.
D H A I N T O D D L E R N U T R I T I O N 43