Optical Coherence Tomography (OCT) [http://www.neec.com
advertisement

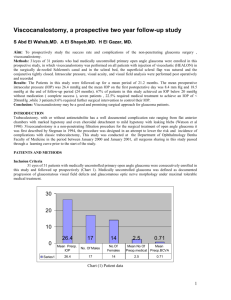
Optical Coherence Tomography (OCT) [http://www.neec.com/Glaucoma_OCT.html] Optical Coherence Tomography, or OCT, is a noncontact, noninvasive imaging technique used to obtain high resolution cross-sectional images of the retina. OCT is analogous to ultrasound B-scan imaging except that light rather than sound waves are used in order to obtain a much higher longitudinal resolution of approximately 10µm in the retina. OCT has been shown to be clinically useful for imaging selected macular diseases including macular holes, macular edema, age-related macular degeneration, central serous chorioretinopathy, epiretinal membranes, schisis cavities associated with optic disc pits, and retinal inflammatory diseases. In addition, OCT has the capability of measuring the retinal nerve fiber layer thickness in glaucoma and other diseases of the optic nerve. Goldmann perimetrie OD: Blinde vlek tussen 10 en 20 graden rechts. DCSI Introduction Deep sclerectomy with collagen implant (DSCI) is a non-perforating filtering procedure used for the surgical treatment of medically uncontrolled open-angle glaucoma. Deep sclerectomy with collagen implant has been developed by Koslov and colleagues in Moscow and aims at decreasing the complications of standard trabeculectomy such as hyphaema, inflammation of the anterior chamber, excessive filtration leading to hypotony, shallow or flat anterior chamber, choroidal detachment and endophthalmitis (1-3). With DSCI, the filtration of aqueous humor from the anterior chamber to the subconjunctival space occurs through a thin trabeculo-descemetic membrane representing the posterior and anterior trabeculum and 1 mm of a limbal Descemet's membrane (Fig. 1). This membrane offers a moderate but constant and reproducible resistance to aqueous outflow and avoids the sudden intraocular pressure drop often seen during trabeculectomy. Deep sclerectomy creates a scleral chamber from which aqueous humor flows to the subconjunctival filtering bleb and eventually to the Schlemm's canal, and maybe intrascleral aqueous veins (4-5). To keep the scleral space patent, a resorbable collagen implant is used. Fig. 1: Schematic representation of the deep sclerectomy dissection and the trabeculodescemetic membrane. Surgical Technique DSCI is usually performed under retrobulbar anaesthesia, but may be performed using topical anaesthesia. A traction suture is placed in the superior rectus muscle for adequate exposure of the deep sclerectomy site. The conjunctiva and Tenon's capsule are opened in the upper fornix. Careful haemostasis of the exposed sclera using wetfield cautery is performed and approximately a 1/3 scleral thickness limbal-based scleral flap measuring 5x5 mm is dissected. This superficial scleral flap is dissected 1 mm into clear cornea anteriorly. Then a limbal-based triangle of deep sclera is removed, leaving a thin layer of sclera over the choroid and the ciliary body. Anteriorly, the dissection is performed down to the Schlemm's canal. The canal is unroofed, and more anteriorly the excision of corneal stroma is performed down to Descemet's membrane. At this stage of the procedure, aqueous humor is percolating through the thin trabeculo-descemetic membrane. The cylindrical collagen Implant (Staar Surgical AG, Nidau, Switzerland) is placed radially in the center of the deep sclerectomy site and sutured with a single 10/0 nylon suture (Fig. 2). The superficial scleral flap is then repositioned over the collagen implant and sutured with two untied 10/0 nylon sutures. Finally, the Tenon's capsule and conjunctiva are closed with a running 9/0 vicryl suture. Postoperatively the patients are treated with antibiotics and steroids 3 times a day for a week to 10 days, followed by a non-steroidal anti-inflammatory drug 3 times a day for 3 months (Fig. 3). NPDS [http://www.augenchirurgie.ch/Vortraege/perforation.htm] To successfully reduce the intraocular pressure (IOP) with the non-perforating deep sclerectomy depends on the opening of Schlemm's canal, and on exposing the Descemet's membrane as thin as possible. Only this allows enough intraocular fluid to filtrate into the scleral pocket and reach the deep scleral vein system. With this type of exposure perforations into the anterior chamber are sometimes unavoidable. With a Healon 5 cushion underneath the tightly sutured upper scleral flap one can prevent the iris from protruding through the site of perforation. This makes an iridectomy unnecessary. Also, an immediate postoperative IOP-drop can be avoided in most cases. The postoperative pressure follow-up does not differ from successfully performed non-perforationg deep sclerectomies. 90% of the cases with perforation do not develop a conjunctival filtering bleb. I find it better to risk a perforation into the anterior chamber than to be overly careful in exposing a membrane that is too thick to allow filtration. The postoperative IOP data is presented in this paper. [http://www.escrs.org/eurotimes/December%202001/excimer.asp] Excimer Laser Achieves Precisely Controlled Deep Sclerectomy By Roibeard O’hEineachain BUENOS AIRES-Performing deep sclerectomy with an excimer laser and implanting a collagen drainage device can provide glaucoma patients with stable IOP control without hypotony and other early post-operative complications that can occur with trabeculectomy procedures, said Ana Sanseau, MD, Instituto de la Vision, and Hospital de Clinicas “Jose de San Martin,” School of Medicine, University of Buenos Aires, Argentina. “This method allows an effective IOP decrease involving little disruption of the patients daily life. Unroofing the Schlemm’s canal with the excimer laser in non-penetrating glaucoma surgery is a new non- perforating procedure which enables precise and homogeneous ablations of scleral tissue, and avoids the risk of perforations of the trabeculo-Descemet's membrane. The absence in our study of post-operative complications reported with trabeculectomy is remarkable,” Dr. Sanseau she presented her findings at the First International Congress on Non-penetrating Glaucoma Surgery in Lausanne, Switzerland. In 20 glaucoma patients who underwent the excimer laser-assisted deep sclerectomy procedure, IOP ranged from 21- 25 mmHg with medications before treatment, while after treatment with a mean follow up of 24 month (range 1 5-29 months) it ranged from 12 to 20 mmHg without medications. Eleven patients required a YAG laser to open the trabeculo-descemetic membrane to reach a lower IOP in the first four weeks after surgery. All the patients in the study had open angle glaucoma with mild-to-moderate damage in the optic nerve and visual field, or poor lOP control with more than one medication. All underwent a complete ophthalmic examination before surgery. After surgery anatomic changes were examined by UBM and the anterior chamber depth and the angle in degrees were also measured. Dr. Sanseau and her associates performed all of the surgeries under peribulbar anaesthesia with bupivacaine, xylocaine and hyaluronidase. They commenced each procedure by placing a suture at twelve o’clock through the cornea and then creating a fornix-based conjunctival flap. Then, after performing careful haemostasis using a wetfield cautery, they delineated and dissected a superficial 4-5 mm flap with a diamond blade calibrated to a depth of 400 mm and advanced 2 mm into the clear cornea. Precisely Controlled Scleral Ablation The Buenos Aires team then ablated the sclera with a 117 Chiron Technolas Excimer Laser with a 193 nm wavelength and a fluence of 160 mJ using a program from Bausch & Lomb Surgical that determines the width and depth of the ablation, she explained, adding: “The first sequence of pulses ablates 100 mm and then it has seven additional sequences of pulses that ablate 20 mm per sequence. We rotate the eye downward to ensure a correctly vertical entry of the laser beam. The laser beam works over the area creating a square figure in a controlled way, which reduces the risk of anterior chamber perforation. “The surgeon can check between sequences of laser pulses for any aqueous humour filtration through the opened Schlemm’s canal. When the aqueous humour begins to percolate through the trabeculo-Descemet’s membrane, the ablation is stopped. Only the external wall of the Schlemm’s canal is opened, leaving most of the trabecular meshwork intact and thereby preventing anterior chamber shallowing.” Once the scleral ablation was completed Dr. Sanseau and her associates implanted a collagen device (STAAR) which they secure in place with a single 10.0 bite nylon suture. They then re-positioned the scleral flap over the implant and closed it with 2 or 5 nylon sutures, and buried the knots. They concluded the procedure by closing the conjunctiva and Tenon’s capsule with two interrupted 8.0 silk sutures. Patients received topical antibiotics and corticosteroids for three weeks after surgery. “The most difficult step in non-penetrating surgery is the ablation of the deep scleral bed. The major advantage of this procedure is that it induces a progressive filtration of aqueous humour through a homogeneous trabeculo-Descemet’s membrane under direct vision. The depth of the internal ablation by the excimer laser is controlled, thus avoiding perforation and prevents sudden post-operative hypotony. Moreover, the success rate is improved with the addition of a collagen device, she concluded. Dr. Sanseau’s co-authors were Carlos Argento, MD, and Javier Casiraghi, MD, also at the University of Buenos Aires. More details of their preliminary findings with excimer laser-assisted deep sclerectomy technique appeared in the April 2001 issue of the Journal of Cataract and Refractive Surgery (27:504-506). [www.bog-sbo.org/bulletin/280_03.pdf] All procedures were performed according to the Kozlov's and Mermoud's technique. In all cases, a 9-0 superior peripheral corneal traction vicryl was used. A limbus-based conjunctival flap was dissected superiorly and the sclera was exposed. A one third scleral thickness limbus based scleral flap measuring 5×5 mm was dissected anteriorly into clear cornea for about 1,5 mm. A second triangular deep scleral flap was then dissected leaving only a very thin layer of deep sclera over the choroid. Anteriorly, the dissection was carried down to unroof and remove Schlemm's canal and juxtacanalicular trabeculum. More anteriorly, the excision of corneal stroma was carried down to Descemet's membrane. At this stage of the procedure, aqueous humor was seen to percolate through the thin remaining trabeculo-Descemetic membrane. After excision of the deep triangular scleral flap, a triangular 3,5×3,5 mm SKGEL t implant (COR- NEAL t , Paris, France) was placed in the center of the deep sclerectomy dissection site. The rectangular superficial scleral flap was then repositioned over the SKGEL t implant and closed with 10-0 monofilament nylon sutures with buried knots. The conjunctiva and Tenon capsule were carefully closed with a running 10-0 Biosorb suture. Postoperative management included topical treatment with dexamethasone 0,1%, geomycine three times daily for 3 to 4 weeks and then with topical diclofenac sodium three times a day during the next following month. If the filtering bleb showed signs of failure, subconjunctival injections of 5 mg of 5-FU were given into the inferior fornix or in the vicinity to the bleb. These injections were repeated up to 7-8 times. Argon laser suture lysis was also performed when needed in order to improve the filtration. Goniopuncture with Nd:YAG laser was performed at the site of surgery through the trabeculo-Descemetic membrane when failure with raised IOP was documented. [http://www.revoptom.com/special.asp?page=osc/feb02/glaucoma.htm] Trabeculectomie Laser trabeculoplastie (LTP) Cyclodestructie In more than 95 percent of glaucoma cases in the United States, the first-line of therapy is medication.1 Surgery is usually considered necessary only when patients are refractive to treatment with medications or are unable to follow the treatment protocol. There also are a few patients who may prefer surgery to medications. In these cases, ophthalmologists have several options available to them for reducing IOP, such as trabeculectomy, laser trabeculoplasty, nonpenetrating filtering surgery and shunts. This article reviews some of the common surgical techniques used for reducing intraocular pressure in glaucoma patients. Filtration Surgery Traditionally, the most common surgical procedure for treating glaucoma has been trabeculectomy, or guarded filtration. In this procedure, the surgeon typically removes a piece of the cornea or sclera, creating a pathway for aqueous fluid to leave the eye. The aqueous fluid exits the anterior chamber and pools in a reservoir under the eyelid where it is gradually absorbed by large veins in the eye's orbit. The result is a reduction in IOP. The reservoir, or bleb, covers the flap-type filtration opening into the eye. Over time, however, it may heal over and close up, resulting in a loss of surgical benefit. In addition to bleb failure, this procedure is also associated with a significant risk for hypotony, hyphema and choroidal effusion or hemorrhage. Antifibrotic agents such as 5-fluorouracil or mitomycin C have been routinely used in low-risk eyes undergoing primary trabeculectomy to help prevent the newly created bypass from closing by scar formation.2 In a retrospective study of patients undergoing combined cataract and glaucoma surgeries, those who had received intraoperative MMC or postoperative subconjunctival 5-FU had greater reductions in IOP levels than those who were not treated with these agents.3 However, the use of 5-FU or MMC as adjuncts to glaucoma surgery may result in the production of thin, avascular blebs and additional complications, including hypotony, endophthalmitis, wound leakage and late-onset infection.4,5 Attempts to optimize antifibrotic treatment have led to the use of low-dose MMC for 2 minutes intraoperatively or postoperative subconjunctival 5-FU.6,7 Alternative wound healing modulators, such as corticosteroids, cytokines and fibrinolytic agents, are also used or are being developed as adjuncts to filtration surgery.4 Trabeculectomy, alone or in combination with medical therapy, has a success rate approaching 95 percent at two years in patients with previously unoperated eyes.8-10 Although long-term control can often be achieved with filtering surgery, many patients require additional therapy. Repeat trabeculectomies have a much lower success rate.10-12 Laser Trabeculoplasty In recent years, laser surgery has gained increasing popularity as an intermediate step between drugs and traditional surgery. Laser trabeculoplasty is one of the most commonly performed glaucoma procedures. The procedure involves creating tiny laser burns around the trabecular meshwork to increase aqueous fluid outflow. When used as the initial treatment of previously unoperated eyes, laser trabeculoplasty results in a clinically significant reduction in IOP in more than 75 percent of patients.13 Although argon lasers (blue-green to green wavelength) are most commonly used for this procedure, laser trabeculoplasty has been successfully performed with yellow (tunable dye), red (krypton) and near-infrared (diode and neodymium:YAG) wavelengths. In a 10-year retrospective follow-up study after argon laser trabeculoplasty, failure was most common after one year (23 percent) and occurred at rates of 5 to 9 percent per year thereafter. 14 Because bleb formation does not occur with laser trabeculoplasty, this procedure is associated with fewer complications than trabeculectomy. Risks associated with laser trabeculoplasty are minor and include post-operative inflammation, IOP spikes and worsening of glaucoma due to membrane formation in the chamber angle.15 Selective laser trabeculoplasty is a relatively new technique that selectively targets trabecular meshwork cells using a Q-switched frequency-doubled Nd:YAG laser.16 Unlike conventional argon laser trabeculoplasty, the new method does not cause thermal or coagulative damage to the trabecular meshwork.17 Because it is associated with minimal tissue damage, SLT is potentially repeatable.18 In a randomized study comparing ALT or SLT as a second procedure after a failed prior ALT procedure, IOP reduction was better after SLT than repeat ALT.19 Laser trabeculoplasty rarely reduces the amount of medical treatment necessary to manage glaucoma, and its effects are generally not long-term. Most patients are unable to reduce the number of drops they are taking following laser trabeculoplasty. Results from long-term studies found that up to 50 percent of treated eyes require additional surgical treatment within five years. 20-23,14 Repeat trabeculoplasty has a low long-term rate of success in those patients whose eyes have lost previous adequate response, with failure occurring in nearly 90 percent of these eyes within two years.24-28 For these reasons, many ophthalmologists prefer to use medications as the first-line of therapy. Laser trabeculoplasty can be thought of as one of the many therapeutic modalities that can be added to a patient's existing arsenal of therapies. Nonpenetrating Filtering Surgery Nonpenetrating filtering surgery is a similar procedure to trabeculectomy except that the sclera is not penetrated. Instead, a thin membrane is created under the scleral flap without entering the eye. The membrane acts as an outflow resistance site, preventing the IOP from dropping too low and causing the anterior chamber to deflate. Nonpenetrating surgeries are divided into two groups: bleb-forming surgeries and viscocanalostomy. Bleb-forming surgeries include ab externo trabeculectomy and deep sclerectomy. In AET, the surgeon removes the inner wall of Schlemm's canal and the juxtacanalicular trabeculum, leaving a thin membrane. In deep sclerectomy, the corneal stroma behind the anterior trabeculum and Descemet's membrane are removed, and in some cases, the surgeon may employ an implant to support the bleb. Viscocanalostomy involves removing a deep piece of scleral tissue along with part of the trabecular meshwork and anterior Schlemm's canal wall. The aqueous fluid percolates through an intact Descemet's window without connecting to the anterior chamber. Because the superficial scleral flap is tightly closed, there is little or no bleb formation. This procedure reduces the risk of postoperative infection and the need for antimetabolites. Some of the disadvantages of viscocanalostomy include: the continued elevation of IOP for as long as one month postoperatively; the length of the surgical procedure relative to standard trabeculectomies; the large scleral flap that reduces the amount of superior conjunctiva available for additional surgeries; and the lack of durability of the results. Because of these problems, viscocanalostomy is not recommended for patients with low- or normaltension glaucoma. When compared with trabeculectomy, nonpenetrating deep sclerectomy was found to be less effective in lowering the IOP in one trial (n=34 eyes), whereas the two procedures were equally effective in another trial (n=78 eyes).29,30 Both of these studies showed that nonpenetrating surgery was associated with the fewest complications. In a study comparing viscocanalostomy with trabeculectomy, none of the 10 patients randomized to treatment by viscocanalostomy achieved successful reductions in IOP over a six-month period, compared to a 50 percent success rate after trabeculectomy. 31 Tube Shunts In cases where there is inflammation, excessive scarring from previous glaucoma surgeries or unusual healing, it may be necessary to insert an aqueous shunt. In this procedure, a tiny plastic tube is routed from the anterior chamber of the eye to a reservoir--a plate placed halfway back around the eye--which prevents the conjunctiva from fastening to the wall of the eye and preventing drainage. Aqueous fluid drains through the tube to the top of the plate where it is absorbed by the blood vessels around the eye. Potential complications of tube shunt implantation include tube contact with the cornea or the lens, which may cause localized damage. If the tube comes in contact with the lens, small localized cataracts may result. In rare instances, the tube may erode through conjunctiva covering it. When this happens, the only option is surgical repair. In a randomized clinical trial comparing the Ahmed glaucoma valve implant with trabeculectomy, the implant group had higher IOPs during a 10-month follow-up.32 In study of two-year outcomes after implantation of 350-mm Baerveldt glaucoma shunts, the success rate was 81 percent for open-angle glaucoma patients and the overall study population reduced their glaucoma medication use from 2.5 mean preoperative medications to 0.8 postoperative medications (68 percent).33 Cyclocoagulation Cyclocryocoagulation and cyclophotocoagulation are procedures that treat dangerously high IOP in patients who have failed conventional filtration surgery or have a poor predicted outcome. Although few specialists perform cyclocryocoagulation procedures any longer, diode laser cyclophotocoagulation is gaining acceptance as a therapy for end-stage or refractory glaucoma.34-38,13 Cyclocoagulation procedures use a specialized probe to freeze or photodynamically ablate part of the ciliary body, thus inhibiting the production of aqueous fluid. The goal is to equalize the amount of fluid produced by the ciliary body with the amount of fluid that is drained from the eye. Although this procedure is noninvasive, outcomes are less predictable and the risks are greater than for other surgical modalities. Common complications include postoperative pain, hypotony, marked inflammation of internal and external eye structures, reductions in visual acuity, choroidal detachment and atrophy. The need for multiple procedures is common, as well. Some of the patients (8 percent at one year and 12 percent at four years) do not produce enough fluid, which leads to a condition in which the eye becomes too soft and may result in visual impairment or loss. Investigational Techniques Surgical techniques that are being developed for glaucoma treatment include microendoscopic approaches to trabeculectomy using laser technology and fiberoptic delivery, microcurettage (goniocurretage), or trabecular aspiration.39 Goniocurettage is a procedure in which pathologically altered trabecular meshwork is removed endoscopically by microcurettage to increase aqueous fluid outflow. 40 The short-term outcome of this technique compares well with ALT. In trabecular aspiration the tissue is removed with a vacuum aspiration device.41 When used to treat patients with pigment dispersion syndrome or pigmentary glaucoma, trabecular aspiration failed to achieve long-term control of IOP in either group.39 Other new techniques involve microtube shunts or adjunct treatments that modify wound healing. 4 A monoclonal antibody direct against transforming growth factor-ß (TGF-ß) has been shown to improve glaucoma filtration surgery outcomes.39 Angiogenesis inhibitors and agents affecting fibroblast migration and extracellular matrix synthesis are also under investigation as aids to maintaining bleb formation after filtration surgery. Despite recent advances in surgical techniques for treating glaucoma, the preferred first line of therapy in the United States is medical treatment. Surgical intervention is generally reserved for patients who are refractive to medical therapy or who are unable to follow the treatment protocol. Surgical techniques available to ophthalmologists for reducing IOP in glaucoma patients include trabeculectomy, laser trabeculoplasty, nonpenetrating filtration surgery and shunts. However, these procedures do not usually provide permanent IOP control. Patients treated surgically must often undergo additional procedures and/or take medications to maintain IOP control. Figure 1: The removal of the inner block during trabeculectomy. Figure 2: An established filtering bleb four months after a trabeculectomy. Figure 3: Various tube shunt types: Ahmed, Baerveldt, Krupin, Molteno. Figure 4: A tube tip within the anterior chamber.