Gilbert_Transport_mechansims_12.2.09
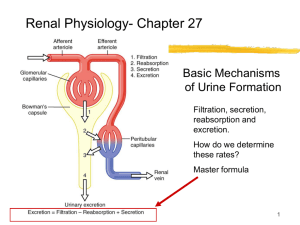
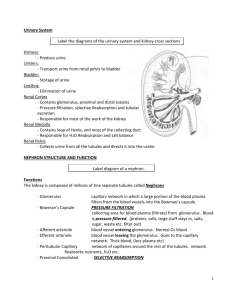
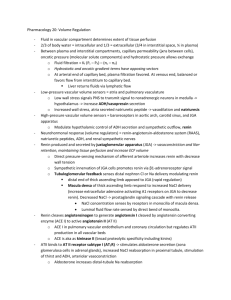
advertisement

Gilbert--Tubular Transport Renal – 12.2.09 Ion Na+ K+ Intracellular and extracellular ion conc -knowing Na & K conc will help you work through problems Transport mechanisms: Paracellular: between cells via diffusion Transcellular: through cells via passive diffusion & active transport. Transport Definition Renal location Ions Simple Passive movement down conc diffusion grad directly through mem or through channel Facilitated Substrate binding induces conf Na transporters diffusion change in carrier protein, no ATP used Primary ATP used to transport ions Na/K ATPase on Na/K ATPase, H+, Active against grad. Antiporters, basolateral mem and Ca++ transport symporters & cotransporters of tubular cells Secondary No ATP, need carrier protein, Luminal mem of Na/glucose, active often transported along gradient. tubular cells. Na+/Ca++, transport Cotransporters & Na+/H+ countercountertransporters transporters Primary active transport Intracellular 142 mEq/L 4 mEq/L 1 extracellular 10 mEq/L 140 mEq/L Simple v. facilitated diffusion: Simple: linear relationship, as conc inc, diffusion rate inc. no Vmax Facilitated: Vmax occurs when transporters are saturated. Secondary active transport Left: secondary active transport -Na/Glucose & Na/AA cotranasporters into tubular cell from lumen. -Na grad maintained by Na/K ATPase pump -Glucose & AA enter interstium. -Na/H countertransporter. Above: Reabsorption from renal tubules: -water & solutes reabsorbed via paracellular & trascellular processes from lumen blood. -move from interstium bld vis bulk flow 2 Gilbert--Tubular Transport Renal – 12.2.09 Transporting solute and water from tubule to capillary (Left) 1: active extrusion of sodium into the interstitium which induces a parallel transport of anions 2: The movement of Na & anions generates an osmotic drive 3. that causes reabsorption of water. 4. Finally, the inc vol in the interstitium alters peritubular Starling forces & induces the bulk flow of water & solute from interstitium into the peritubular capillary Transport Maximum Some substances have a max rate of tubular transport due to saturation of carriers, limited ATP, etc. • Transport Maximum: Once the transport maximum is reached for all nephrons, further inc in tubular load are not reabsorbed; they are excreted. -example: sugar in bld, excess is excreted •Threshold: the tubular load at which transport maximum is exceeded in some nephrons. This is not exactly the same as the transport maximum of the whole kidney because some nephrons have lower transport max’s than others. -Examples: glucose, amino acids, phosphate, sulphate Left: Glucose transport max (Tm) -- good buffering system -Filtration: via passive diffusion (linear, RED) -reabsorption: via facilitated diffusion (Vmax, BLUE) -excretion: what is left in lumen -threshold dif from transport max due to nephron heterogeneity. Conc of solutes in different parts of the tubule depend on relative reabsorption of the solutes compared to water • if water is reabsorbed to a greater extent than the solute, the solute will become more concentrated in the tubule (e.g. creatinine, inulin) • if water is reabsorbed to a lesser extent than the solute, the solute will become less concentrated in the tubule (e.g. glucose, amino acids) Ion Reabsportion: -Na reabsportion occurs mainly at proximal convoluted tubules, some at distal convoluted tubules, none in collecting duct. -Water, chloride, and urea reabsorption are coupled with sodium reabsorption -WHEREVER THE Na GOES, THE WATER WILL FOLLOW. 3 Gilbert--Tubular Transport Renal – 12.2.09 Transport Characteristics of dif portions of the nephron Reabsorbed secreted Prox. Tubule Cl-, Na, HCO3, K, H20, Drugs (penicillin, glucose, amino acids salicylates), bile salts, oxalate, urate, Catecholamines, PAH Loop of Henle: 3 seg listed below: Thin descending LH Very permeable to H2O, moderately permeable to Most solutes including urea and sodium Thin ascending LH Thin Ascending limb not permeable to H2O Thick ascending LH 25% of filtered load! Secretion of H+not + + Reabsorption of Na , Cl , K , permeable to H2O HCO3-, Ca++, Mg++ Early Distal Tubule Active reabsorption of Na+, Not permeable to water Cl-, K+, Mg++ (called diluting segment) • not very permeable to • ~ 5% of filtered load urea NaCl reabsorbed Late Distal Tubule permeablility to H2O depends on ADH -Na, K, Ca, Bicarb • not very permeable to urea -K & H+ Medullary collecting duct permeablility to H2O depends on ADH -Na, urea, bicarb, urea H+ Pharm Notes In cortex, at top of conc grad where everything is isosmotic -loop diuretic hit Na/2Cl/K transporter Hypoosmotic Thiazide Diuretics: - chlorothiazide - hydrochlorothiazide blk Na/Cl cotransporter Contains macula densa: key for tubulargolmerular feedback, Production of renin-ang system to maintain GFR. -Principle cells: aldosterone acts on, secrete K -intercalated cell: respond to ADH, acid/base – secrete H+ Aldosterone antagonists - Spironolactone - Eplerenone -blk Na/K ATPase & Na channel Na+ channel blockers: - Amiloride - Triamterene Prox tubule Left: Prox. Tubule transport charac: -Na & Cl: don’t change relative to plasma cuz of isoosmotic cortex -Creatine: inc cuz filtered but not reabsorbed. -bicarb, glucose & AA dec in lumen cuz reabsorbed. Loop of Henle Gilbert--Tubular Transport Renal – 12.2.09 Collecting Tubules Below: Na, K, Cl transport in thick ascending loop of Henle 4 Medullary collecting duct: Gilbert--Tubular Transport – 12.2.09 Lots of waterRenal transport but tightly reg by ADH. Regulation of Tubular Reabsorption System/force Effect Glomerulotubular -As tubular load inc, so Balance does tubular reabsorption. Reabsorption rate is maintained, amt inc -minimized changes in urine vol as tubular load changes Peritubular Physical -Balance of oncotic & Forces hydrostatic pressures -net reabsorptive pressure ~ 10 mmHg, fluid & solutes to be reabsorbed into the peritubular caps Aldosterone -Inc Na reabs @ principle cells -Inc K secrete @ principle cells -inc H+ secrete @ intercalated cells -inc Aldo secretion: Ang II, K, ACTH, dec Aldo secretion: ANF, inc Na conc Angiotensin II Inc water and Na retention -inc Aldo secretion Directly inc Na reabs ADH Atrial natriuretic horm Parathyroid hormone Sympathetic NS - dec peritubular cap hydrostatic P - inc filtration fraction incs peritubular colloid osmotic P Inc perm to H20 Inc GFR Dec renin, Ang II, Adlo Dec NaCl & H2O reabs Dec ADH secretion & actions Inc NaCl reabs 5 Location Proximal tubule notes Peritubular caps late distal, cortical and medullary collecting tubules •deficiency - Addison’s disease Na+ wasting, hyperkalemia, hypotension • Excess - Conn’s syndrome Na+ retention, hypokalemia, alkalosis, HTN proximal, loop, distal, collecting tubules From constriction of efferent arterioles Blocking Ang II w/ ACEi & Ang II antagonist dec Aldo, dec Na reabs, dec efferent art R, naturesis & diuresis dec BP CD inc H20 reabs dec urine flow & inc urine osmolarity Glomerulus JGA, adrenal cortex Collecting duct (CD) Post pituitary & CD -Secreted by atria in resp to stretch (inc vol) -minimizes bld vol expansion Prox tubule, TAL, DT, 6 Gilbert--Tubular Transport Renal – 12.2.09 CD inc H20 reabs (not TAL cuz imperm) Atrial Pressure (pressure natriuresis) Stim renin release Dec GFR & renal bld flow • Inc peritubular cap hydrostatic pressure • Dec renin & aldo • Inc release of intrarenal natriuretic factors: PG & EDRF Afferent arteriole constriction Peritubular caps Reabsorption by the Peritubular Capillaries Kf = filtration coeffient (leakiness) Colloid onoctic pressure = osmotic forces from proteins. Osmotic pressure = from anything that has a charge. Gilbert--Tubular Transport Renal – 12.2.09 7 As there are inc in Na, your plasma vol inc, CO inc, if you have more vol in the CV system the pressure will inc. The pressure inc until the pressure naturesis mech is activated in kidney. When that occurs it will gradually shift to the left over a couple of days. If the person is salt senstive, the curve will shift right but reach a new steady state. Aldosterone Escape: (Above) Acute phase = excess Na retention as the Na is retained the BP will be inc once the BP maxes out Na excretion will reach a steady state again 8 Gilbert--Tubular Transport Renal – 12.2.09 Practice Questions: Know: •Transport mechanisms: proximal tubule, loop of Henle, distal and collecting tubules • Physiological regulators of tubular transport -Physiological Regulators of Tubular Reabsorption -Factors that Cause Abnormal Increases in Tubular Reabsorption (disordersO Answers: 1. A.1/3 water remains B. 1/8 water remains C. 1/50 water remains 2. Renin tumor: Na reabs 3. Liddle’s syndrome: excessive Na reabs 4. Conn’s Syndrome: Na reabs 5. inappropriate ADH syndrome: water reabsorption