eprint_4_10346_1010.doc
advertisement

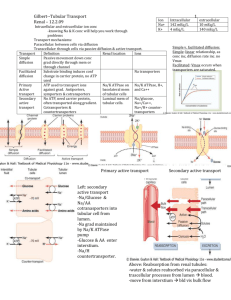
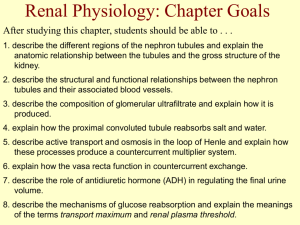
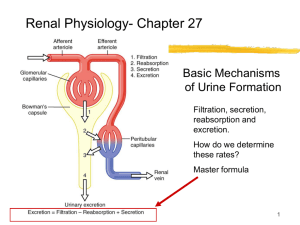
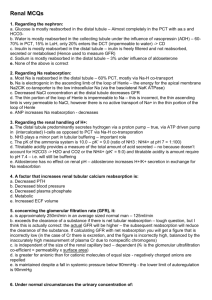
نصير جواد المختار.د Physiology Lecture IX: Regulation of Na+ and Water Reabsorption Na+ are dominant EC cation, thus they exert about (90-95%) osmotic pressure in ECF (in combination with Cl - anion). After Na+ freely filtered at glomerulus, its reabsorption which is active occur in all tubular segment except descending limb of loop of Henle, while HOH reabsorption is by diffusion and dependent on Na+ reabsorption. In proximal tubules by the rate of Na + move out of cell to fluid and achieved by Na+/K+ ATPase pumps in the basolateral membrane of cells. This active transport of Na+ out of cell diminish intracellular Na + concentration compared to luminal concentration. This in turn establish Na+ concentration gradient, thus Na+ diffuses from tubule through brush border to cell. The continuous active transport of Na+ out of cell creates electrical potential (-70 mv) which is an additional factor favours Na + diffusion from tubular lumen to cell. Cl- will be cotransported with Na+ by difference in electrical charge when the concentration of solute decrease in lumen and increase in interstitium. This resulted in concentration difference which promote water osmosis in same direction. In Loop of henle: Reabsorption occur in ascending limb by active/ passive transport but is impermeable to HOH. Therefore Na+ concentration falls to a low level within tubular fluid. In distal convoluted tubule CCT, CD is highly variable with rate controlled by concentration of aldosterone. In presence of large amount of aldosterone all Na+ reabsorbed while in its absence large proportional of Na+ entered distal tubule isn’t reabsorbed passed to urine. Regulation of Aldosterone Secretion: Aldosterone secretion is regulated by rennin angiotensin system and major comp. is juxtaglomerular apparatus composed of 3 types of cells: 1. JG Cells: Located in media of afferent arteriols and they synthesize, store and release rennin enzyme. They serve as baroreceptor and respond to increase in trans????? Pressure gradient between afferent arteriole and interstitium innervated by sympathetic nerve. They serve as volume 1 نصير جواد المختار.د Physiology receptor which monitor renal perfusion pressure and stimulated by hypovolumia decreased renal perfusion pressure. 2. Macula Densa Cells: Located at transition between thick ascending segment of loop of Henle and distal tubule and function as chemoreceptor stimulated by decreased Na+/Cl- load (not innervated). 3. Messangial Cell: Rennin is secreted to blood stream where it combines with rennin substrate- angiotensenogin synthesized in liver to form (AnI). The latter converted in lung by pulmonary endothelial cells to (AnII) by angiotensin converting enzyme. (AnII) has following functions: I. Aldosterone synthesis and secretion. II. Potent vasoconstrictor of renal arteriole at low plasma concentration. How kidney changes aldosterone circulating amount? Increase Na+ intake lead to increase EVF volume, lead to increase arterial pressure. Juxtaglomerular apparatus receive sympathetic innervations when baroreceptor stimulated by increase atrial pressure. They ?????? information to brain that in form JGA via renal nerve to: Decrease rennin output → decrease AnI → decrease AnII → back aldosterone released → decrease NA+ reabsorption and more Na+ excreted. 2