Academic Programme - IOSConference.org
advertisement
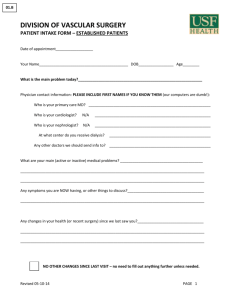
Fifty Third Annual Meeting of the Irish Otorhinolaryngology / Head and Neck Society Sir William Robert Wills Wilde (1815 – 1876) Lough Erne Resort, Enniskillen, Co. Fermanagh Friday 5th & Saturday 6th October 2012 Officers President : Mr. T. O’Dwyer Vice President : Mr. J. G. Toner Secretaries : Mr. R. Adair (Northern) Mr. N. Patil (Southern) Editor of Proceedings : Mr. P. Gormley Treasurer : Ms. Cate Scally Members : Mr. M. Donnelly Mr. E. McNaboe Mr. D. McShane Mr. G. O’Leary Past Presidents T. G. Wilson F. A. McLaughlin R. R. Woods J. McAuliffe Curtin D. Craig Kennedy Hunter M. J. Roberts R. S. McCrea M. O’Brien R. M. Harvey A. Blayney T. Wilmot E. Fenelon H. W. H. Shepperd W. Doyle Kelly A. C. M. L. Miller A. Maguire J. E. T. Byrne H. Burns A. Kerr K. Tobin J. H. A. Black M. A. Walsh D. Adams A. Blayney W. Primrose Wilde Discoursers 1961 1962 1963 1964 1965 1966 1967 1968 1969 1970 1971 1972 1973 1974 1975 1976 1977 1978 1979 1980 1981 1982 1983 1984 1985 1986 1987 1988 1989 1990 1991 1992 1993 1994 1995 1996 1997 1998 1999 2000 2001 2002 2003 2004 2005 2006 2007 2008 2009 2010 2011 Terence Cawthorne Ian Simpson Hall C.P. Wilson Ronald Macbeth W.H. Struben Angell James Michel Portmann Howard House Joseph Ogura J.P. Hood Harold F. Schucknecht Donald F.N. Harrison Stuart Strong Douglas Bryce John Ballantye Claus Jansen Gabriel Tucker L.B.W. Jongkees Robert Pracy George Nager R.B. McDowell R. Wentges Victor Goodhill Douglas Ranger H. Spondalin P. Alberti Tauno Palva Philip Stell Dietrich Plester Arnold G. Maran David Brain William Panjee Tony Bull Richard. Ramsden David Kennedy L. Ryan Ugo Fisch R. Goody E. McKay J. Fredrickson Patrick Gullane William Coman Thomas McDonald Trevor McGill Gilbert Nolst Trenite George Browning Kevin Gibbin Max McCormick Peter Wormald Fred Owens John Watkinson Program Thursday 4th October 1600 - 1900 Registration 1900 - 1940 IOS Council Meeting 2000 - 2130 Buffet Dinner Friday 5th October 0730 - 0850 Registration 0850 - 0900 Welcome by President / Announcements 0900 - 1100 Free Paper Session (Head + Neck) Chairpersons : Barry Devlin + Mark Rafferty 0900 - 0910 Monitoring Treatment Responses In the Node Positive Neck in Patients With Oropharyngeal Squamous Cell Carcinoma Phoebe Roche, James Paul O Neill, Tadgh O Dwyer Mater Hospital OBJECTIVES: Oropharyngeal squamous cell carcinoma accounts for between 15 and 20 % of all head and neck cancers. Approximately 85 % of all oropharyngeal tumors will present with nodal metastases. Over the last decade, there has been a significant rise in its incidence and there is controversy over its management. The aim of this paper, is to review our practise, in monitoring patients with a history of nodal disease due to oropharyngeal primary. METHODS: A five-year audit of all patients treated for oropharyngeal squamous cell carcinoma with nodal disease at the Mater Hospital is presented along with a review of the recent literature. RESULTS: According to the Mater Hospital Head and Neck cancer registry, a total of 94 patients (age range 40 – 82) were diagnosed with, and treated for oropharyngeal cancer in our hospital between July 2007 and July 2012. Both HPV positive and HPV negative tumors were represented within the cohort. CONCLUSION: Our patients are followed by a multidisciplinary team and positron emission tomography PET CT at 12 weeks following their primary therapeutic modality. Patients with residual disease then proceed with salvage surgery. 0910 - 0920 Role of Sestamibi and PTH assay in parathyroid surgery Ramesh Gurunathan 1, Gillian Taylor 2 & Greg McBride 3 1, 2 - Registrars in ENT; 3 - Consultant ENT Surgeon Altnagelvin Hospital, Londonderry Background: Parathyroid surgery for hyperparathyroidism has moved from traditional four gland exploration to minimally invasive procedure with advent of better imaging tools, intraoperative PTH monitoring and endoscopic techniques. In our hospital parathyroid operation is accomplished with preoperative Sestamibi and serum PTH monitoring at D1 post-op. Intra-operative PTH assay is done only in selected patients. Aim: 1. Analyse the outcome of parathyroid surgery at our Hospital 2. To correlate pre-operative Sestamibi localisation of adenoma with operative findings Method: Retrospective chart review of 32 patients had parathyroid operations from 2009 to 2012. Results: Majority of referrals came through GP and seen at Joint Endocrinology & ENT clinic but occasional referrals from renal, urology, orthopaedics and surgical admissions. Half presented with incidental hypercalcemia and other half had varied clinical presentations like calculi, renal failure, fractures, fatigue, dehydration, acute abdomen etc. Majority (24/32) were females. Age ranged from 22 to 88 with mean of 58. Average operative time was 50 minutes with incision length from 2.5 to 4 cms. Two patients needed 2nd exploration. Postoperative PTH and calcium levels returned to normal in 31/32 patients. Of 32 patients, sestamibi localisation was positive in 20 patients (63%) and correlated 100% with surgical findings. In patients with negative scan, 4 gland explorations were done. Inferior gland pathology is found in two thirds with left inferior in majority. Conclusion: In our view, a preoperative Sestamibi scan is sufficient in majority of patients. 4 gland explorations with intraoperative PTH assay are useful in selective patients with negative scan. 0920 - 0930 Chemoradiation in Elderly Patients with Locally Advanced Head and Neck Cancer: A Population-Based Analysis of Treatment Patterns and Adverse Events Caitriona B. O’Neill, James P. O’Neill, Shrujal S. Baxi, Coral L. Atoria, Martin C. Henman, Eric J. Sherman, Nancy X. Lee, Elena B. Elkin Objective: Concurrent chemoradiation (CTRT) is a standard treatment for patients with locally advanced squamous cell carcinoma of the head and neck cancer (LAHNSCC). Our objectives were to characterize patterns of CTRT use, identify trends in the selection of concurrent chemotherapy, and to assess the nature and frequency of hospitalizations for acute treatment-related adverse events in older patients with LAHNSCC. Methods: Using SEER cancer registry data linked with Medicare claims, we identified patients aged 66 years or older with LAHNSCC diagnosed 1999-2007. We identified trends in CTRT use and the use of specific chemotherapeutic agents. Hospitalizations or emergency room (ER) visits for chemotherapy-related adverse effects were also evaluated. Results: 4,939 LAHNSCC patients were identified, of whom 1,086 (22%) received CTRT. Over time there was a significant increase in the proportion treated with CTRT (p<0.0001). The proportion of patients receiving cetuximab increased 42% in the three year period, 20052007. Sixty-three percent of CTRT patients had a hospital admission or ER visit for an acute treatment-related toxicity and 12% of these patients died in hospital. Conclusions: Although CTRT use is increasing in older patients, acute treatment-related admissions are substantial. Treatment selection is complex and must look beyond chronologic age and consider individual patient factors, such as functional status and personal preference, as well as institutional factors, patient resources, support services and costs. 0930 - 0940 Developing an Airway Alert System (AAS) for post-operative head and neck patients T. Ashfield 1, D. Chatterjee 2, B. Shephard 2, I. Ahmad 2, S. Tricklebank 2 & R. Oakley 1 Departments of ENT, head & neck surgery 1 and anaethetics 2 Guy’s and St. Thomas’ NHS Foundation Trust, London, UK Objective The Fourth National Audit Project of the Difficult Airway Society (NAP4) demonstrated that post-operative major head and neck surgery patients were the group at greatest risk of acute airway events. Improvements in identification of, and planning management for difficult airways were key recommendations. Audit of practice within our own unit confirmed these national observations, highlighting the need for improvement. We developed the AAS to improve identification and planning for difficult airways in post-operative head and neck patients. Methods AAS is divided into three phases; risk stratification, planning and continuing review. Key airway safety issues are reviewed and recorded by the anaesthetic, surgical and critical care teams, and patients deemed high risk are placed into one of three groups, according to the nature of the anticipated difficulty. A daily checklist is employed to ensure that the airway plan is current and specified equipment is at the bedside. The system also triggers precautions that remain in place until it is deemed appropriate to 'de-escalate'. Results Current understanding and confidence in difficult airway management amongst ICU staff was poor prior to introduction. AAS is now in place and we aim to improve this situation and ultimately improve patient safety. Conclusions Practical, airway skills whilst central to managing a difficult airway are only successful in concert with clear strategy. This system places clear plans at the bedside that are reviewed daily. We have shown that AAS is deliverable, easy to use, and is likely to patient safety in this high risk group. 0940 - 0950 GENE MUTATION ANALYSIS OF NASAL MUCOSAL MALIGNANT MELANOMAS M Moran, AP Kelly, WJ Primrose, MA Catherwood, JA James Objectives: Correlation of pathological characteristics of nasal melanomas with clinical data, in order to investigate a role for gene mutation analysis as a prognostic biomarker for this tumour group. With nasal melanomas it is more difficult to assess the widely accepted grading systems such as Clark level of invasion or surface ulceration, which are used in cutaneous melanomas. Methods: Patients with a diagnosis of nasal malignant melanoma were identified for a ten-year period between 2000 and 2010. Results: The group of patients identified comprised 8 males and 9 females, with a mean age at diagnosis of 69.1 years. Histopathological sections were reviewed for these patients, in particular the immunohistochemistry analysis for markers such as S100, HMB-45 and Melanin-A. In addition, the samples underwent additional molecular tests for BRAF genetic mutations, on the basis that these mutations have been implicated as prognostic indicators in other (cutaneous) melanomas. 23.5% of the patients had BRAF mutations detected. Conclusions: Nasal malignant melanoma is a disease entity that is difficult to treat successfully, and patients often undergo a combination of surgery and chemoradiotherapy in an attempt to control tumour growth and metastasis. This study illustrates the heterogeneity of disease within a cohort of patients with nasal melanoma, and it is hypothesised that a stratified medicine approach to treatment of mucosal melanomas such as these could be enhanced by greater understanding of genes and pathways implicated in the development and spread of melanoma. The genetic mutation analysis for this subset will be correlated with clinical outcomes including overall survival. 0950 - 1000 PREVALENCE OF MULTIPLE SYNCHRONOUS OR METACHRONOUS PRIMARY SQUAMOUS CELL CARCINOMA OF THE UPPER AERODIGESTIVE TRACT J Kulasegarah, C Timon Objective The elevated risk of second primary malignancy (SPM) in patients with head and neck squamous cell carcinoma (HNSCC) is well established. Despite the advances in locoregional control achieved by modern surgery and chemoradiation, survival with HNSCC has not meaningfully improved, in part due to continuing risk of development of SPMs in these patients. We aim to determine the prevalence of SPM over a period of 12 years and also to explore the role of HPV in lesions of the head and neck. Methods A retrospective study of patients diagnosed with HNSCC between January 2000 and Jun 2012 was conducted in St. James’s Hospital and Royal Victoria Eye and Ear Hospital. We aim to perform p16 immunohistochemistry, HPV DNA extraction and genotyping on all histological samples in the future. Results We identified 60 patients over a period of about 12 years (2000 – 2012). 10 females and 50 males between the ages of 36 to 78 (mean 59) were reviewed. Among them, there were 17 pts with synchronous tumours and 43 pts with metachronous tumours. We had 10 pts with SPM in the lung, 2pt in the oesophagus and 48pts within the head and neck region. Among the 60pts with SPM, we had 10 patients with a third primary malignancy and 1 pt with a fourth primary malignancy. Conclusion No comprehensive data have been reported on the risk of SPM among HPV-positive and HPV-negative HNSCC, although Licitra et al observed a non-significant trend toward lower SPM risk in patients with HPV-positive disease. 1000 - 1010 MOLECULAR PREDICTORS SHOULD BE PART OF HEAD & NECK CANCER PROTOCOL? Mohammad Habibullah Khan, Michael Walsh OBJECTIVE: The accepted universal method of staging head and neck cancer has been the TNM staging system. The main deficiency of that system is that it does not take into account the biological markers of the tumour. Molecular staging is now part of the accepted protocol in breast, lung and colon cancer staging. We propose that molecular predictors for example - P53 and EGFR should be part of head and neck cancer protocol. METHODS: We have undertaken a retrospective study of a cohort of T2 laryngeal SCC patients who had failed primary chemotherapy and radiation treatment. They all showed recurrence with the necessity for total laryngectomies. Biopsy specimens were analysed for molecular and genetic markers. RESULTS: These will be discussed at meeting. CONCLUSIONS: Although TNM classification will retain its significance, it is now becoming possible by using molecular markers to acquire biological information about host and tumour and eventually to optimise the choice of treatment. 1010 - 1020 An Audit Comparing FNAC & Core Biopsy in the Management of the Thyroid Nodule JM Adams, M Korda OBJECTIVE British thyroid association 2007 thyroid cancer guidelines suggest FNAC as the first line investigation of choice in the assessment of thyroid lumps/goitre. Core biopsy is often used as a second line tissue sampling technique when FNAC is inadquate or indeterminate. We aimed to compare the two techniques as practiced in our trust with respect to rate of sample inadequacy and/or insufficiency. METHODS A retrospective case review was performed of all thyroid tissue sampling procedures trust-wide over a 6 month period. Data retrieved included patient demographics, type and number of tissue sampling technique, specialty & seniority of performer, results of each, further steps in management, and eventual surgical specimen in those patient proceeding to surgery. The rates of insufficient & inadequate samples were calculated. RESULTS A total of 106 thyroid tissue sampling procedures in 86 patients were undertaken over the 6 month period out-lined, of which were 77 FNAC & 29 core biopsies. There were no complications recorded. The overall rate of Thy1 FNAC (excluding Thy1c) was 26% (20/77). This dropped to 18.5% (10.54) for USS guided FNAC. For core biopsy, the inadequate/insufficient rate was 6.9% (2/29). CONCLUSION Our data suggest that USS guided core biopsy of thyroid returns significantly lower rates of inadequate/insufficient samples. Cost benefit analysis would be required to determine if USS guided core biopsy may be a more appropriate first line investigation. 1020 - 1030 Risk factors for salivary fistula after total laryngectomy Basheeth.N, Sheahan.P, O’Leary.G Objectives To evaluate risk factors for development of pharyngocutaneous fistula after total laryngectomy in patients with squamous cell carcinoma of the larynx. Methods Retrospective chart review of patients undergoing total laryngectomy for squamous cell carcinoma of larynx between 1996-2011 in Cork Head and Neck Cancer Centre. Patients with pharyngeal primaries or undergoing total pharygectomy and / or oesophagectomy were excluded. Results Eighty-four patients underwent total laryngectomy during the study period. 13 patients with hypopharynx primaries were excluded. Of the remaining 71 patients, 27 underwent primary total laryngectomy, and 44 underwent salvage laryngectomy after failed radiotherapy (31) or chemoradiotheray (13). 18 (25%) of patients developed a salivary fistula. The incidence of fistula was 11.1% (3/27) in the primary laryngectomy group, and 34.1% (15/44) in the salvage laryngectomy group (p=0.047). Among patients undergoing salvage laryngectomy, the interval between completion of radiation and total laryngectomy was significantly lower in patients developing fistula than those who did not (8.1 months versus 22.6 months, p=0.01). The likelihood of fistula was not significantly affected by radiation dose (p=0.49); chemotherapy concurrent with radiation (p=0.32); pre-operative tracheostomy (p=0.72); performance of primary tracheo-oesophageal puncture (p=0.32); performance of simultaneous bilateral neck dissection (p=0.35); or use of pectoralis major myogenous flap (p=1.0). Conclusion The risk of pharyngocutaneous fistula is higher in salvage laryngectomy than in primary laryngectomy. The interval between completion of radiotherapy and total laryngectomy appears to be a significant risk factor for development of pharyngocutaneous fistula in salvage cases. 1030 - 1040 MINIMALLY INVASIVE PARATHYROIDECTOMY PARATHYROID ADENOMA CWP Kelly, CY Eng, MS Quraishi FOR Objective: Parathyroid surgery is the acceptable definitive treatment for primary hyperparathyroidism (pHPT) due to parathyroid adenoma. Minimally Invasive Parathyroidectomy (MIP) has an excellent cure rate and minimal morbidity. We aim to demonstrate the safety, efficacy and subjective patient satisfaction of MIP and investigate the accuracy of pre-operative radiological localisation in relation to operative findings. Methods: A retrospective case-note review of patients who underwent MIP for pHPT due to solitary parathyroid adenoma from April 2006 to October 2011 was performed. All patients were initially investigated by an endocrinologist to confirm pHPT with pre-operative localisation imaging using ultrasound scan (USS) and 99mTc-sestamibi (MIBI). Open mini-incision parathyroidectomy (O-MIP) with intra-operative frozen section was performed in our centre. Results: One hundred and forty three patients were included with an average age of 62.3 years. Pre-operative USS and MIBI scans were concordant in 69% of cases. In combined modality (USS and MIBI), localisation was 94.8% There was 95.5% identification of parathyroid tissue confirmed by intra-operative frozen section.. Ninety percent of patients were treated as a day case. The overall mean operative time was 66 minutes. The mean pre-operative calcium level was 2.98 mmol/l and the short-to-medium term mean calcium level was 2.49 (Paired t-test, p=0.000). There was no recurrent laryngeal nerve injury or other significant complication. Conclusion: MIP confers significant advantages over the traditional gold standard treatment of bilateral neck exploration. Accurate localisation is the key to successful MIP. In experienced hands, ultrasound and MIBI may be the only pre-operative investigations required for accurate localisation. 1040 - 1050 Adult Recurrent Laryngeal Papillomatosis Fei Tan, John Russell Objective: Recurrent laryngeal papillomatosis (RLP) is a chronic disease of viral etiology that occurs in both children and adults. The ultimate goal of surgical therapy is to maintain a safe airway while avoiding excessive scarring and maintaining useful vocal cord function. No single type of therapy has been consistently effective in eradicating RLP. Strides are being made in learning more about the natural history of this disease. This audit reviews current management of RLP in St Vincent’s University Hospital (SVUH). Methods: A retrospective study confined to 16 patients who first attended SVUH ENT OPD between 01 Jan 2003 and 20 July 2012 with a histological diagnosis of laryngeal papillomatosis. Derkay’s scoring system with both clinical and anatomical components was used to evaluate the severity of patient’s RLP throughout their management and follow up in SVUH. A time curve of Derkay’s score was generated for every patient. Results: Intra- and inter-patient variability are observed. This is demonstrated on both qualitative time curves and quantitative average intervals for surgeries (from 6.4 weeks to 5.3 years). Female patients have much younger onset than male patients. 92% patients were happy with their overall voice quality at the end of the audit. No malignant transformation is discovered. Conclusions: Each RLP patient has a unique time pattern of disease growth, which mandates a customized management plan.Our treatment is mainly improving patient’s voice and function rather than for airway urgency.Derkay’s scoring system is helpful in planning treatment. Information from this audit is useful in consenting for surgery. 1050 - 1100 The ‘Unknown Primary’ and the impact of human papilloma virus in metastatic squamous cell carcinoma lymph nodes. James Paul O'Neill, Andrea Wang, Ronald Ghossein*, Luc Morris, Snehal Patel, Jatin Shah, Dennis Kraus** * The Department of Pathology, Memorial Sloan Kettering Cancer Center, New York, USA ** The Department of Head and Neck Surgery, North Shore-LIJ Health System Objective: This analysis investigated possible associations between HPV status, smoking history and survival outcome in patients with neck metastasis and carcinoma of unknown primary. Methods: Carcinoma of unknown origin diagnosed from patients between 2002 and 2008 within MSKCC who had formalin-fixed and paraffin-embedded metastatic lymph node samples from modified radical neck dissections. HPV fluorescence in situ hybridization (FISH) and p16 immunohistochemistry (p16 IHC) were performed. Results were compared with survival, age, race, gender, tobacco use, alcohol use, and nodal stage. Results: Over 50% of patients ‘unknown’ primary appears to be of oropharyngeal origin. Overall survival appeared to be superior in patients with <10 pack-years smoking history and HPV+/p16+ disease. Conclusions: The 'Unknown Primary' is a misnomer and more correctly termed the 'Undiscovered Primary'. Smoking status should be considered as a prognostic factor in patients with, along with HPV DNA status. 1100 - 1130 Coffee Break 1130 - 1300 Free Paper Session (Rhinology) Chairpersons : Brendan Hanna + Kieran O’Driscoll 1130 – 1140 Endoscopic Sphenopalatine Artery Ligation – a four year experience at one institution Eadaoin O’Cathain, Patrick Sheahan South Infirmary Victoria University Hospital, Cork OBJECTIVE Epistaxis accounts for a large proportion of emergencies seen by ENT specialists on-call. Here we discuss our experience of endoscopic sphenopalatine artery (SPA) ligation for control over recalcitrant epistaxis over the last four years. METHODS Retrospective review of case notes of patients who underwent SPA ligation between October 2008 and September 2012. RESULTS 27 patients underwent SPA ligation during the study period. 56% had medical comorbidity. 26% were on anticoagulants. Three quarters of patients had been packed multiple times prior to surgery. Seven patients underwent concomitant septoplasty at the time of SPA ligation. One patient underwent simultaneous anterior ethmoid artery ligation. The SPA was controlled by electrocautery in 11% of cases, and by surgical clips in 89%. In 4 (15%) cases, the nose was packed at the end of surgery. 5 (18.5%) patients were re-packed after surgery with Merocel packs due to persistent oozing. One patient returned to theatre for anterior ethmoidal and internal maxillary artery ligation. The success rate of SPA ligation was 78% (21/27). The average hospital stay was 3 days. 9.5% of patients had medical complications that required a longer hospital stay. CONCLUSIONS SPA ligation is an effective procedure for control of recalcitrant epistaxis, and should be considered early in the management of epistaxis to avoid morbidity from repeated nasal packing. 1140 - 1150 THE USE OF CT IN MANAGEMENT OF SINUS DISEASE; DIFFERENCES BETWEEN SPECIALITIES. C O’Rourke, S Ryan, A Rehman, JE Fenton Objective: The management of chronic rhinosinusitis has traditionally been the preserve of Otolaryngologists but recently there has been an anecdotal shift in this concept with an increasing contribution from respiratory physicians. The aim of this study is to compare the indications, results and outcomes of patients undergoing investigation of paranasal sinus disease with computed tomography (CT) requested by the two separate specialities. Methods: This study was a retrospective analysis of 80 CT sinus scan reports over a two year period, which were ordered by otolaryngology (Group 1) and pulmonary (Group 2). Results: They were 50 female and 30 male, a ratio of 1.7:1. The most common indicators for CT from group one were chronic sinusitis (n=16; 40%), nasal polyps (n=10; 25%) and rhinorrhea (n=6; 15%). versus rhinorrhea (n=16; 40%), persistent cough with post-nasal drip (PND) (n=12; 30%) and recurrent respiratory tract infections (n=12; 30%) in group 2. There was a significantly higher positive finding rate on CT sinus ordered by otolaryngologists (90% v 70%; p=0.023). Group 1 also showed a significant difference in positive findings that were directly related to indication (78% v 63%; p=0.043). The mean Lund & Mackay score for group 1 was significantly higher than that of group 2 (8 v 4; p=0.0026) Conclusion: Our results show that there were significantly higher positive CT findings, consistent with indicators used for the study, when ordered by otolaryngologists. CT may be an overused diagnosis tool for management of sinus disease by Pulmonary Rhinologists 1150 - 1200 SEPTAL SURGERY - THE FIRST DECADE OF SIMULATION; DO TRAINEES FEEL APPROPRIATELY TRAINED? S Gupta BSc MBBS MRCS, P S Phillips FRCS, F Salim, C Hopkins FRCS, R Oakley FDSRCS FRCS (Orl-HNS) PG Cert Med Objectives The proportion of trainees in training reporting feeling appropriately trained when performing their first solo septoplasty, a core ENT procedure, in 2001 were compared with those in 2011. The changes in the use of simulated surgery and other training tools and their impact on the level of trainees feeling appropriately trained were analysed. Methods A postal questionnaire (sent to all ENT trainees in 2001) was circulated to all ENT registrars training in the UK in 2011 asking whether they felt appropriately trained before their first solo septoplasty, and what training tools they had been exposed to to simulate this operation prior to performing it. Results Of 337 trainees, 222 responded (65%) as compared to 167 of 223 (74.9%) in 2001. Of these, 173 trainees had been trained solely in the UK. 105 of these (60.7%) felt appropriately trained when performing their first septoplasty. Exposure to training courses, cadaveric dissections and endoscopic septoplasties had increased since 2001. There was a significant association between feeling appropriately trained and being trained by a rhinologist (P<0.0001), being trained in steps (P<0.0001), attending a course (P=0.0076), seeing or doing the dissection on a cadaver (P=0.0044, P=0.0076), and seeing flaps raised endoscopically (P=0.0003). Watching septoplasty internet videos and dissecting biological models was not significantly associated with feeling appropriately trained. Conclusions The use of tools simulating septal surgery has become more widespread over the last decade. The number of trainees reporting feeling inadequately trained when performing this core ENT operation for the first time remains disappointingly high. 1200 - 1210 ANTERIOR SKULL BASE TUMOURS : OUR EXPERIENCE Mohammad Habibullah Khan, Peter D Lacy OBJECTIVE: Anterior craniofacial resection has become a standard procedure for management of lesions of the anterior skull base. During the last few years, modifications of the classic anterior craniofacial resection have been reported. With the introduction of endoscopic sinus techniques and instrumentation, surgeons have begun to use endoscopic approaches for management of anterior skull base lesions. METHOD: A retrospective study of patients with endonasal and skull base tumours treated in our department with endoscopic technique. RESULTS: All the patients who underwent endoscopic approach for skull base tumour, had a short hospital stay, no external scars, speedy recovery, a quick return to their activities and no evidence of recurrence, on their surveillance so far. CONCLUSION: We propose that endoscopic approach to skull base tumours is safe and this strategy facilitates superior visualization, avoids craniofacial incisions, and preserves local structures. Although we do not consider this approach a replacement for the traditional anterior craniofacial resection, it is an important adjunct in the skull base surgeon's armamentarium. 1210 - 1220 Nasal Septal Perforation Repair: One Surgeon's experience. A. O'Kane, A. Kelly, D. McCaul, S. Hall Objective Surgical management of septal perforation is considered difficult. The procedure can be technically challenging with a relatively poor success rate. Numerous surgical techniques are described in the literature but no standardized surgical protocol has been established. We present one surgeon’s experience of septal perforation repair over a 10-year period. Method We performed a retrospective study of 52 patients with nasal septal perforations who underwent surgical repair between April 2002 - April 2012. These were carried out by a single surgeon, in a single unit. Aetiological factors, patient symptoms and perforation size were recorded. Postoperative results were evaluated. Results Of the 52 patients who underwent surgery 39 had complete follow-up and of these 88 % were found to have a successful repair. The followup period varied from a minimum of 2 weeks to a maximum of just under 3 years with a mean follow up period of 7 months. Best results were seen with a 5-layer closure, including an interposition cartilage graft. No significant complications resulted from surgery. Conclusion This is one of the largest single centre studies of surgical septal perforation repair performed. We describe a technique which is proven reliable and with a high success rate. 1220 - 1230 Nasal Melanoma Pathology Reporting: Left in the Dark? Andrew Kelly, Mr Michael Moran (BHSCT and Queen’s University Belfast), Jacqueline A James (BHSCT and Queen’s University Belfast) OBJECTIVES To audit the suitability of the current Royal College of Pathologists minimum dataset for the histopathological reporting of common skin cancers document for mucosal melanomas. METHODS Patients with a diagnosis of nasal malignant melanoma were identified for a ten-year period between 2000 and 2010. The histopathology reports were analysed to assess their compliance with the published Royal College of Pathologists minimum dataset for malignant melanomas. Where possible, the report for the resection specimen was used, as it was regarded that this form provided the most comprehensive account of the tumour characteristics. RESULTS 16 patients were identified who had a diagnosis of new or recurrent nasal mucosal melanoma since the year 2000. All available histopathology reports were reviewed for these patients, which were compiled by one of five consultant pathologists, with joint reporting in some cases. None of the reports included all of the criteria recommended in the minimum dataset for the reporting of malignant melanoma. CONCLUSIONS Nasal mucosal melanoma is a rare but important disease entity with notably poor clinical outcomes. Specific aspects of the malignant melanoma minimum dataset are inappropriate for the assessment of mucosal tumours, and the results highlight a potential benefit of having a minimum dataset specific to mucosal melanomas. 1230 - 1240 The Beaumont Hospital experience of the endoscopic endonasal transsphenoidal approach to the sellar region for the resection of pituitary lesions. Mr. Tom Moran, Mr. Peter Lacy, Mr. Donncha O’ Brien Objective As a modality for the treatment of pituitary tumours, there have been numerous refinements to the surgical approach. Pituitary surgery has been revolutionized by the introduction of the endoscope and minimally invasive surgery to the pituitary gland.This study aims to compile and evaluate the outcomes of all of the minimally invasive pituitary surgery procedures performed at our institution. Methods This is a retrospective evaluation of all 80 patients who have undergone transsphenoidal hypophysectomy under the combined care of the ENT and Neurosurgical departments of Beaumont hospital. Patient demographics, the characteristics of the pituitary lesions and the intraoperative and postoperative complications were compiled and discussed. Results 78 patients operated on over 4 years, 67% had total clearance, 24% had subtotal clearance and 4.8 had partial clearance. 3 complications, 3.5 days post op inpatient stay. This compares favourably with similar international studies. Conclusion The endoscopic endonasal transsphenoidal approach to the sellar region for resection of pituitary lesions is a safe procedure in experienced hands. A coordinated team approach drawing on the expertise of both the endoscopic rhinologist and the neurosurgeon is optimal to achieve the best outcome for the patient. 1240 - 1250 PATIENT SATISFACTION FOLLOWING MANIPULATION UNDER ANAESTHETIC FOR NASAL FRACTURES N Foden, C Igwe, N Mehta, T Joseph OBJECTIVE Nasal fractures are seen commonly in ENT urgent referral and outpatient clinics. Closed reduction or manipulation under anaesthetic (MUA) of a fractured nose is performed for functional or cosmetic reasons. We sought to ascertain patient satisfaction following MUA and determine the likelihood that further surgery would be required. METHODS A retrospective review of all adult patients who underwent MUA nose for nasal fractures at a single centre over a one-year period (April 2011-March 2012) was undertaken. A structured interview was carried out by telephone by a single interviewer. RESULTS 97 patients underwent MUA of a fractured nose over the period. Interviews were successfully performed with 68 (70%) patients. 68 (100%) indicated a cosmetic reason for undergoing MUA whilst 49 (72%) also reported functional reasons. 13 (19%) reported no improvement in cosmesis following the procedure and 18 (37%) were dissatisfied with their functional outcome. 33 (68%) would consider further surgery, of which 18 (26%) had already sought further advice regarding this. CONCLUSIONS Although MUA for a fractured nose is an acceptable treatment in the first instance we found a number of patients to be dissatisfied. A substantial number would consider revision surgery. This has important consequences for funding in an economic environment where access to a number of procedures, including septorhinoplasty, are being scaled back. It is essential that all patients undergoing MUA following a nasal fracture are informed that the procedure may not result in a favourable outcome and that revision surgery may be required at a later stage. 1250 - 1300 ADENOIDECTOMY: ASSESSING THE TECHNIQUES AND COMPLICATIONS R Caffrey, A McGreevy, C Jackson, C Scally INDICATIONS, Objectives Adenoidectomy is a common surgical procedure in children and currently there are no national guidelines on its indications. We audited adenoidectomy practice in our local unit, which included indications, method and complications. Methods Retrospective case note review of patients listed for adenoidectomy over a one year period in a district general hospital. Results 178 patients were included, of whom 134 (75.3%) underwent adenoidectomy. The majority (127) (94.8%) performed by curettage. The commonest presenting complaint was recurrent tonsillitis, and in 28 patients this was the only documented symptom. This was followed by glue ear symptoms, nasal symptoms, snoring and various others. The overall complication rate was 6.7%, with adenoidal bleeding occurring in one patient (0.7%). Conclusion Adenoidectomy is a frequently performed procedure with a low complication rate. This study does highlight a varied approach to indications for adenoidectomy. We present our adenoidectomy guidelines, which we hope will improve the consistency of patient care. 1300 - 1400 Lunch 1400 - 1420 Annual General Meeting 1420 - 1530 CME - Frontiers in endoscopy Chairpersons : Robin Adair + Nash Patil Sinus endoscope optics research do you know where you are looking? - Paul White An update on sialendoscopy - Aongus Curran Challenges for the rhinologist and skull base surgeon - Brendan Hanna 1530 - 1600 Coffee Break (Poster Adjudication - Cate Scally + Marcus Choo) 1600 - 1700 Free Paper Session (Otology) Chairpersons : Ted McNaboe + Mary Bresnihan 1600 - 1610 MASTOID SURGERY IN AN ONLY OR BETTER HEARING EAR M. Sadadcharam, R. McConn-Walsh Objective The patient with cholesteatoma in an only or better hearing ear presents a management dilemma. The aim of surgery is to remove disease entirely and preserve or indeed improve hearing Methods This was undertaken as a retrospective study in conducted in a university-based tertiary referral centre. Our experience with surgical management of twenty patients with cholesteatoma in an only or better hearing ear is presented. The location and extent of cholesteatoma, the type of operation performed, and post-operative hearing results are presented Results Throughout our series, there was no documented loss of bone conduction thresholds and the hearing in all patients was either preserved or improved Conclusions The present series confirms that hearing can be preserved or indeed improved in patients undergoing mastoid surgery in an only or better hearing ear. This should be undertaken in a tertiary referral centre 1610 - 1620 OUTCOMES OF OSSICULOPLASTY IN THE PAEDIATRIC POPULATION TS Ahmed, N Seymour, H Daya OBJECTIVE Although most ossiculoplasties are performed in adults, the procedure is occasionally performed in children. Ossiculoplasty is considered successful if useful hearing is restored. This can be determined both subjectively and objectively. This study aims to investigate clinical outcomes following paediatric ossiculoplasty and identify factors predicting hearing results. METHODS All children undergoing ossiculoplasty between 2001 and 2011 at our hospital were identified from clinical coding databases. A retrospective chart review was performed and data including operative findings, type of prosthesis used and pre and post-operative pure tone audiometric thresholds were extracted. RESULTS Twenty-two children (mean age 10.8, range 3-18) underwent 28 ossiculoplasty procedures. The majority had undergone treatment for cholesteatoma. Thirteen individuals were fitted with a total ossicular replacement prosthesis (TORP) and 9 were fitted with a partial ossicular replacement prosthesis (PORP). Seventeen ossiculoplasties (60.7%) resulted in hearing improvement with a mean of 5.5 dB (SD 14.1 dB): in 15 (89%) this improvement was deemed to be ‘useful’ as assessed with the Glasgow benefit plot. Three ossiculoplasties (10.7%) resulted in no hearing change and 8 procedures (28.6%) resulted in audiometric threshold worsening, of which recurrent cholesteatoma was present in 4 cases. CONCLUSIONS Ossicular reconstruction following tympanomastoid surgery is helpful in improving hearing outcomes. Patients undergoing reconstruction with a PORP, where the stapes suprastructure was preserved, were more likely to have an improvement. There is also some association between cholesteatoma recurrence and poorer hearing outcomes in this series: these patients were more likely to require TORP prostheses and undergo revision ossiculoplasty. 1620 - 1630 The development of an accelerometer based biofeedback device for the management of BPPV F O’Duffy and T O’ Connor 1, P Breen2, D O’ Keefe1, G O’ Laighin2. Keogh I. J.1 1. Academic Department of Oto-Rhino-Laryngology, Head & Neck Surgery, National University of Ireland, Galway, Ireland. 2. School of Engineering & Informatics, National University of Ireland Galway, University Road, Galway, Ireland. Background: The management of posterior semicircular canal Benign Paroxysmal Positional Vertigo (BPPV) has been revolutionised by the Epley manoeuvre. This manoeuvre provides immediate relief from symptoms of BPPV in up to 90% cases. However, many cases still relapse, requiring repeated manoeuvres. It is our view that there is potential to develop a head worn accelerometer based bio feedback device for the management of BPPV. The aim of our study was twofold. Firstly to develop and modify, using existing accelerometer framework, a device for the measurement of real-time angular changes which occur during vestibular manoeuvres, Head Position Recording Device (HPRD). Secondly, to compare using the HPRD the angular accuracy obtained in performing a Clinician guided Epley manoeuvre against the angular accuracy obtained by using a home treatment device “Dizzy-Fix”. Study Design: The accelerometer device chosen as the basic framework for the development of the HPRD was the SHIMMER™, a wearable, wireless health sensing platform. The SHIMMER™ device can record and transmit physiological and kinematic data in real-time. Software used for data collection and interpretation was the Eyesweb Open Platform package. With the merging of the SHIMMER™ device for data collection and the Eyesweb open frame software for data processing, an early prototype of the HPRD was produced. The HPRD was worn by 10 healthy subjects who underwent clinician guided bilateral Epleys manoeuvres. They also wore the device for bilateral self performed Epleys manoeuvres using Dizzyfix. Results: Our results demonstrate the highly-accurate angular measurement and orientation capabilities of the head worn HPRD, developed at our institution. We identified a greater degree of accuracy in the Dizzy-Fix guided Epley manoeuvre group, over the Clinician-guided manoeuvre. Conclusions: This study highlights the potential of a novel technology, HPRD in the future management of BPPV. Using the HPRD our study has established that the commercially available device; Dizzyfix, achieves greater angular accuracy in the performance of a PRM over the traditional Clinician-guided manoeuvre. 1630 - 1640 TRANS CANAL CONCHAL MYRINGOPLASTY- AN AUDIT CB Heffernan, BJ Conlon CARTILAGE UNDERLAY OBJECTIVES The senior surgeon utilises a trans canal conchal cartilage underlay myringoplasty technique for small dry posterior tympanic membrane perforations. The cartilage is sized and then tabs fashioned around the edge of it to allow easier insertion through the perforation while preventing it falling out of the middle ear. Our aim is to audit all patients who underwent this procedure in our institution over the past six years. METHODS Patients who underwent all types of tympanoplasty were identified from theatre logbooks and the HIPE system. A chart review then isolated those patients who had this specific procedure. Post-operative audiograms and otoscopic photographs were reviewed. RESULTS 10 patients were identified. These patients were chosen based on the fact they had isolated dry tympanic membrane perforations with no mucosal disease. All patients tolerated the procedure well with no early post-operative complications. At the three-month post-operative clinic follow-up all patients had intact tympanic membranes and no deterioration in their audiograms. CONCLUSIONS This method of preparing the cartilage graft is innovative and effective. Trans canal conchal cartilage underlay myringoplasty is a useful procedure for patients with dry central tympanic membrane perforations especially those with multiple comorbidities. . As there is no need for a post auricular incision or tympanomeatal flap it lends itself to a shorter operation, smaller scars and quicker recovery but with high success rate. 1640 - 1650 PETROUS APEX LESIONS; THE EXPERIENCE OF A NEUROOTOLOGY AND SKULL BASE MDM M. Sadadcharam, M. Javadpour, D. Rawluk, R. McConn-Walsh Objective The petrous apex is a relatively inaccessible region of the medial skull base surrounded by a number of important vascular and neural structures. Lesions arising in or spreading to the petrous apex cause varied and occasionally severe clinical sequelae, which typically result from mass effect or direct invasion of the cranial nerves, brainstem, or internal carotid artery. Because it is relatively inaccessible, the petrous apex is not amenable to direct examination. As such, imaging with CT and MRI plays an important role in diagnosis and characterization of lesions occurring there. Methods A retrospective study conducted in a university-based tertiary referral centre Results Fifty one patients with various petrous apex pathologies were reviewed. The most common presenting symptoms were hearing loss, dizziness, headaches, and tinnitus. The commonest lesions were petrous apex cholesteatomas, cholesterol cysts and metastatic lesions. The differentiating radiologic features of each were noted. Asymmetric pneumatisation, retained secretions and marrow gave radiographic findings commonly over-diagnosed as lesions of the petrous apex Conclusions Lesions of the petrous apex can be diagnosed accurately by CT and MRI. Where possible, both imaging modalities should be obtained as they provide complimentary information. If only one imaging modality is available, the preference should be for MRI (T1, T2 and T1 with gadolinium enhancement). 1650 - 1700 AUDIT OF AETIOLOGY OF GENETIC HEARING LOSS IN CHILDREN WHO A RECEIVED COCHLEAR IMPLANT BETWEEN JANUARY 2006- DECEMBER 2011 Doyle S., Leonard J., Viani L. Objective: The BAAP published comprehensive guidelines in 2009 which looked at the investigation of children with profound sensorineural hearing loss. Using these recommendations we performed an audit to look at aetiological investigations performed on children who received a cochlear implant between 2006 and 2011 at the National Cochlear Implant unit. Methods: 58 patient histories were reviewed. Data was retrieved from clinic and inpatient notes, correspondences and results stored in the charts. Results: 7 children had a diagnosis at the time of referral. 2 children were from consanguineous relationships. Of the 51 remaining children 38 (74%) were referred to genetics, 19 of the 58 had a family history of hearing loss, 39 did not. 21 of the children had specific aetiological investigations. 35 (60%) were referred to ophthalmology for assessment of suspected syndromes. 10 (17.2%) children had an ECG performed to rule out specific potential associated cardiac anomalies. Conclusion: Of the 58 children, there was a high rate of referral to genetics and Ophthalmology. A comprehensive guideline is needed for investigating these children. This has been implemented since March 2012 with the introduction of a clinic to formally investigate these children. The guidelines and protocols for investigation of suspected genetic hearing loss are described but we plan to develop guidelines to look and genetic and non- genetic causes of sensorineural hearing loss. 1900 - 2000 Drinks Reception 2000 - 2230 Wilde Discourse: Mr. Richard Canter (Bath, UK) followed by: Gala Dinner (Black Tie) / President’s speech Saturday 6th October 0730 - 0900 Registration 0900 - 1100 Free Paper Session (Paediatric + General + Head / Neck) Chairpersons : Turlough Farnan + Peter Walshe 0900 - 0910 BOTOX: A WRINKLE FREE APPROACH TO MANAGING DROOLING K. Davies, T. O Dwyer Objective: 1. To evaluate the efficacy of submandibular botox injections in the management of sialorrhoea 2. Assess its role in the long-term management of this condition. Methods: Retrospective review of a paediatric patient population with sialorrhoea treated by injection orowf Botox® into the submandibular salivary glands between 2005 and 2012. Efficacy and long term effect was evaluated with a pre and post procedure parental quality of life questionnaire. Results 73 injections were performed in 35 patients aged two to 21 years with a beneficial effect in 75% of cases. Three patients developed significant swallowing difficulties requiring NG feeding. Other minor complications included four patients noticing a change in the consistency of secretions. Long-term cure was achieved in 16 cases. The most effective protocol was injection of 50 units of botulinum toxin into each submandibular gland under ultrasound guidance. Conclusion The treatment of sialorrhoea by Botox® injections into the submandibular salivary glands is an effective and repeatable procedure. It plays a vital role in the management algorithm of sialorrhoea at our institution. Our results, complications and management will be discussed. 0910 - 0920 SURGICAL MANAGEMENT OF OTITIS MEDIA EFFUSION (OME) IN BELFAST TRUST, 2011-2012 N McCay, F Toner, K Trimble WITH OBJECTIVE Assess current practice against the recommendations of NICE CG60 guidelines on indications for surgical management of OME in children. METHODS Retrospective chart review of all children under 7 years of age having insertion of ventilator tubes between September 2011 and March 2012. RESULTS 107 children had surgery during the 6 month period with clinical history and examination involving general developmental status in 64%, general upper respiratory health in 74.5% and otoscopy in 98% of cases. Hearing testing was performed in 76.6% of cases and tympanometry in 97%. 67% of children had a documented 3 month persistence of bilateral OME and 45% had a hearing level of 25-30 dB or worse in the better ear. CONCLUSIONS Based on information recorded in patient charts 55% of children undergoing surgery for bilateral OME did not meet the NICE guidelines for intervention and 35.4% of children had not had hearing tested prior to surgery. 0920 - 0930 Audiological And Otological Outcomes In Children With A History Of Cleft Palate A. Doyle, P Roche, A. McGillivary, M. Earley, A. Blayney OBJECTIVE: To document the audiological and otological outcomes of a cleft palate cohort, and to review trends in the patterns of hearing loss and middle ear pathology. To establish the differences in outcomes based on severity of cleft. METHODS: A retrospective review of 166 cases of cleft palate with or without cleft lip was performed. The initial and final 4-point audiogram on the hospital chart was recorded, along with corresponding tympanogram and E.N.T surgical data. RESULTS: Of the 166 cases identified on the cleft database, 103 patients (51 females and 52 males) were eligible for inclusion. The mean age at final audiogram was 10.3 years. The majority of this cohort had cleft of the secondary palate (n=29). 55.3% patients were found to have normal hearing bilaterally at their last audiogram (n=57). No patients were found to have severe or profound hearing loss. 15.5% of patients had used at least one hearing device at some point in their care, (n=16). CONCLUSIONS: The severity of the middle ear disease experienced by our patients appeared to be related to the degree of tissue loss seen with the various cleft classifications but despite variation amongst the cohort, the majority had a normal final audiogram. 0930 - 0940 PAEDIATRIC AIRWAY CLINIC: THE EVER-EVOLVING DIVERSIFICATION OF ITS ROLE D Fitzgerald, H Rowley Department of Otolaryngology, Head and Neck Surgery Temple Street Children's University Hospital, Dublin 1 OBJECTIVES: To assess the evolution of the role of the paediatric neck and airway clinic, at The Children’s University Hospital, Temple Street, in the context of an increasingly varied neonatal and paediatric population. METHODS: A retrospective review was conducted of attendances at the clinic, over a ten year period, with a view to assessing case load and changing complexity. Referral patterns, presenting complaints and related diagnoses were correlated with clinical findings and outcomes, and surgical requirements. FINDINGS: In the initial years, management of relatively non-complex problems such as laryngomalacia, or the monitoring of children with tracheostomies, comprised the majority of cases. More recently, in particular in the past two years, there has been a marked increase in the complexity of our patients, correlating with the acquisition of new subspecialties linked to our centre. In addition to referring specialties already well-established, such as the Cleft Palate Clinic, we now collaborate with the Paediatric Transplant team, Craniofcial Unit, Maxillofacial and Neurosurgeons, amongst others. CONCLUSIONS: The Paediatric Airway Clinic now has a very diverse patient population, necessitating evolution of the service to provide ever more specialised expertise, in order to deal with new clinical challenges presenting themselves on an increasingly frequent basis. The provision of services to newly emerging subspecialties has lead to non-complex patients having to wait significantly longer for initial assessment. 0940 - 0950 MANAGEMENT OF THE OTOLARYNGOLOGIC FEATURES OF RARE CRANIOFACIAL SYNDROMES CB Heffernan , DJ Murray, H Rowley OBJECTIVES Our otolaryngology department works closely with the national craniofacial service. Craniofacial syndromes have numerous otolaryngology features due to their common embryological origin. Our department previously looked at the most common craniofacial syndrome which is Pierre Robin. Now we are auditing the rarer syndromes that we encounter such as Apert’s, Pfeiffer’s and Crouzon’s. We aim to give an overview of our involvement in the management of these rare syndromes. METHODS The craniofacial surgery department has a database of all their patients. We have retrospectively reviewed this database to identify those who required input from the otolaryngology department. We cross referenced this data with that from our airway database and the HIPE service. The patients with Pierre Robin were excluded. We reviewed the patients’ cases notes and our airway database. RESULTS Thirty patients were identified who presented to this department between 1990 and 2011. These patients had seven different syndromes with Crouzon’s being the most common. Data regarding airway management and hearing difficulties was collected. The most common procedures required were tracheostomy, choanal dilatation and ventilation tube insertion. All patients were followed until sixteen years of age after which they were transferred to adult services. CONCLUSION Craniofacial syndromes though complex can have excellent outcomes if managed in a multidisciplinary setting. Thorough airway assessment and management is the most important initial step. Also early audiological assessment is essential to prevent speech and language delay. 0950 - 1000 GUIDELINES FOR THE INVESTIGATION AND MANAGEMENT OF HAEMANGIOMA OF THE HEAD AND NECK E Phelan, K Davies, P Lenane, H Rowley Objectives: 1. Review the current investigations and management of paediatric head and neck haemangiomas 2. Highlight the role of the paediatric ENT surgeon as part of the multidisciplinary team approach in the management of this condition Methods: Retrospective chart review of all paediatric head and neck haemangioma patients presenting to or referred to the ENT outpatients. Results: Over forty children with head and neck haemangiomas over a 2 year period were indentified. The management protocol including indications for imaging, imaging type and other preliminary investigations were reviwed. Current indications for use of propanolol in each case was also analyzed. Conclusion: The investigations and management of head and neck haemangiomas has changed in the last number of years, however the paediatric ENT surgeon remains a crucial member of the multidisciplinary approach in the management of these difficult cases. 1000 - 1010 Improving Care For Thyroid Cancer Patients Phoebe Roche, James Paul O Neill, Siobhan Mc Quaid, Tadgh O Dwyer, Helena Rowley Department of Otolaryngology Head and Neck Surgery, Mater Hospital INTRODUCTION & OBJECTIVES: The incidence of thyroid carcinoma is now triple that of thirty years ago, and with approximately 56000 predicted cases in the US alone in 2012, it is now widely recognized as the fastest rising human cancer in the world. The aim of this study to examine the impact of recent changes we have made in the management of thyroid cancer patients in our department . METHODS: A review of the recently established protocols, guidelines and identified caseload of the Combined Thyroid MDT is performed and the impact of the establishment of a comprehensive thyroid cancer database and dedicated thyroid cancer clinic on patient care is evaluated. RESULTS: In total, sixty-five patients were treated for thyroid cancer between July 2007 and July 2012 across a variety of specialties at the Mater Hospital. Well-differentiated carcinoma accounted for approximately 89%, and females’ outnumbered males by over 2:1. New protocols and guidelines have been generated through the recently established MDT and the Endocrinology-Otolaryngology clinic with a view to improving future outcomes. CONCLUSION: Increasingly, patients with thyroid cancer are being referred to the Head and Neck Surgeon. We advocate a multidisciplinary approach, as it enables accurate stratification of patients, and effective implementation of evidence-based care in our practice. 1010 - 1020 IS SYSTEMATIC IDENTIFICATION OF ALL 4 PARATHYROID GLANDS NECESSARY DURING TOTAL THYROIDECTOMY? A PROSPECTIVE STUDY Rania Mehanna MB, Naveed Basheeth MB, Matthew S Murphy MB MRCPI*, Patrick Sheahan MD FRCSI (ORL-HNS) (corresponding author) Department of Otolaryngology – Head & Neck Surgery and *Department of Endocrinology South Infirmary Victoria University Hospital, Cork, Ireland Introduction: Routine identification of all 4 parathyroid glands has been advocated as a means of reducing rates of postoperative hypocalcaemia and inadvertent parathyroidectomy. The object of the present study was to investigate whether identification of more parathyroid glands during thyroidectomy performed by capsular dissection technique had any impact on incidence of postoperative hypocalcaemia and unintentional parathyroid resection. Study Design: Prospective cohort study of consecutive patients undergoing total thyroidectomy by capsular dissection technique over a 3-year period. Exclusion criteria included performance of concomitant central neck dissection; hyperparathyroidism; revision surgery; and invasive cancer. Methods: The number of parathyroid glands identified intraoperatively was recorded. No effort was made to find glands that were not obviously apparent during the course of dissection. Patients were not placed on routine calcium supplementation. Results: The final study population consisted of 126 patients. The mean number of parathyroid glands identified was 2.3. The incidence of biochemical (any postoperative calcium < 2 mmol/L) and clinical hypocalcaemia was 22.2% and 10.3%, respectively. Patients in Group A (0-2 parathyroids identified) had a significantly lower incidence of clinical hypocalcaemia than patients in Group B (3-4 parathyroids identified) (3.2% versus 17.1%) (p=0.02). The differences in biochemical hypocalcaemia were not significant (16.1% versus 28.1%, p=0.13). The incidence of inadvertent parathyroidectomy was 9.5%. There was no difference between the groups in incidence of inadvertent parathyroidectomy (9.7% versus 9.4%, p=1.0). Conclusions: Routine identification of all 4 parathyroid glands is not necessary in thyroidectomy performed using capsular dissection technique. 1020 - 1030 AUDIT OF INCLUSION CRITERIA FOR TONSILLECTOMY G Ferguson, PR Bell, SJ Hall OBJECTIVE: Tonsillectomy is one of the most common operations performed worldwide, but it is not without risk. Evidence-based guidelines exist to aid clinicians in identifying patients who would benefit from surgery. An audit was conducted to assess the inclusion criteria used in selecting patients for tonsillectomy. METHOD: 100 sets of patient notes were randomly selected for patients undergoing tonsillectomy in the preceding 12-month period. The outpatient notes were scrutinized including assessment of the general practitioners referral letter, the consultation note and final clinic letter. The inclusion criteria used for selecting patients for tonsillectomy were compared with existing national guidelines. RESULTS: Seventy-seven percent of patients who underwent tonsillectomy met the inclusion criteria outlined by at least one of the nationally used guidelines. Eleven percent of those undergoing tonsillectomy had other indications including symptoms of upperairway obstruction associated with tonsillar hypertrophy that are not included in national guidelines. The remaining twelve percent of patients did not have sufficient information documented in either the general practitioners referral letter or the clinic notes to adequately assess the decision for surgery. CONCLUSION: Suitability of tonsillectomy should be determined by clinicians based on what is appropriate for each individual patient. We recommend that departmental guidelines are regularly reviewed to improve cost-effectiveness and to ensure the highest levels of patientsafety are achieved. We also recommend the provision of departmental guidelines to local general practitioners to ensure patients are not inappropriately referred to the Otorhinolaryngology service. 1030 - 1040 Improving tracheostomy decannulation in recalcitrant cases using the comprehensive dynamic airway assessment (CDAA) T. Ashfield 1, B. Shephard 2, D. Chatterjee 2, L. Clark 3, I. Ahmad 2, R. Oakley 1 Department of head and neck surgery 1, Department of anaesthesia 2, Guy’s Hospital, Department of speech and language therapy 3, King’s College Hospital, London, UK Objectives Prolonged tracheostomy is associated with morbidity, mortality and increased length of stay. Fibre-optic endoscopy (FE) is advocated for such cases but is limited to the supraglottic airway. Anaesthetists commonly perform fibre-optic intubation under local anaesthesia. CDAA introduces this method to the ward setting, allowing conscious assessment of the entire upper airway. CDAA been performed in cases of failed tracheostomy decannulation, enabling decannulation under direct vision if appropriate. Methods FE is used to assess the entire supra- and sub-glottic airway including dynamic cord function. Through video presentation we demonstrate the following procedure. Co-phenylcaine is administered to the nasal cavity and atomised 4% Lidocaine to the laryngopharyngeal mucosa. Pulse oximetry is used and no sedative agents are given. CDAA is performed after 15 minutes and a diagnosis for failed decannulation can be made or refuted. The tracheostomy can be decannulated under direct vision if indicated. Results Outcomes of 213 post critical-care tracheostomised patients were audited from April 2009-April 2012. Twenty-seven(13%) patients failed decannulation due to reduced airflow. Of these, 23 underwent conventional review and FE which yielded a 17%(4) decannulation rate; 2 of the remainder subsequently died with tracheostomy in-situ. Since its inception in August 2011, 8 patients have undergone CDAA with a 75%(6) in-procedure decannulation rate. Discussion CDAA has been successfully applied to a heterogeneous group. It is a significant development in improving outcomes for patients with complex tracheostomies. It requires minimal resource, is versatile and exploits skills available to the otolaryngologist. CDAA could form an integral part of all decannulation protocols. 1040 - 1050 The Robotic Head and Neck Surgeon James Paul O’Neill, Dennis Kraus Memorial Sloan Kettering Cancer Center New York, USA Abstract: Introduction: Transoral robotic surgery (TORS) provides access to the oral cavity, oropharynx, hypopharynx, larynx, parapharyngeal space and skull base vial the oral aperture. Methods: We performed a variety of TORS manoeuvres over 2011 within our department. These included robotic platform operational skills, set up of the patient side system, and extirpation of malignant tumours of the oral cavity and laryngopharynx on 15 patients. We then recorded the operative and post-operative course of these patients. Results: 14 patients had successful oncological resection of their tumours without positive margins. The robotic laryngectomy was abandoned and converted to an open standard technique. Post operative morbidity included secondary haemorrhage and a temporary tracheostomy on 2 patients. Conclusions: Experienced clinical judgment, surgical skills, and oncologic principles are necessary for the needs of the individual cancer patient A learning platform exists for robotic surgical techniques. We would encourage the IOS to embrace Robotics and introduce these novel techniques for Otolaryngology, Head and Neck Surgical trainees. 1050 - 1100 Novel Strategies In The Management Of Anaplastic Thyroid Carcinoma A Dias, M Alhashemi, ER Dorris, P Smyth, M Flanagan, V McEneaney, J O’Leary, O Sheils Introduction Thyroid carcinoma is the most common endocrine malignancy. Papillary thyroid carcinoma(PTC) is the most common type of thyroid cancers. Current treatment strategy is based on surgical removal of the thyroid gland with adjuvant radioiodine ablation of remnant cancer cells. BRAFV600E mutation is a common mutation found in PTC and poorly differentiated anaplastic thyroid carcinoma(ATC). BRAFV600E mutation causes activation of the Mitogen-activated Protein Kinase(MAPK)/Extracellular signal-regulated kinase(ERK) signaling pathway, causing tumorigenic transformation of the cell. This constitutive activation causes a downregulation of iodine-metabolizing genes(TSHR) in the thyroid tumor cells leading to loss of radioiodine avidity, rendering treatment ineffective. Aim To evaluate the expression of Thyroid stimulating hormone receptor(TSHR) in an anaplastic thyroid cancer cell line carrying BRAFV600E mutation and to investigate the effect of MEK inhibition on TSHR expression by suppressing the MAPK/ERK pathway using the selective MEK inhibitor PD0325901. Method The new generation slective MEK inhibitor PD0325901 was used to block the MAPK/ERK pathway in an anaplastic thyroid carcinoma cell line carrying BRAFV600E mutation and a normal transformed cell line. TSHR expression was assessed using TaqMan RT-PCR and immunofluorescence confocal imaging. 1100 - 1130 Coffee Break 1130 - 1300 CME Session Chairpersons : Greg McBride + Martin Donnelly 1130 - 1200 Guest Lecture Paediatric DCR - Paul White 1200 - 1230 The IOS Debate : Day Case Tonsillectomy Joe Toner, Belfast (for) / Helena Rowley, Dublin (against) 1230 - 1300 Current Training in ORL Richard Canter (UK) / Michael Walsh (Ireland) 1300 - 1330 Closing Speech Best Paper Prize (Sponsored by Tekno Surgical) Best Poster Prize 1330 - 1430 Luncheon Meeting - Irish Institute of Otolaryngology Notes for paper presenters: Each talk has been allocated ten minutes - eight for delivery and two for questions/discussions. A bell will sound at the end of eight minutes, and again at nine. There is a best paper prize, and points will be deducted for exceeding your time. In order to ensure a smooth changeover between talks, we suggest you send us your presentation in slide format to info@iosconference.org at the earliest. You will always receive an acknowledgement. If you do not, it means that your slides have not transmitted successfully. Please note that anyone who sends on their presentation must also bring a copy of it to the meeting. The person in charge of audio-visual facilities at the conference is Ollie O’Flanagan. If you have specific queries regarding format, video-clips, Apple Macs, etc., do contact him at ooflanagan@rcsi.ie immediately (his mobile number should you need it is 00 353 87 9672013). Anyone wishing to use an Apple Mac must bring along the VGA conversion dongle that comes with the Mac. Mr. Flanagan will be available to load slides at the venue on Thursday 4 October between 6 pm and 7.30 pm, and again on Friday / Saturday mornings between 8 am and 9 am; and during refreshment breaks on each of these two days. Please ensure you meet up with him and give him your slides well in advance of your slot. It will not be possible to do this at other times, and especially not at the start of your presentation. The best paper will be announced at the end of the conference on Saturday afternoon. Notes for poster presenters: Please ensure your poster is put up by 9 am on Friday 5 October. The judges will visit the display later that day during the second coffee break (3.30 to 4 pm) and may wish to speak to you regarding your material - you should be available at the poster at this time to give a short presentation (max. three minutes) should you be required. The best poster prize will be announced at the end of the conference on Saturday afternoon, and attracts a prize. Trade Exhibition Allergy Therapeutics plc. Arthrocare Audico Limited Baxter Healthcare Ltd. Cochlear Europe Ltd Covidien Ireland Commercial Ltd Endosurgical Ltd Fannin Limited HC21 Healthcare Irish Hospital Supplies Ltd. Johnson & Johnson Medical Ireland Meda Health Sales Medserv Limited Medtronic Ltd. A. Menarini MSD Ireland Ltd Murray Surgical Ltd. NeilMed European Division Omega Financial Management Pharmed Holdings Limited Radiesse Voice Sword Medical Synthes Medical Ireland Tekno Surgical Vista Pharmaceuticals