29787,"nona's sweets",17,,,480,http://www.123helpme.com/view.asp?id=79260,2.3,28100,"2016-02-28 04:00:01"
advertisement
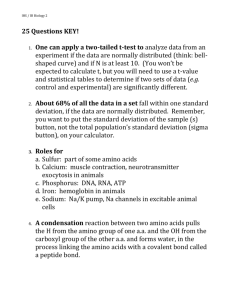
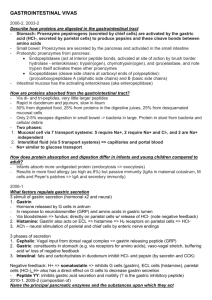
Prof. Dr. Hedef Dhafir El-Yassin 2012 Clinical cases in digestion and absorption: 1. Clinical cases in carbohydrate digestion and absorption: Case 1.1: Deria Voider is a 20-year-old exchange student from Nigeria who has noted gastrointestinal bloating, abdominal cramps, and intermittent diarrhea ever since arriving in the United States 6 months earlier. A careful history shows that these symptoms occur most commonly about 45 minutes to 1 hour after eating breakfast but may occur after other meals as well. Dairy products, not a part of Deria’s diet in Nigeria, were identified as the probable offending agent because her gastrointestinal symptoms disappeared when milk and milk products were eliminated from her diet. Discussion: Lactose intolerance can either be the result of a primary deficiency of lactase production in the small bowel (as is the case for Deria Voider) or it can be secondary to an injury to the intestinal mucosa, where lactase is normally produced. The lactose that is not absorbed is converted by colonic bacteria to lactic acid, methane gas (CH4), and H2 gas. The osmotic effect of the lactose and lactic acid in the bowel lumen is responsible for the diarrhea often seen as part of this syndrome. Similar symptoms can result from sensitivity to milk proteins (milk intolerance) or from the malabsorption of other dietary sugars. In adults suspected of having a lactase deficiency, the diagnosis is usually made inferentially when avoidance of all dairy products results in relief of symptoms and a rechallenge with these foods reproduces the characteristic syndrome. If the results of these measures are equivocal, however, the malabsorption of lactose can be more specifically determined by measuring the H2 content of the patient’s breath after a test dose of lactose has been consumed. Deria Voider’s symptoms were caused by her “new” diet in the country, which included a glass of milk in addition to the milk she used on her cereal with breakfast each morning. Management of lactose intolerance includes a reduction or avoidance of lactosecontaining foods depending on the severity of the deficiency of intestinal lactase. Hard cheeses (e.g.cheddar) are low in lactose and may be tolerated by patients with only moderate lactase deficiency. Yogurt with “live and active cultures” printed on the package contain bacteria that release free lactases when the bacteria are lysed by gastric acid and proteolytic enzymes. The free lactases then digest the lactose. Many adults who have a lactase deficiency develop the ability to ingest small amounts of lactose in dairy products without experiencing symptoms. This adaptation probably involves an increase in the population of colonic bacteria that can cleave lactose and not a recovery or induction of human lactase synthesis. For many individuals, dairy products are the major dietary source of calcium, and their complete elimination from the diet can lead to osteoporosis. 1 Prof. Dr. Hedef Dhafir El-Yassin 2012 Case 1.2: Ann Sulin’s fasting and postprandial blood glucose levels are frequently above the normal range in spite of good compliance with insulin therapy. Her physician has referred her to a dietician skilled in training diabetic patients in the successful application of an appropriate American Diabetes Association diet. As part of the program, Ms. Sulin is asked to incorporate foods containing fiber into her diet, such as whole grains (e.g., wheat, oats, corn), legumes (e.g., peas, beans, lentils), tubers (e.g., potatoes, peanuts), and fruits. Discussion: Poorly controlled diabetic patients such as Ann Sulin frequently have elevations in serum glucose levels (hyperglycemia). This is often attributable to a lack of circulating, active insulin, which will stimulate glucose uptake (through the recruitment of GLUT 4 transporters from the endoplasmic reticulum to the plasma membrane) by the peripheral tissues (heart, muscle, and adipose tissue). Without uptake by these tissues, glucose tends to accumulate within the bloodstream, leading to hyperglycemia. Case 1.3: Nona Melos (no sweets) is a 7-month-old baby girl, the second child born to unrelated parents. Her mother had a healthy, full-term pregnancy, and Nona’s birth weight was normal. She did not respond well to breastfeeding and was changed entirely to a formula based on cow’s milk at 4 weeks. Between 7 and 12 weeks of age, she was admitted to the hospital twice with a history of screaming after feeding but was discharged after observation without a specific diagnosis. Elimination of cow’s milk from her diet did not relieve her symptoms; Nona’s mother reported that the screaming bouts were worse after Nona drank juice and that Nona frequently had gas and a distended abdomen. At 7 months she was still thriving (weight above 97th percentile) with no abnormal findings on physical examination. A stool sample was taken. Discussion: The dietary sugar in fruit juice and other sweets is sucrose, a disaccharide composed of glucose and fructose. . Nona Melos’ symptoms of pain and abdominal distension are caused by an inability to digest sucrose or absorb fructose, which are converted to gas by colonic bacteria. Nona Melos’s stool sample had a pH of 5 and gave a positive test for sugar. The possibility of carbohydrate malabsorption was considered, and a hydrogen breath test was recommended. Nona Melos was given a hydrogen breath test, a test measuring the amount of hydrogen gas released after consuming a test dose of sugar. Her urine tested negative for sugar, suggesting the problem is in digestion or absorption, because only sugars that are absorbed and enter the blood can be found in urine. The basis of the hydrogen breath test is that if a sugar is not absorbed, it is metabolized in the intestinal lumen by bacteria that produce various gases, including hydrogen. 2 Prof. Dr. Hedef Dhafir El-Yassin 2012 2. Clinical cases in protein digestion and absorption: Case 2.1 Sissy Fibrosa, a young child with cystic fibrosis, has had repeated bouts of bronchitis caused by Pseudomonas aeruginosa. With each of these infections, her response to aerosolized antibiotics has been good. However, her malabsorption of food continues, resulting in foul-smelling, glistening, bulky stools. Her growth records show a slow decline. She is now in the 24th percentile for height and the 20th percentile for weight. She is often listless and irritable, and she tires easily. When her pediatrician discovered that her levels of the serum proteins albumin, transferrin, and thyroid hormone binding prealbumin (transthyretin) were low to low-normal (indicating protein malnutrition), Sissy was given enteric-coated microspheres of pancreatic enzymes. Almost immediately, the character of Sissy’s stools became more normal and she began gaining weight. In the next 6 months, her growth curves showed improvement, and she seemed brighter, more active, and less irritable. Discussion: Patients with cystic fibrosis, such as Sissy Fibrosa, have a genetically determined defect in the function of the chloride channels. In the pancreatic secretory ducts, this defect causes inspissation (drying and thickening) of pancreatic exocrine secretions, eventually leading to obstruction of these ducts. One result of this problem is the inability of pancreatic enzymes to enter the intestinal lumen to digest dietary proteins. Sissy Fibrosa’s growth and weight curves were both subnormal until her pediatrician added pancreatic enzyme supplements to her treatment plan. A well noticed improvement in Sissy’s body weight and growth curves was noted within months of the start of this therapy. 3 Prof. Dr. Hedef Dhafir El-Yassin 2012 Case 2.2 For the first few months after a painful episode of renal colic, during which he passed a kidney stone, Cal Kulis had faithfully maintained a high daily fluid intake and had taken the medication required to increase the pH of his urine. Because he has cystinuria, these measures were necessary to increase the solubility of the large amounts of cystine present in his urine and, thereby, to prevent further formation of kidney stones (calculi). With time, however, he became increasingly complacent about his preventive program. After failing to take his medication for a month, he experienced another severe episode of renal colic with grossly bloody urine. Fortunately, he passed the stone spontaneously, after which he vowed to faithfully comply with therapy. His mother heard that some dietary amino acids were not absorbed in patients with cystinuria and asked whether any dietary changes would reduce Cal’s chances of developing additional renal stones. Discussion: Cal Kulis and other patients with cystinuria have a genetically determined defect in the transport of cystine and the basic amino acids, lysine and arginine, across the brush-border membranes of cells in both their small intestine and renal tubules. However, they do not appear to have any symptoms of amino acid deficiency, in part because these amino acids are nonessential amino acids. The most serious problem for these patients is the insolubility of cystine, which can form kidney stones In Hartnup disorder the intestinal and renal transport defect involves the neutral amino acids (monoamine, monocarboxylic acids), including a number of the essential amino acids (isoleucine, leucine, phenylalanine, threonine, tryptophan, and valine) as well as certain nonessential amino acids (alanine, serine, and tyrosine). A reduction in the availability of these essential amino acids would be expected to cause a variety of clinical disorders. Yet children with the Hartnup disorder identified by routine newborn urine screening almost always remain clinically normal. However, some patients with the Hartnup biochemical phenotype eventually develop pellagra-like manifestations, which usually include a photosensitivity rash, ataxia, and neuropsychiatric symptoms. Pellagra results from a dietary deficiency of the vitamin niacin or the essential amino acid tryptophan, which are both precursors for the nicotinamide moiety of NAD and NADP. The only rational treatment of patients having pellagra-like symptoms is the administration of niacin (nicotinic acid) in oral doses. Although the rash, ataxia, and neuropsychiatric manifestations of niacin deficiency may disappear, the hyperaminoaciduria and intestinal transport defect do not respond to this therapy. 4 Prof. Dr. Hedef Dhafir El-Yassin 2012 3. Clinical cases in lipid digestion and absorption: Case 3.1 Will Michael had several episodes of mild back and lower extremity pain over the last year, probably caused by minor sickle cell crises. He then developed severe right upper abdominal pain radiating to his lower right chest and his right flank 36 hours before admission to the emergency room. He states that the pain is not like his usual crisis pain. Intractable vomiting began 12 hours after the onset of these new symptoms. He reports that his urine is the color of iced tea and his stool now has a light clay color. On physical examination, his body temperature is slightly elevated, and his heart rate is rapid. The whites of his eyes (the sclerae) are obviously jaundiced (a yellow discoloration caused by the accumulation of bilirubin pigment). He is exquisitely tender to pressure over his right upper abdomen. The emergency room physician suspects that Michael is not in sickle cell crisis but instead has either acute cholecystitis (gallbladder inflammation) or a gallstone lodged in his common bile duct, causing cholestasis (the inability of the bile from the liver to reach his small intestine). His hemoglobin level was low at 7.6 mg/dL (reference range _12–16) but unchanged from his baseline 3 months earlier. His serum total bilirubin level was 3.2 mg/dL (reference range _ 0.2–1.0), and his direct (conjugated) bilirubin level was 0.9 mg/dL (reference range _0 –0.2). Intravenous fluids were started, he was not allowed to take anything by mouth, a nasogastric tube was passed and placed on constant suction, and symptomatic therapy was started for pain and nausea. When his condition had stabilized, Michael was sent for an ultrasonographic (ultrasound) study of his upper abdomen. Discussion: In patients such as Will Sichel who have severe and recurrent episodes of increased red blood cell destruction (hemolytic anemia), greater than normal amounts of the red cell pigment heme must be processed by the liver and spleen. In these organs, heme (derived from hemoglobin) is degraded to bilirubin, which is excreted by the liver in the bile. If large quantities of bilirubin are presented to the liver as a consequence of acute hemolysis, the capacity of the liver to conjugate it, that is, convert it to the water-soluble bilirubin diglucuronide, can be overwhelmed. As a result, a greater percentage of the bilirubin entering the hepatic biliary ducts in patients with hemolysis is in the less watersoluble forms. In the gallbladder, these relatively insoluble particles tend to precipitate as gallstones. One or more stones may leave the gallbladder through the cystic duct and enter the common bile duct. Most pass harmlessly into the small intestine and are later excreted in the stool. Larger stones, however, may become entrapped in the lumen of the common bile duct, where they cause varying degrees of obstruction to bile flow (cholestasis) with associated ductal spasm, producing pain. If common duct obstruction is severe enough, bilirubin flows back into the venous blood draining from the liver. As a consequence, serum bilirubin levels, particularly the indirect (unconjugated) fraction, increase. Tissues such as the sclerae of the eye take up this pigment, which causes them to become yellow (jaundiced 5 Prof. Dr. Hedef Dhafir El-Yassin 2012 Case 3.2 Al Martini has continued to abuse alcohol and to eat poorly. After a particularly heavy intake of vodka, a steady severe pain began in his upper mid-abdomen. This pain spread to the left upper quadrant and eventually radiated to his mid-back. He began vomiting nonbloody material and was brought to the hospital emergency room with fever, a rapid heart beat, and a mild reduction in blood pressure. On physical examination, he was dehydrated and tender to pressure over the upper abdomen. His vomitus and stool were both negative for occult blood. Blood samples were sent to the laboratory for a variety of hematologic and chemical tests, including a measurement of serum amylase and lipase, digestive enzymes normally secreted from the exocrine pancreas through the pancreatic ducts into the lumen of the small intestine. Discussion: Alcohol excess may produce proteinaceous plugs in the small pancreatic ducts, causing back pressure injury and autodigestion of the pancreatic acinar cells drained by these obstructed channels. This process causes one form of acute pancreatitis. As a result of decreased secretion of pancreatic lipase through the pancreatic ducts and into the lumen of the small intestine, dietary fat was not absorbed at a normal rate, and steatorrhea (fat-rich stools) occurred. If quitting alcohol does not allow adequate recovery of the enzymatic secretory function of the pancreas, Mr. Martini will have to take a commercial preparation of pancreatic enzymes with meals that contain even minimal amounts of fat. Steatorrhea also may be caused by insufficient production or secretion of bile salts. Therefore, Will Sichel might also develop this condition. 6