shortness mg
advertisement

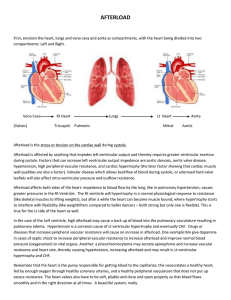
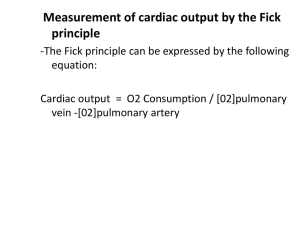
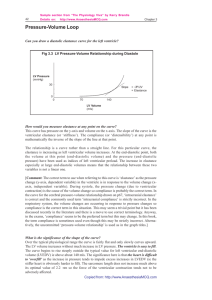
1. The hemodynamics indicate cardiogenic shock . Which hemodynamic values reflect this? What is status of preload and afterload? What medications can be given to manage the preload and afterload?: 1. Professors Response: The hemodynamics indicate cardiogenic shock, with decreased cardiac output increased preload and afterload. Management of all three parameters is needed. Preload can be decreased with venous vasodilators and diuretics. Afterload can be decreased with arterial vasodilators. Nitroprusside will vasodilate both venous and arterial beds. Nitroglycerine may be added as a venovasodilator. Contractility can be increased with dobutamine, dopamine or amrinone. Dopamine may increase afterload, whereas dobutamine and amrinone will increase contractility and may also cause vasodilation. 2. If medications are ineffective in managing preload and afterload, what mechanical device might be used and how would it improve cardiac output?: 2. Professors Response: If these measures are not effective, an intra-aortic balloon pump will decrease left ventricle workload by decreasing afterload and increase coronary artery blood flow. 3. Mr.G. improves and is discharged from the hospital; however, he returns to the hospital ED within 10 days with a diagnosis of heart failure. He states that I can t catch my breath and my legs are as big as tree trunks and I have pain on my right side . On assessment you find that he is strictly following the fluid and salt restriction ordered since recent hospital admission but still reports that he has been gaining 1 to 2 pounds every day since discharge. He states that he takes the following medications: Enalapril (Vasotec) 5 mg bid, digoxin 0.125mg qd, furosemide 40 mg qd; potassium chloride 20 mEq qd. The admitting physician orders all the medications but changes the furosemide to 40 mg intravenous push (IVP) qd and 80 mg IVP now. What error in teaching most likely occurred when Mr.G. was discharged 10 days ago? : 3. Professors Response: He was not instructed when to call with early weight gain, thus leading to current ER visit. Patients need to be instructed when to call their provider after being discharged from the hospital for exacerbated heart failure. Complete selfmanagement patient education is considered a standard of care and is mandated by the Joint Commission on Accreditation of HealthcareOrganizations (JCAHO) when providing care to hospitalized patients. The goal of the discharge treatment plan is to minimize symptoms and prevent readmission. 4. Most heart failure admissions are related to fluid volume overload. Patients who do not require intensive care monitoring can most often be treated initially with IVP diuretics, oxygen, and angiotensin converting enzyme (ACE) inhibitors. What is the rationale for giving the furosemide IVP? How will you evaluate its effectiveness?: 4. Professor's Response: Mr.G s is fluid overloaded and needs to decrease fluid volume in a short period. IV administration is delivered directly into the vascular system, where it can start to work immediately. In congestive heart failure (CHF), blood flow to the entire gastrointestinal system is compromised; therefore the absorption of orally ingested medications may be variable and take longer to work. You administer 80 mg furosemide IVP; evaluate its effectiveness by: _ Daily weight _ Intake and output _ Decreased dependent edema _ Decreased shortness of breath 5. How do ACE inhibitors help in CHF?: 5. Professor's Response: ACE inhibitors prevent the conversion of angiotensin I to angiotensin II, a potent vasoconstrictor. This results in systemic vasodilation, thereby reducing preload (reducing the volume of blood entering the left ventricle [LV]) and afterload (reducing the resistance to the left ventricular contraction) in patients in CHF. 6. Why was Mr.G. receiving receiving digoxin and potassium?: 6. Professor's Response: Digoxin improves cardiac output by improving myocardial contractility; monitor potassium levels carefully, hypokalemia can lead to digitalis toxicity. 7. How would you classify Mr.G s heart failure? What lab studies would you expect to be done?: 7. Professor's Response: Mr. G is evidencing symptoms of both right and left-sided heart failure: right-sided (lower extremity edema, JVD, abdominal discomfort (hepatomegaly); left-sided heart failure: dyspnea, tachycardia, crackles, fatigue and probably an S3 can be heard. Chest x-ray to show heart enlargement, Echocardiogram to show decreased ventricular function and decreased EF, elevated liver function studies, elevated BUN and creatinine, elevated prothrombin time (liver congestion impairs livers ability to synthesize procoagulants, BNP elevated; EKG show hypertrophy, ischemic changes, tachycardia and arrhythmias. 8. Mr.G is ready for discharge. What key management concepts should be taught to prevent relapse and another admission?: 8. Professor's Response: The most essential aspect of teaching hospitalized patients without overloading them is to focus on realistic key points. Teaching should be aimed at tips to improve symptoms and prevent readmission. The five most important concepts for patients with heart failure are included in MAWDS instructions. _ Medications take as directed, don t skip a dose, and do not run out of medications. _ Activity stay as active as you can while limiting your symptoms. _ Weight weigh every morning, call if you gain or lose 2 pounds overnight or 5 pounds from your target weight. _ Diet follow a low-salt diet and limit fluids to less than 2 quarts/liters per day. _ Symptoms know what symptoms to report to your provider; report early to prevent readmission.