identification and treatment of substance use disorders
advertisement

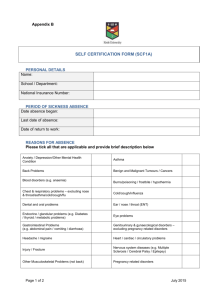
Substance Use Disorders Introduction to the Identification and Treatment of Substance Use Disorders (SUDS) B. Thomas Gray, Ph.D. Directions: To receive 2 hours continuing education credit for psychologists, licensed psychological associates, licensed professional counselors and licensed social workers, for this TPA sponsored home study assignment, you must: 1) 2) Read the article in its entirety; Take the test at the end of the article; Mail or fax the test answers along with $45 (TPA Members) or $65 (Non-TPA Members) to the Texas Psychological Association, PO Box 1930, Cedar Park, TX 78630 (512) 255-1642.. Examinations will not be scored without appropriate fee. You must answer correctly 70% or better to pass the examination. If you do not pass, you may retake the test, with payment again of the test fee. 12/29/03 1 Substance Use Disorders 2 Introduction to the Identification and Treatment of Substance Use Disorders (SUDS) B. Thomas Gray, Ph.D. Substance Use Disorders (SUDs) are arguably the most common mental health problem in the United States. A large proportion of persons presenting for care in medical and mental health settings meet criteria for one or more SUDs, and it is inevitable that a psychologist engaged in clinical practice will encounter such individuals. It is therefore important to have a good working knowledge of the disorders and related problems. This article is intended to provide a general introduction to the SUDs and their treatment. It is impossible in this context to engage in a comprehensive review of all relevant areas, and this article alone is far from sufficient to allow the psychologist lacking background to become proficient in working with SUDs. For example, I do not address problematic use of nicotine or caffeine here. Because of the general nature of this discussion, specific references are not cited in the text; I have instead appended a rather lengthy bibliography, organized topically, for the use of those who wish to pursue further information. Internet addresses are also provided to resources such as Division 50 (Psychology of Addictions) of the American Psychological Association, the National Institute on Alcohol Abuse and Alcoholism, the National Institute on Drug Abuse, and other government outlets. Training opportunities are typically available on a regular basis in most areas, and the interested psychologist is encouraged to take advantage of as many as possible. My email address is provided here, as well, and I would be more than happy to assist anyone searching for further information and training. Introduction Epidemiology Roughly one in ten people in the United States meet criteria for a SUD. A strong and compelling correlation has been repeatedly documented between substance use, particularly alcohol use, and a wide range of social and personal issues: violent crime, suicide, domestic violence, child abuse, and traffic accidents and fatalities. The economic cost of alcohol and other drug misuse runs into the tens of billions of dollars each year. Approximately 25% of children in the U.S. witness alcohol misuse in their families, and more than half of American adults have a close family member with serious alcohol problems. One readily becomes inured to such statistics, yet the implications for psychologists are far reaching. A substantial proportion of the U.S. population clearly has problems relating to substance use, either through their own use, or that of a close relative. The frequency of SUDs is even higher among those who present for medical and and/or mental health care in a variety of settings. In many hospitals, for example, over half the emergency room visits are the direct or indirect result of alcohol and other drug use. Sixty percent or more of incarcerated individuals have direct or indirect connections with alcohol and/or other drug use. SUDs are also the most common disorder co-occurring with other mental health diagnoses. Available data suggest that 50% or more of patients diagnosed with Schizophrenia also have a concurrent alcohol or illicit drug use disorder (or both). One important conclusion that can be drawn is that the settings in which psychologists are frequently employed are precisely those where we find significant numbers of patients with SUDs. Consequently, whether a psychologist in clinical practice chooses to or not, she will almost inevitably be exposed to a substantial number of individuals who are abusing substances. Refusing to address SUDs means one of two things: the range of potential patients that can be seen by the clinician will either be dramatically reduced; or more likely, SUDs that exacerbate another Substance Use Disorders 3 mental health condition will be misdiagnosed or even overlooked, meaning the patient receives inadequate care. Substances of Abuse Drug Classification. Substances of abuse may be conveniently grouped into several different categories based on pharmacological similarities, as illustrated in Table I. Alcohol, for example, is grouped together with other minor tranquilizers and sedative-hypnotics, such as the benzodiazepines and barbiturates. This is because the effects of these various drugs on the individual are quite similar. In addition, the withdrawal syndrome that individuals experience after they become dependent on these substance is quite similar. This is why benzodiazepines are often effective in treating severe alcohol withdrawal. Cannabis (marijuana and hashish) is a rather unique substance that is variously described in terms of sedative, stimulant, and even hallucinogenic properties. Different authorities classify cannabis in different ways, and for this reason, I have identified it as a separate category in Table I. A group of socalled Designer Drugs are also identified as a separate category. These are drugs that have been synthesized by illicit drug producers over the past 15 to 20 years, drugs that often have characteristics of more than one of the categories outlined in Table I. MDMA, commonly known as “ecstasy,” is one of these Designer Drugs that has gained considerable notoriety of late; it has properties of both amphetamines (psychostimulants) and hallucinogens. A related substance deserving of mention is a combination of marijuana that is soaked in formaldehyde or a similar fluid used in embalming, with the latter usually classified as an inhalant. This product is often referred to on the street as “fry,” or “whack,” and greatly magnifies and alters the effects of the marijuana alone. The addition of the inhalant component seems likely to introduce the hazard of serious neuropsychological sequelaeRoute of Administration. An important question with many substances is the way in which it is taken. Alcohol, of course, is primarily used via a single route of administration – oral. Other drugs, however, may be taken in multiple ways. Cocaine and heroin, for example, may be used intranasally (“snorted”), injected subcutaneously (IM), injected intravenously (IV), or smoked. The differences in effect between the various routes of administration are quite significant. Perhaps most illustrative is that of cocaine. Prior to the later 1980s, clinicians generally did not believe that one could become seriously physically dependent on cocaine. In the mid-1980s, though, crack, the smokable form of cocaine, became widely available and quickly became extremely popular. Smoking cocaine delivers a notably more concentrated dose, and hence a much more powerful immediate effect, even than IV use of the drug. This made the drug considerably more physically and psychologically reinforcing, which was compounded by the fact that the more potent form also has a shorter duration of effect; thus, the behaviors involved in using crack had to be repeated more frequently, adding to the reinforcing properties. Given the substantial impact that route of administration can and does have with many substances, it is critically important for the clinician to inquire about this aspect of drug use during an interview early in the assessment process. Diagnostic Issues. DSM Categories. The current edition of the Diagnostic and Statistical Manual of Mental Disorders1 (DSM) identifies numerous diagnoses related to substance use. By far the two most commonly diagnosed categories are abuse and dependence. Abuse of a substance is defined as continued use despite problems due to any of the following: abdication of primary role responsibilities (e.g., work, school, and/or family), legal entanglements, social and/or interpersonal difficulties caused by use, or use in hazardous situations such as driving. A diagnosis of dependence on a substance requires at least three of the following: physical tolerance; a distinct withdrawal syndrome2; use of more of the substance and/or for a longer period than intended (sometimes interpreted as loss of control over use); inability to reduce or stop use despite a desire to do so; an inordinate investment of time in using and/or recovering from the effects of use; important activities given up or reduced due to use; or continued use despite knowing that use is 1 American Psychiatric Association. (2000) Diagnostic and statistical manual of mental disorders (4th ed., text revision). Washington, D.C., Author. 2 Tolerance and/or the presence of a withdrawal syndrome (which the DSM defines to include use of the substance or a similar substance to avoid withdrawal symptoms) are generally recognized as signs of physical dependence. Substance Use Disorders 4 causing or exacerbating physical and/or mental problems. One may be diagnosed with either abuse or dependence of substances from most of the drug categories outlined in Table I, with dependence clearly being more problematic for the individual (and for those around him or her). Using three or more substances (excluding nicotine and caffeine) to the extent that criteria for Substance Dependence are met qualifies the individual for a diagnosis of Polysubstance Dependence. Potential diagnostic confusion. Heavy and prolonged misuse of alcohol, of any of a variety of illicit drugs, of prescription drugs, or a combination thereof, will readily produce symptoms that will mimic those of virtually any other mental health disorder listed in the DSM. This can and often does make proper diagnosis quite challenging, particularly if assessment of substance use is not adequately conducted. Perhaps the clearest example is that of alcohol and depression. Alcohol is a central nervous system sedative, and consequently, anyone who drinks heavily for a protracted period of time will almost inevitably begin to show signs and symptoms of depression. Whether such an individual should be diagnosed with a depressive disorder concurrent with the alcohol use disorder along with a concurrent depressive disorder could be debated at some length. Regardless, it would be quite important in formulating an adequate treatment plan to recognize the possibility if not the likelihood that the depressive symptoms were secondary to alcohol misuse. If adequate history demonstrates the existence of a depressive disorder prior to the onset of problematic drinking, an independent diagnosis is clearly warranted. Once the patient has been able to maintain continuous abstinence from alcohol or other drugs for a period of at least a few weeks, the persistence depressive symptoms would similarly argue for an independent diagnosis. Another clear example of the diagnostic confusion induced by use/abuse of substances is seen in the psychotic symptoms, auditory and visual hallucinations in particular, that are sometimes manifested by heavy psychostimulant abusers and by severely alcohol dependent individuals during acute withdrawal. The latter case is only rarely seen, and is potentially confusing because the typical hallucinations often do not appear until 24 to 36 hours following sudden cessation of alcohol use. It is essential for the clinician to be alert to such circumstances, and to accurately diagnose, however, because the situation is potentially emergent; as many as one in seven patients who reach such a point during withdrawal from alcohol dependence will die if untreated. The case of psychostimulants is more common. Persistent use of cocaine or amphetamine, particularly if smoked rather than taken intranasally or by injection, will almost inevitably produce auditory hallucinations, sometimes visual hallucinations, and occasionally tactile hallucinations; accompanying delusions are also often seen. These symptoms can easily be mistaken for a true thought disorder, when they are in fact secondary to misuse of psychostimulants. Identification of SUDs The above discussion has emphasized the importance of accurately identifying SUDs. A thorough clinical interview will typically be a fundamental source of information to provide the basis for accurate identification. Nevertheless, it is often useful to have available brief screening measures to aid in detection of SUDs, and as with most other disorders, paper-and-pencil forms of psychometrically sound tests are particularly efficient. A plethora of substance use screening instruments have been published over the years, especially within the last 15 to 20 years. These typically fall into two distinct categories, direct and indirect. Direct tests are those that inquire about various symptoms of substance abuse in a straightforward fashion. They consequently have high face validity, and are sometimes criticized for being readily subject to manipulation. Examples include the Michigan Alcoholism Screening Tests (MAST), the CAGE, the Alcohol Use Disorders Identification Test (AUDIT), and the Drug Abuse Screening Test (DAST). The other category is indirect tests, which are typically empirically derived from large question pools, and are purported to be useful in identifying substance abusers. Probably the best known example of an indirect Substance Use Disorders 5 test is the McAndrews Scale (MAC and MAC-R3) of the Minnesota Multiphasic Personality Inventory. A possible advantage of indirect tests is the claimed resistance to dissimulation. Psychology has yet to see any reasonable test that correctly identifies all members of the target group and at the same time correctly excludes all non-members of the group. Obviously, this applies to substance abuse screening instruments, as well; all of the available tests are distinctly fallible. Nevertheless, some are more useful than others, and it is clear that direct tests have consistently yielded higher reliability estimates and greater actuarial accuracy than indirect tests. This holds true across a variety of different populations, including criminal justice groups (i.e., DWI samples). Figure 1 compares the MAST and the MAC/MAC-R on sensitivity (the percentage of those with a substance use disorder accurately identified by the tests) and specificity (the proportion of non-substance abusers accurately excluded by the test) for various samples. The predictive superiority of the direct test is clearly seen. Manipulation of cutoff scores for any test will, of course, dramatically impact the actuarial outcome. A higher cutoff score will yield more false negatives (i.e., subjects who have SUDs but who are not identified as such by the test), and a lower cutoff score will yield more false positives (subjects who are identified by the test as having a SUD despite not meet criteria for one). In most clinical situations, the ideal approach is to use a lower cutoff, and then use a thorough interview to “weed out” the false positives. Such an approach is also very useful when more complex cases, such as those involving co-morbid substance use and other psychiatric disorders. Table 2 includes a number of questions or question categories that can be usefully added to a clinical interview format to provide a more complete picture of the patient’s substance use and potential problems relating to that. Treatment History Before considering various treatment modalities, it is useful to briefly review the history of substance abuse treatment in the United States. Present day concerns regarding current levels of alcohol consumption in this country notwithstanding, it is interesting if not surprising to note that per capita alcohol consumption has declined rather substantially since Colonial days. Considerably higher levels of alcohol use were seen throughout the Nineteenth Century and into the early part of the Twentieth Century. By the mid-1800s, a powerful religious coalition that came to be known as the Temperance Movement was gaining cohesiveness, and with that, political influence. Segments of this group were strong supporters of the Pure Food and Drug Act of 1906, that required manufacturers to accurately label the contents of salable food and drug items; the Department of Agriculture was identified as the agency responsible for enforcement, and interestingly, the Coca Cola Company was one of the first targets. A second major piece of legislation backed by the Temperance Movement was the Harrison Act, passed in 1914. This act was focused on addictive drugs, and gave authority to the Treasury Department to strictly regulate these substances. The impact of the anti-drinking coalition culminated in 1919 when the 21st Amendment, also known as the Volstead Act, was ratified, ushering in the era of Prohibition. In the 19th and early 20th centuries, several sources of treatment were available for persons with alcohol or other substance use problems. Especially prior to the Pure Food and Drug Act of 1906, a variety of patent medications were marketed as being useful treating problems related to use of several different substances, including especially alcohol and tobacco. One of the most successful of these was the so-called “Gold Cure,” which was actually a series of similar “programs” that at their core had “patients” regularly imbibe a mysterious elixir containing a “secret ingredient.” The latter was originally claimed to be gold, although it never was, and the claim was quickly dropped. Although several versions of this scheme appeared by the late 1800s, the original and most widespread enjoyed great popularity for some 20 years, until an increasingly skeptical public (and press) brought about its demise. 3 The MAC-R is the revision of the MacAndrew scale that came with introduction of the second edition of the MMPI in 1989. Substance Use Disorders 6 A number of private clinics, hospitals, and sanitaria offered services, usually residential or inpatient. Given that the superintendents and senior staffs of most of these facilities were psychiatrists, and that psychiatry at that time was in large part given over to psychodynamic psychotherapy, this was precisely the form of treatment that was most often provided. Meta-analytic studies of more recent applications of such approaches have generally shown psychodynamic treatment to be notably less effective than most other approaches. Probably the most common source of treatment for individuals with alcohol and/or other drug problems prior to Prohibition, however, was found in state hospitals and related public-funded institutions, such as “Inebriate Hospitals. “ Not surprisingly, given the predominance of psychiatric thinking in most of these facilities, some elements of psychodynamic thinking were also to be found in the care provided. The daily routine, for the most part, though, consisted of regular religious worship and work of some sort. The latter seems likely to have stemmed from the Judaeo-Christian homily regarding “idle hands.” Prohibition was, of course, a resounding failure, indicative of ineffectiveness of government efforts to eliminate use of substances. By the time it was finally repealed in 1933, economic conditions had changed dramatically and the U.S. was in the throes of the Great Depression. Funding for treatment was therefore sharply diminished, in part because of severely strained government budgets, but also due to a perceived absence of need stemming from the faulty assumption that making any drug illegal is sufficient to eliminate any problems related to its use. It was in this environment that Alcoholics Anonymous (AA) emerged in the middle and late 1930s. Beginning in Ohio, and quickly spreading to New York (one of the two men who is credited with founding the group was from New York), a core membership and leadership emerged that took responsibility for codifying the basic tenets of AA. The approach is laid out in some detail in the basic text of Alcoholics Anonymous, and is based on the 12 Steps (see Bibliography). The fledgling movement came to the attention of Jack Anderson, the well-known reporter, who wrote an article that appeared in the Saturday Evening Post in 1941; attendance at AA meetings promptly and dramatically increased. By the late 1940s, AA had become well known across the U.S., and claimed a membership of over 100,0004. The self-help group had gained a sufficiently positive reputation that two separate facilities arose independently in Minnesota, both offering treatment for substance-dependent individuals (primarily alcohol-dependent) based on AA principles. One of these, Pioneer House, was publicly funded; the other has grown from a staff of four on a privately owned farm, into the major corporation of Hazelden. In less than two years, many of the same approaches were borrowed in the implementation of a program for excessive drinkers at Willmar State Hospital, also in Minnesota.5 Because of their proximity to one another, the staffs of these different programs routinely interacted with one another and exchanged ideas, and sometimes jobs, as well. It is therefore difficult if not impossible to credit specific programs or individuals with any of the various additions and modifications that were made to the treatment approaches that were used throughout the 1950s and 1960s. For fairly obvious reasons, this became known as Minnesota Model treatment (MMT). Many elements of the Pioneer House/Hazelden/Willmar programs were adopted by a group of recovering entrepreneurs who started the Parkside group a few years later; Parkside went on to become the largest chain of substance abuse treatment providers in the U.S. and other countries in the 1960s and 1970s. Hazelden was originally intended to serve two markets: alcohol-dependent clergy; and “professional class” (i.e., those who had not yet lost everything due to their drinking) alcohol-dependent The Forwards to each of the three editions of Alcoholics Anonymous, the standard text of AA, often referred to as the “Big Book,” reported membership in the various groups throughout the world rose from “over 100” in 1939, to more than 150,000 in 1955, to more than 1 million in 1976. 5 The hospital staff were apparently under the impression that the other two programs were much more firmly established than they in fact were. 4 Substance Use Disorders 7 men6. The concept was tacitly broadened to include other drug dependencies within a few years, due in no small part to the lack of available treatments. It in fact took Hazelden a number of years to adequately develop a market for treating the still-employed person with SUDs, and Parkside adopted and achieved similar goals. Out of these efforts was born the concept of Employee Assistance Programs, now very widely used in business throughout the U.S. An important point that must be emphasized is the virtual absence of psychologists throughout the process of developing these early treatment efforts. Indeed, psychology as a discipline tended to ignore problems related to alcohol and other drug use. As but one illustration, the major psychology journals in the U.S. published only a small handful of articles pertaining to SUDs prior to 1950. The major texts pertaining to group therapy (a primary modality employed in MMT) in the 1970s and 80s contained explicit statements regarding the inadvisability of including persons with SUDs as group members. Given the dearth of professional interest, it should not surprise us in the least that others stepped in to fill the void in terms of providing services. The practice of hiring people with reasonably stable histories of recovery as measured by periods of abstinence originated very early on in the development of MMT, and has of course continued in somewhat more sophisticated form up to the present. The ultimate and stereotypical version of MMT was the 28-day residential program, an idea that had much less to do with any sort of therapeutic rationale than it did with efforts to serve a business market7. An extreme variant was hospital-based and included round-the-clock nursing care and daily monitoring by psychiatrists. Many of the residential programs became casualties of the rise of managed care in the late 1980s and early 1990s, as insurance companies became increasingly skeptical of the value of paying for 4 weeks of inpatient hospitalization. Thus, a number of outpatient-based programs, that typically made less use of routine psychiatric care, began to arise. Importantly, psychologists have sometimes been involved in these efforts, which is in part a reflection of an awakening of attention to the importance of SUDs. An interesting result of the increase in outpatient treatment has been a significant departure from the traditional approaches of counselors working within these programs. The stereotypical “in-your-face” substance abuse counselor, as depicted in several popular films and TV programs, made heavy use of confrontation as a technique, and this was sometimes the primary “therapeutic” technique. Such strategies proved far less effective in outpatient settings, where the patient was free to leave and might not return. Simple economic necessity, aided perhaps by the inclusion of psychologists and other professionals with greater academic training in some programs, has led to a broadening of therapeutic approaches. Minnesota Model Treatment (MMT) The original Pioneer House/Hazelden/Willmar program revolved largely around attendance at AA meetings supplemented by lectures on the 12 Steps and related points. Over the years, as MMT was further developed, a number of additional components were added. A point of particular emphasis for many years has been the concept of substance dependence as a disease. This is frequently referred to as the Disease Model, and was a fundamental justification for establishment of hospital-based programs. The Disease Model formulation draws heavily on a biological (especially genetic) origin for alcohol problems, which presumably applies to other drugs, as well. Research has been quite consistent in showing that the child of a parent with an alcohol problem is three to four times as likely to also develop an alcohol problem. There is also evidence that has accumulated of late implicating dopamine and suggesting a possible genetic 6 Prior to the late 1970s, when former First Lady Betty Ford revealed publicly that she had undergone treatment for a SUD, women were far less frequently recognized as having such problems. It is no coincidence that the California treatment center that bears her name has essentially followed a Minnesota Model approach. 7 The essence of the idea was to offer to businesses a program by which they could salvage a valued employee who had developed a SUD by having him or her devote two weeks of vacation time and two weeks of sick leave to a full-time treatment program. The benefit to the employee was that, rather than being summarily terminated, his (or later, her) job would be held open pending completion of treatment. Substance Use Disorders 8 explanation for this phenomenon. At the same time, however, it has also become apparent that biological explanations alone are insufficient to explain all, or perhaps even most, cases of alcohol dependency. For example, convincing data has been presented in the last several years that strongly suggests trauma as a causative factor in the development of SUDS. The Disease Model also posits that alcohol and other drug problems are chronic, that they follow a reasonably consistent and progressive course, and that, if untreated, they will lead to death. It is undeniable that, in a large number of cases, these generalities apply. This conceptualization was based in no small part on work by E. M. Jellinek in the 1940s and early 1950s,8 particularly his analysis of a questionnaire that had been published in the Grapevine, the official newsletter of AA. As one would expect, the items correspond rather closely to the model of severe drinking problems that is outlined in the AA text. Given the tendency of members of any group to sometimes retrospectively reinterpret their prior experience to correspond more closely with that of other group members, the AA respondents tended to endorse questions in a manner that fit the same scheme. Thus, it is teleological to assert this evidence supports the interpretation that the progression of alcohol-related symptoms that is described by AA is universal. Despite questions concerning some of the foundations of the Disease Model of SUDs, other data is more supportive. For example, George Vaillant’s classic longitudinal study show that, although his alcohol dependent group9 decreased in size over time, this was primarily because these individuals either stopped drinking or they died. It appears that a substantial proportion of those who stopped did so without any formal intervention, a point that runs contrary to some presentations of the Disease Model. Another important finding in Vaillant’s study was the small but important number of previously alcohol dependent individuals who had returned to asymptomatic drinking. This runs contrary to another and perhaps even more fundamental tenet of MMT, one derived clearly from AA: once an individual develops a SUD, it may go into remission, but never completely resolves. A corollary is the consequent necessity of abstinence as a primary treatment goal. The issue of whether or not SUDs are a disease has generated no small amount of controversy, some of it quite acrimonious. Good arguments can and have been made on both sides, and the debate can be predetermined simply in defining the term disease. A reality, however, is that a model of SUDs as a chronic disease fits the experience of a large number of alcohol and/or drug dependent individuals. MMT in various forms is by far the most widespread and commonly available treatment in the U.S., and has been quite helpful to many, but certainly not all, of the afflicted. As noted above, another aspect of the MMT approach is the belief that abstinence from alcohol/illicit drug use is a necessary treatment goal. It is certainly true that, for many patients, abstinence is probably the wisest route. However, achieving that goal is often not an easy matter. An alternative approach that has gained a considerable following is Harm Reduction, which instead posits that, even if abstinence may be ideal, this is rarely attained, particularly on the first try. Therefore, perhaps it is more effective to work toward reduction of use, thereby reducing the potential damage caused by use. The counter argument is that such an approach is overly permissive, and encourages ongoing use by effectively telling the patient it is “okay” to continue using. There does not appear to be much in the way of a middle ground in this debate at present, and the conflict between two schools of thought remains readily accessible. As a final commentary in this section, it must also be pointed out that some of the criticisms leveled at AA (and consequently at MMT, as well) by psychologists border on the preposterous. It is quite common to hear a psychologist make a statement of the form, “I know someone who tried it [AA] and it 8 Jellinek, E. M. (1946). Phases in the drinking history of alcoholics: Analysis of a survey conducted by the official organ of Alcoholics Anonymous. Quarterly Journal of Studies on Alcohol, 7, 1-88. Jellinek, E. M. (1960). The disease concept of alcoholism. New Brunswick, NJ: Hillhouse Press. 9 Different criteria were in use at the time Vaillant’s study was initiated, and this group does not correspond precisely to the current DSM definition of Alcohol Dependence. Substance Use Disorders 9 didn’t work…,“ or, “They became dependent on 12-step meetings…” Many if not most practitioners have encountered patients for whom a specific therapeutic modality was not very helpful, or who became dependent on the therapist and/or the approach. This is far from sufficient to abandon the entire approach! Perhaps the most absurd commentary, though, is the statement that AA (and by default, MMT) is not helpful because “It’s not scientific.” If we as a profession truly followed such dicta, there would be few acceptable therapies available. In truth, AA itself represents an excellent first line intervention for patients with alcohol problems, and Narcotics Anonymous may similarly be helpful for someone having difficulties with illicit drugs. Twelve-step programs are cheap, they are readily available, volunteers can usually be accessed virtually around the clock, and they provide considerable social support for modifying the substance-using behavior. Of course, the psychologist should keep in mind that 12-step self-help groups are distinct from and must be regarded as separate from MMT. Referring a patient to AA is not the same as referring him to the Betty Ford Center or a similar MMT-based program, and vice versa. There is nevertheless a good deal of overlap in philosophy and approach, and there is sometimes considerable animosity on the part of psychologists for either. It cannot be stated too strongly that, if you, as a treating clinician, refer a patient to either AA or MMT, it is critically important that you be supportive of that referral. Conveying the impression, either overtly or covertly, that attending AA or going through an MMT program will not be helpful, then of course that will prove to be the case. The ethical course is learn more about the 12-step approach, perhaps by reading the AA Big Book and even attending some meetings; the alternate course is to find a different referral. Of course, you could also expand your level of expertise and provide the primary treatment yourself, but if that is the chosen course, it is worthwhile to keep in mind that AA/NA can be a useful support for your patient if she does not object too strongly. Substance Use Disorders 10 Other Treatment Modalities Brief Interventions. Critics of MMT have been quick to point to the relatively low rates of patient retention and treatment completion, as well as low rates of success as judged by numbers of patients who are able to maintain abstinence from alcohol and illicit drugs. This has led several clinicians, particularly those working in medical settings, to develop alternative approaches involving much briefer interventions. These interventions are sometimes referred to as simply “advise giving,” in that they typically comprise a single session during which someone such as a physician provides basic information concerning misuse of particular substances. In some versions of this, referral information for appropriate 12-Step self-help groups or other self-help groups is provided, as well. The patient is also typically given contact information should additional care be desired. There have been a number of variations of such brief interventions that have been tested. Results are common not surprisingly, rather variable, but typically show rates of abstinence comparable to those attained by the traditional 28 day treatment programs. Aversion Therapies. A number of aversion-based “cures” for SUDs have been offered, going as far back as the later 1800s, well before the learning concepts so familiar to psychologists had been formalized. The early approaches often involved administration of a chemical that induced nausea and/or vomiting, paired with use of alcohol. This is essentially the same procedure that is still in use in a few programs today. It is interesting that some records suggest Hazelden had experimented with some aversion-based treatment in the early 1950s. By far the best known example of formalized aversion therapy for SUDs in the U.S., though, is the Schick and Schick-Schadel Clinics. The original Schick facility was founded in Seattle, coincidentally around the same time that Wilson and Smith were beginning to formulate the basic principles of AA. The Schick approach was sufficiently successful that within a few years a second program was opened in Fort Worth, and remains so today. A limited range of outcome data have been published from the Schick-Schadel programs, suggesting rates of success at least as promising as those from MMT-based programs. Cognitive Behavioral Treatments. A relatively recent development is the appearance of strategies based on assumptions that de-emphasize biological underpinnings for SUDs. Peter Monti and his colleagues have instead proposed a theory that substance use problems arise in large part due to deficits in coping skills. At its core, the treatment approach teaches a series of specific skills, typically in group settings. Sessions can readily be adapted for use in an individual therapy format if that is considered appropriate. Topics range from basic conversational skills to refusing drinks or drugs, managing criticism, and other social abilities. A list of the topics utilized in the Project MATCH Cognitive Behavioral Coping Skills component (discussed below) is presented in Table ** as an example. Relapse Prevention. Beginning in the 1980’s, Allen Marlatt colleagues began drawing attention to the rather high rates of relapse reported among individuals who had attended traditionally oriented treatment. Typically only about one out of three or even less individuals maintain abstinence following MMT program completion. More recent research has shown that return to use of alcohol or other drugs is the norm, rather that the exception, but has also shown that one or even a few episodes of use do not necessarily and inevitably lead to long term heavy usage. This runs contrary to a fundamental assumption of MMT, ultimately deriving from AA’s ideology, suggesting that a single drink will inevitably lead to a return to routine and regular heavy drinking. The high rates of relapse seen in MMT (and many other treatments, as well) can therefore be viewed as being in part an artifact of the dichotomous conceptualization of complete abstinence. Following this line of thinking, the individual who has a single drink, or even one or two nights of drinking after treatment, is considered equivalent to the person who immediately returns to persistent and heavy alcohol consumption. An important concept deriving from Marlatt’s work is the Abstinence Violation Effect, which is suggested to be a fundamental flaw in MMT. The extreme form of this argument is that MMT’s heavy emphasis on the importance of abstinence leads participants to conclude that having one drink or one episode of drug use equates to failure. Thus, the individual is left to assume that there is no point in Substance Use Disorders 11 continuing to work towards abstinence or any other treatment goal following a brief episode of using, and will consequently continue on to heavy use because all is already lost. Relapse prevention therapies seek, therefore, to provide alternative strategies for coping with episodes of relapse, as well as preventing relapse episodes from occurring at all. This is accomplished primarily through use of cognitive behavioral techniques. Motivational Interviewing (MI). The basic elements of motivational interviewing (MI) were introduced by psychologist William Miller in the early 1980s, and the concepts have been developed through two editions of the volume he co-wrote with Stephen Rollnick. Originally developed as an approach to working with addictive disorders, MI has been conceptually linked to Prochaska and De Clemente’s transtheoretical model of personal change, which proposes four basic stages of change: 1. Precontemplation, in which the individual does not recognize behavior as problematic, and therefore sees no need for change. 2. Contemplation, in which the individual recognizes that a problem exists although it is uncertain as to the source of the difficulty, and is not committed to personal change directed at addressing the problem. 3. Action, in which the individual fully acknowledges the need for change and is ready to or has already taken steps to achieve that. 4. Maintenance, in which the individual has accomplished significant change and is continuing actions to maintain or increase that level of change. The essential goal of MI is to assist individuals in moving from one stage to the next, in an effort to further personal commitment to behavior change in addressing problems. MI is at its core a Rogerian technique, but with a distinctly different slant. Heavy emphasis is placed on reflection, but the reflection is strategic in that the patient’s statements that are in favor of change are preferentially reflected, thus subtly encouraging the patient to make more of such statements. Another central component of MI is the recognition that ambivalence is an inevitable part of the change process; that is, one is extremely unlikely to wholeheartedly embrace change, especially early in the process. (For many of us, simply considering the desirability of loosing a few pounds – i.e., changing diet and/or exercise behaviors – is sufficient to illustrate this point). The person-centered approach of MI allows the therapist to not only avoid becoming involved in debate with the patient, but to capitalize on the ambivalence to reinforce change-oriented verbalizations and behaviors. Specific strategies include heightening contrast between desired goals and actual behaviors, and avoiding resistance by sidestepping and working around difficult issues rather than confronting them directly. This stands in marked contrast to the traditional MMT approach in which “resistance” is viewed as directly contrary to treatment goals, rather than as a normal part of the process of change. Which Is Best: Project MATCH. There has been considerable debate for many years concerning the superiority of one treatment approach over another, as well as the appropriateness of specific treatment goals. Such controversy has at times become quite heated, in that hallowed assumptions are sometimes at stake. A clear example is the acrimonious debate surrounding the controlled drinking versus complete abstinence as viable and worthwhile treatment goals. In the early 1990’s, Project MATCH was initiated, with its primary stated aim being the validation of specific individual attributes that would potentially make a person more suitable for one particular treatment approach over another. A total of 970 individuals were recruited from two different populations: (a) individuals who had recently completed some sort of inpatient treatment; and individuals recruited from the community to enroll in outpatient treatment. These patients were randomly assigned to one of three outpatient treatment conditions: 1. Motivational enhancement therapy, a series of four individual sessions based on principles of motivational interviewing. Substance Use Disorders 12 2. 12-Step facilitation, a series of five individual sessions designed to enhance a person’s participation in 12-Step support groups. 3. Cognitive behavioral treatment, a six session series of individual meetings deriving specific content material from the work of Monti and his colleagues (see above; also see Table 3). Each individual completed a lengthy test battery prior to starting the program, and interviews were conducted at regular intervals after completion. One of the most striking results of Project MATCH was the tremendous impact that treatment had on substance using behavior, regardless of the treatment conditions to which individuals were assigned; all three conditions showed marked improvement from baseline measures. In a sense this represented a failure, in that the expectation that individual attributes could be defined to aid in assigning individuals to treatment conditions was not met. On the other hand, the degree of reduction in substance use following application of any of the treatment conditions was quite striking. The primary exception to the notion of treatment improving substance use is in individuals showing more concurrent psychiatric disturbance. Specifically, as the level of psychiatric symptomatology increased, the effectiveness of the 12-Step facilitation therapy declined, but the relative effectiveness of cognitive behavioral therapy increased. Pending replication of this finding, the best conclusion is that treatment is often quite helpful, regardless of modality, but with patients who are displaying higher levels of concurrent psychiatric problems, greater reliance should probably be placed on cognitive behavioral strategies. A Dose of Reality. The treatment modalities defined in Project MATCH are, of course, rather rigidly defined as strategies relying upon a single theoretical approach. Outside of research settings, new treatment programs are to be found that are so narrow in their approach. As noted above, the large majority of treatment programs available in the United States are variants of an MMT approach. However, most programs today incorporate significant elements of cognitive behavioral skills training, including substantial components of relapse prevention, and MI is increasingly adopted as a general clinical strategy. Thus, there are, in fact, very few “pure” treatment programs to be found. Other important trends include the virtual disappearance of inpatient care, a dwindling number of residential facilities, a concomitant rise in the number of outpatient programs available, and an increase in awareness of the importance of longer stays in treatment. The later is particularly important for substances such as cocaine, which have proven to be particularly resistant to treatment, but is, of course, also strongly opposed by managed care companies. Conclusions Summary. Several points have been emphasized in this paper. These may be briefly summarized as follows: 1. SUDs affect a large proportion of individuals across the world, and represent the most commonly occurring mental health disorder in the U.S. SUDs are also the most common comorbid disorder. 2. When screening for SUDS, direct instruments are considerably more effective (not to mention less costly) than indirect tests. 3. Many forms of treatment have been developed over the years, with a plethora appearing in the past 50 to 75 years. It is perhaps surprising to learn that many of these, including 12-step selfhelp groups and MMT, have proven to be helpful for a large number of people. 4. AA or a similar self-help group represents a potentially valuable first line intervention. 5. Cognitive behavioral treatments have a generally good record, and available data suggest such approaches may be especially useful with patients who have concurrent psychiatric problems. 6. Psychology has generally not been well involved in treatment for SUDs. There are strong signs that this is changing, however, and more psychologists have greater interest in such issues. Substance Use Disorders 13 A Look Forward. In a 1997 American Psychologist article, William Miller and Sandra Brown argued strongly that psychologists should be actively involved in treatment of SUDs. They presented cogent evidence that psychologists are best prepared in terms of theoretical background, as well as clinical skills, to effectively manage such problems. It is striking that psychology has, for so many years, tended to overlook this series of disorders that affect such a substantial proportion of the American population, and especially those with whom psychologists are more likely to come into contact. At the same time, it is encouraging to see greater interest over the past several years, as evidenced by the creation of an APA division devoted to study of addictions, as well as an increasing number of papers and sessions at annual TPA conventions dealing with SUDs-related topics. Miller and Brown called for greater emphasis on SUDs in graduate training, an idea with which I wholeheartedly concur. I can only hope that this paper will encourage others to pursue further education and training in these areas. Substance Use Disorders 14 Table 1 A Classification of Drugs of Abuse SEDATIVES STIMULANTS OPIATES ALCOHOL Benzodiazepines (Valium, Xanax, Ativan, Serax, etc.) Barbiturates Amphetamines Cocaine Ritaline PPA (Phenylpropanalomine – a common ingredient in many overthe-counter diet and “energy” pill until outlawed several years ago Heroin Morphine Codeine Opium Methadone HALLUCINOGENS CANNABIS LSD Mescaline Peyote Marijuana Hashish DESIGNER DRUGS INHALANTS MDMA (Ecstasy) DMT, STP, etc. PCP (Angel Dust; note that much of what is sold on the streets as PCP is in fact any of several different substances, many of them quite toxic) Paints Glues Thinners and other Solvents Gasoline Amyl Nitrate Nitrous Oxide Freon Any of hundreds of other household products Substance Use Disorders 15 Table 2 Possible Interview Questions Frequency of drinking/drug use (days per week) Quantity per sitting Inquire about mixed drinks – sometimes contain more than one oz of alcohol Also inquire about “beers” – is patient referring to a standard 12 oz can, or possibly to a 40 oz container Ask how much patient drinks before feeling intoxicated (“How much do you have to drink to get a buzz?” Inquire about blackouts/episodes of memory loss (“Have you ever awakened in the morning and not remembered how you got home, or have you ever heard friends talking about things that happened at a party last night but you don’t remember?”) Inquire about prescription drug use – this may require multiple questions: Do you always take your prescription drugs as directed? Do you go to more than one physician to get prescriptions? Do you ever go to the emergency room to get additional medication? Do you ever obtain prescription drugs from friends or acquaintances? ALWAYS ask about suicidal ideation – substance abuse is a major risk factor for suicide Ask if patient has had legal problems of any sort – make list Ask specifically if there have been DWIs – if yes, inquire about results of breathalizer test Ask specifically about other possibly substance-related charges – e.g., Public Intoxication, Minor in Possession of Alcohol, Possession of Controlled Substance, etc. Is patient on parole or probation? Ask about marital or relationship problems – if yes, inquire about possible role of substance use Ask about employment problems – again, if yes, inquire about possible role of substance use Substance Use Disorders 16 Table 3 Possible Session Topics for Cognitive-Behaviorally Based Groups (From Project MATCH; Kadden et al., 1995) Basic Sessions: 1. Introduction to Coping Skills Training 2. Coping with Cravings and Urges to Drink 3. Managing Thoughts about Alcohol and Drinking 4. Problem Solving 5. Drink Refusal Skills 6. Planning for Emergencies and Coping with a Lapse 7. Seemingly Irrelevant Decisions Optional Sessions: 1. Starting Conversations 2. Nonverbal Communication 3. Assertiveness 4. Receiving Criticism 5. Awareness of Anger/Anger Management 6. Awareness of Negative Thinking/Managing Negative Thinking 7. Increasing Pleasant Activities 8. Managing Negative Moods and Depression 9. Enhancing Social Support Networks 10. Job-Seeking Skills 11. Family Issues Substance Use Disorders 17 Figure 1 Actuarial data (sensitivity versus sensitivity) for the MAST (circles) and MAC/MAC-R (triangles) Substance Use Disorders 18 References and Resources Information Outlets The National Institute on (NIAAA) publishes a good deal of literature on many aspects of alcohol problems, including, but by no means limited to, the Project MATCH series. Web address: http://www.niaaa.nih.gov/ The National Institute on Drug Abuse (NIDA) also offers a wide variety of materials, much of which is of value to clinicians. Web address is: http://www.nida.nih.gov/ NIAAA and NIDA materials can be obtained through the National Clearinghouse for Alcohol and Drug Information (NCADI) – it’s usually cheaper this way. http://www.health.org/ 1-800-729-6686 American Psychological Association, Division 50 – Addictions http://www.apa.org/divisions/div50 Important Journals Addiction Formerly the British Journal of Addiction, this journal often has a more medical focus Alcoholism: Clinical and Experimental Research A heavy emphasis on biological aspects of alcohol issues Alcohol Research & Health (formerly known as Alcohol Health & Research World) is a relatively inexpensive ($22 per year) publication that is useful in keeping abreast of developments in the field of alcohol research. It can be ordered by phone, using a credit card, by calling (202) 512-1800, between 8:00 a.m. and 4:30 p.m. eastern time, or by faxing a credit card order to (202) 512-2250. A printed order form, that can be mailed in, is also available. The most recent issues are also available online at: http://silk.nih.gov/silk/niaaa1/publication/aharw.htm Journal of Studies on Alcohol The oldest and probably most prestigious U.S. journal pertaining to addictions – with an obvious focus on alcohol Journal of Substance Abuse Treatment As the name suggest, primary emphasis on treatment issues Psychology of Addictive Behaviors The journal of APA’s Division 50 Papers are sometimes published in other psychology journals, e.g., American Psychologist, Journal of Consulting and Clinical Psychology, Psychological Bulletin, and others. There are also a number of other addictions journals – see: Arciniega, L. T., & Miller, W. R. (1997). Where to publish? Some considerations among English-language addiction journals. Addiction, 92, 1639-1648. Substance Use Disorders 19 General References Miller, W. R., & Brown, S. A. (1997). Why psychologists should treat alcohol and drug problems. American Psychologist, 52, 1269-1279. Washton, A. M. (2001). Why psychologists should know how to treat Substance Use Disorders. Originally published in New Jersey Psychologist; available online at: http://www.apa.org/ppo/issues/washton303.html Hester, R. K., & Miller, W. R. (Eds.) (2002). Handbook of alcoholism treatment approaches: Effective alternatives (3rd ed.). Boston, MA: Allyn & Bacon. Schuckitt, M. (1995). Drug and alcohol abuse: A clinical guide to diagnosis and treatment (5th ed.). New York: Plenum. Written by a psychiatrist – contains considerable medical information, including data on pharmacological effects of various drugs. Also has good summaries regarding symptoms produced by various substances, and how those symptoms mimic other mental disorders. New edition is due out this year. Leshner, A. I. (1997). Addiction is a brain disease, and it matters. Science, 278, 45-47. McCrady, B. S., & Epstein, E. E. (eds.). Addictions: A comprehensive textbook. New York: Oxford University Press. Lowinson, J., Ruiz, P., Millman, R. B., & Langrod, J. G. (eds.). Substance abuse: A comprehensive textbook (3rd ed.). Baltimore: Williams & Wilkins. NIAAA. (2000). 10th Special Report to the U.S. Congress on Alcohol and Health. Bethesda, MD: Author. Also available online at: http://silk.nih.gov/silk/niaaa1/publication/10report/10-order.htm Previous editions of the Special Report were published in 1997, 1994, etc. – unfortunately not available online, but useful as a comparative resource. NIDA. (1999). The Sixth Triennial Report to Congress From the Secretary of Health and Human Services Drug Abuse and Addiction Research: 25 Years of Discovery to Advance the Health of the Public. Bethesda, MD: Author. Also available online at: http://www.nida.nih.gov/STRC/STRCindex.html (1999). Alcohol Research & Health, 23(2), whole number. The entire issue of this journal was devoted to “Update on approaches to alcoholism treatment.” It is available online at: http://silk.nih.gov/silk/niaaa1/publication/aharw.htm Epidemiology Current data from ongoing projects such as the National Household Surveys on Drug Abuse and the Drug Abuse Warning Network (DAWN) are readily available through the SAMHSA website: http://www.samhsa.gov Cacciola, J. S., Alterman, A. I., McKay, J. R., & Rutherford, M. J. (2001). Psychiatric comorbidity in patients with substance use disorders: Do not forget Axis II disorders. Psychiatric Annals, 31, 321-331. Kessler, R. C., Nelson, C. B., McGonagle, K. A., Edlund, M. J., Frank, R. G., & Leaf, P. J (1996). The epidemiology of co-occurring addictive and mental disorders: Implications for prevention and service utilization. American Journal of Orthopsychiatry, 66, 17-31. Substance Use Disorders 20 Regier, D. A., Farmer, M. E., et al. (1990). Comorbidity of mental disorders with alcohol and other drug abuse: Results from the epidemiological catchment area (ECA) study. JAMA, 264(19), 2511-2518. Ross, H. E., Glaser, F. B., & Germanson, T. (1988). The prevalence of psychiatric disorders in patients with alcohol and other drug problems. Archives of General Psychiatry, 45, 1023-1031. Screening Allen, J. P., & Columbus, M. (1995). Assessing alcohol problems: A guide for clinicians and researchers. National Institute on Alcohol Abuse and Alcoholism, Treatment Handbook Series 4. Bethesda, MD: National Institute on Alcohol Abuse and Alcoholism. Babor, T. F., Steinberg, K., Anton, R., & del Boca, F. (2000). Talk is cheap: Measuring drinking outcomes in clinical trials. Journal of Studies on Alcohol, 61, 55-63. Babor, T. F., Stephens, R. S., & Marlatt, G. A. (1987). Verbal report methods in clinical research on alcoholism: Response bias and its minimization. Journal of Studies on Alcohol, 48, 410-424. Dawe, S., Loxton, N. J., Hides, L., Kavanaugh, D. J., & Mattick, R. P. (2002). Review of Diagnostic Screening Instruments for Alcohol and Other Drug Use and other Psychiatric Disorders (2nd ed.). Canberra, Australia: Commonwealth Department of Health and Ageing. Available online at: http://www.health.gov.au/pubhlth/publicat/document/mono48.pdf Donovan, D. M., & Marlatt, G. A. (1988). Assessment of addictive behaviors. New York: Guilford. Zanis, D. A., McLellan, A. T., & Randall, M. (1994). Can you trust patient self-reports of drug use during treatment? Drug and Alcohol Dependence, 35, 127-132. History, 12-Step Programs, and Minnesota Model Approaches Alcoholics Anonymous: The story of how many thousands of men and women have recovered from alcoholism (3rd ed.). (1955). New York: Alcoholics Anonymous World Services. Alcoholics Anonymous comes of age. (1957). New York: Alcoholics Anonymous World Services. Johnson, V. (1980). I’ll quit tomorrow. San Francisco: Harper & Row. Kurtz, E. (1991). Not-God: A history of Alcoholics Anonymous (expanded ed.). Center City, MN: Hazelden. McCrady, B. S., & Miller, W. R. (eds.) (1993). Research on Alcoholics Anonymous: Opportunities and alternatives. New Brunswick, NJ: Rutgers Center of Alcohol Studies. White, W. L. (1998). Slaying the dragon: The history of addiction treatment and recovery in America. Bloomington, IL: Chestnut Health Systems. Motivational Interviewing and Stages of Change A useful resource is the Motivational Interviewing website: http://www.motivationalinterview.org Connors, G. J., Donovan, D. M., & DiClemente, C. (2001). Substance abuse treatment and the stages of change: Selecting and planning interventions. New York: Guilford. Substance Use Disorders 21 Miller, W. R. (1985). Motivation for treatment: A review with special emphasis on alcoholism. Psychological Bulletin, 98, 84-107. Miller, W. R., & Rollnick, S. (2001). Motivational interviewing: Preparing people for change (2nd ed.). New York: Guilford. Prochaska, J. O, DiClemente, C. C., & Norcross, J. C. (1992). In search of how people change: Applications to addictive behaviors. American Psychologist, 47, 1102-1114. Velasquez, M. M., Gaddy-Maurer, G., Crouch, C., & DiClemente, C. C. (2001). Group treatment for substance abuse: A stage of change treatment manual. New York: Guilford. Project MATCH Some of the treatment manuals for Project MATCH have been referenced above, along with the NIAAA web site address. An executive summary, very readable and useful, is available at: http://www.niaaa.nih.gov/press/1996/match.htm. Babor, T. F., Miller, W. R., DiClemente, C., & Longabaugh, R. (1999). A study to remember: Response of the Project MATCH research group. Addiction, 94, 66-69. This is the Research Group’s responses to 14 commentaries on Project MATCH; the commentaries immediately preceded this paper. Carroll, K. M., Connors, G. J., Cooney, N. L., DiClemente, C. C., Donovan, D. M., Kadden, R. R., Longabaugh, R. L., Rounsaville, B. J., Wirtz, P. W., & Zweben, A. (1998). Internal validity of Project MATCH treatments: Discriminability and integrity. Journal of Consulting and Clinical Psychology, 66, 290-303. Project MATCH Research Group. (1993). Project MATCH: Rationale and methods for a multisite clinical trial matching patients to alcoholism treatment. Alcoholism: Clinical and Experimental Research, 17, 11301145. Project MATCH Research Group. (1997). Matching alcoholism treatments to client heterogeneity: Project MATCH posttreatment drinking outcomes. Journal of Studies on Alcohol, 58, 7-29. Project MATCH Research Group. (1998). Therapist effects in three treatments for alcohol problems. Psychotherapy Research, 8, 455-474. Project MATCH Research Group. (1998). Matching alcoholism treatments to client heterogeneity: Project MATCH three-year drinking outcomes. Alcoholism: Clinical and Experimental Research, 22, 13001311. Project MATCH Research Group. (1998). Matching patients with alcohol disorders to treatments: Clinical implications from Project MATCH. Journal of Mental Health UK, 7, 589-602. Velasquez, M. M., DiClemente, C. C., & Addy, R. C. (2000). Generalizability of Project MATCH: A comparison of clients enrolled to those not enrolled in the study at one aftercare site. Drug and Alcohol Dependence, 59, 177-182. Cognitive-Behavioral Approaches Beck, A. T., Wright, F. D., Newman, C. F., & Liese, B. S. (1993). Cognitive therapy of substance abuse. New York: Guilford. Substance Use Disorders 22 Kadden, R., Carroll, K., Donovan, D., Cooney, N., Monti, P., Abrams, D., Litt, M., & Hester, R. (1995). Cognitive-behavioral coping skills therapy manual. Project MATCH Monograph Series, Vol. 3. Rockville, MD: NIAAA. Monti, P. M., Abrams, D. B., Kadden, R. M., & Cooney, N. L. (1989). Treating alcohol dependence: A coping skills training guide. New York: Guilford. Controlled Drinking Denning, P. (2000). Practicing harm reduction psychotherapy: An alternative approach to addictions. New York: Guilford. Marlatt, G. A. (1998). Harm reduction: Pragmatic strategies for managing high risk behaviors. New York: Guilford. Miller, W. R., & Muñoz, R. F. (1982). How to control your drinking (Rev. ed.). Albuquerque: University of New Mexico Press. Sanchez-Craig, M. (1993). Saying when: How to quite drinking or cut down. Toronto, Canada: Addiction Research Foundation. Sobell, M. B., & Sobell, L. C. (1993). Problem drinkers: Guided self-change treatment. New York: Guilford. Solution-Focused Strategies Berg, I. K., & Miller, S. D. (1992). Working with the problem drinker: A solution-focused approach. New York: W. W. Norton. Miller, S. D., & Berg, I. K. (1995). The miracle method: A radically new approach to problem drinking. New York: W. W. Norton. Relapse Prevention The December, 1996 Supplement to the journal Addiction (Vol. 91) was devoted to issues related to relapse. Marlatt, G. A., & Gordon, J. R. (1985). Relapse Prevention: Maintenance Strategies in the Treatment of Addictive Behaviors. New York: Guilford. Dual Diagnosis Beeder, A. B., & Millman, R. B. (1997). Patients with psychopathology. In J. Lowinson, P. Ruiz, R. B. Millman, & J. G. Langrod (eds.), Substance abuse: A comprehensive textbook (3rd ed., pp. 551-563). Baltimore: Williams & Wilkins. Daley, D. C., Moss, H., & Campbell, F. (1987). Dual disorders: Counseling clients with chemical dependency and mental illness. Center City, MN: Hazelden. Evans, K., & Sullivan, J. M. (2001). Dual diagnosis: Counseling the mentally ill substance abuser (2nd ed.). New York: Guilford. Substance Use Disorders 23 Mueser, K. T., Noordsy, D. L., Drake, R. E., Fox L., & Barnes, K. H. (2003). Integrated treatment for dual disorder: A guide to effective practice. New York: Guilford Press. Rosenthal, R. N., & Westreich, L. (1999). Treatment of persons with dual diagnoses of substance use disorder and other psychological problems In B. S. McCrady & E. E. Epstein (eds.), Addictions: A comprehensive textbook (pp. 439-476). New York: Oxford University Press. Aversion Therapies Rimmele, C. T., Howard, M. O., & Hilfrink, M. L. (1995). Aversion therapies. In R. K. Hester & W. R. Miller (eds.) (1995), Handbook of alcoholism treatment approaches: Effective alternatives (2nd ed., pp. 134147). Boston, MA: Allyn & Bacon. Substance Use Disorders 24 Substance Use Disorders Name:__________________________________________________Degree________________ Mailing Address:_______________________________________________________________ City/State/Zip:___________________________________Phone:________________________ Email: ___________________________ Visa/MC#____________________________________________________ Security Code (3-digit code on signature panel): _________ Expiration: ________ Fees: Texas Psychological Association Members $45, Non-Members $65 Mail the test along with fee to the TPA Central Office, PO Box 1930, Cedar Park, TX 78630 or you can fax back to (512) 255-1642. Questions 1. Approximately ____ people in the United States have an active substance use disorder. a) 1 in 20 b) 1 in 5 c) 1 in 10 d) 1 in 3 2. Which of the following statements concerning Project MATCH is correct? a) Three different treatment modalities for SUDS were compared b) The initial goal was to identify characteristics that would be helpful in assigning individuals to particular treatment modalities c) It has been called the largest controlled therapy trial ever conducted d) It was conducted over multiple sites across the U.S. e) All of the above are true f) None of the above are true 3. Which of the following statements concerning psychology’s early involvement in substance abuse treatment is correct? a) Psychology has been actively involved in developing treatments for people with alcohol and other drug problems since the early 1900s b) SUDs have been a topic of some interest to psychologists for perhaps 15 to 20 years c) Some psychologists actively discouraged work with SUDs patients as little as 20 years ago d) A large number of papers pertaining to SUDs can be found in psychology journals prior to 1950 e) Both b) and c) are correct f) All of the above are correct 4. When screening for patients for SUDs a) Standardized tests are of no value b) A psychodynamic approach is most useful c) Indirect tests such as the MacAndrew scale of the MMPI/MMPI-2 are the most useful d) One can identify patients with SUDs solely on the basis of a direct test such as the MAST e) A useful approach is a direct test such as the MAST or the DAST, supplemented with a careful and thorough interview Substance Use Disorders 25 5. All of the following statements concerning comorbidity of DSM-defined disorders are true EXCEPT a) As many as 50% or more of patients with Schizophrenia have one or more comorbid SUDs b) SUDs are the most common comorbid disorder with other psychiatric disorders c) Alcohol dependent individuals are never really clinically depressed or have any other psychiatric disorder; all they need to do is stop drinking and the other “problems” will disappear d) Prolonged and heavy substance use will often produce symptoms that mimic many other psychiatric disorders e) Heavy alcohol use will cause depression that often clears within a few weeks of stopping drinking 6. Which of the following treatment modalities is generally seen as having only limited effectiveness in working with persons who have SUDs? a) Psychodynamic therapies b) Cognitive-behavioral therapies c) Aversion therapies d) Referral to AA or NA meetings e) Relapse prevention therapy 7. One of the more surprising findings from Project MATCH was a) On average, the severity of patients’ alcohol use declined markedly regardless of the treatment modalities to which they were assigned b) It was possible to identify specific factors predicting which patients would improve more in each of the three treatment conditions c) None of the three treatment modalities seemed to facilitate any significant changes in the drinking patterns of the patients assigned d) Patients assigned to the cognitive-behavioral treatment condition showed considerably greater change in drinking patterns compared to the other two conditions e) Patients assigned to the 12-Step facilitation treatment condition showed almost no change in their drinking patterns over the course of the program 8. Which of the following statements concerning Minnesota Model treatment (MMT) is INCORRECT a) MMT typically relies heavily on the so-called “Disease Concept” of substance dependencies b) MMT was originally based on AA principles, and incorporated regular attendance at AA meetings as an essential element c) Most MMT programs today run on an outpatient basis rather than the more traditional inpatient program d) MMT originated at the Betty Ford Center in California e) The first EAP programs were a direct outgrowth of some of the first MMT programs 9. The so-called “Disease Concept” of alcohol (and other drug-) dependency a) Typically ignores biological data such as studies on the heritability of alcohol dependence b) Argues that many individuals will be able to learn to control their drinking with suitable treatment c) Has as its core the beliefs that alcohol (and other drug-) dependency is chronic and progressive d) Lacks any sort of empirical support e) Is universally accepted by psychologists 10. Which of the following treatment modalities seems likely to be more effective when working with a patient who has a comorbid SUD and other psychiatric problems a) Psychodynamic therapies b) Cognitive-behavioral therapies c) Aversion therapies d) Referral to AA or NA meetings e) Relapse prevention therapy