Team Charter - Safe Surgery Collaborative draft 3 jan 23, 2011
advertisement
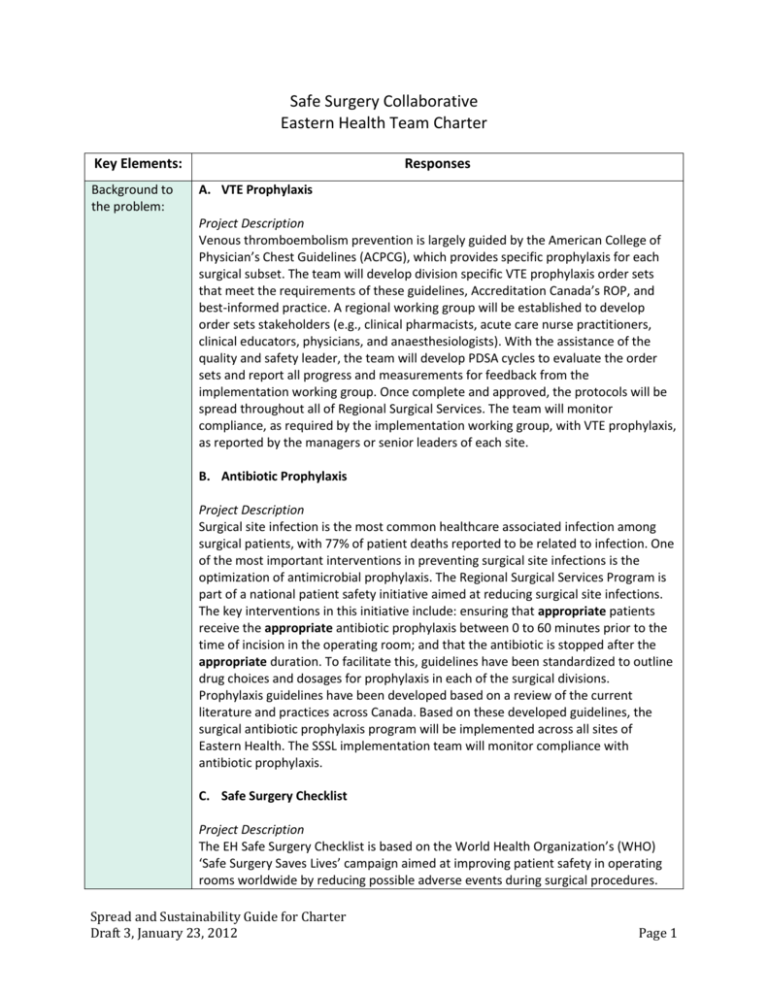
Safe Surgery Collaborative Eastern Health Team Charter Key Elements: Background to the problem: Responses A. VTE Prophylaxis Project Description Venous thromboembolism prevention is largely guided by the American College of Physician’s Chest Guidelines (ACPCG), which provides specific prophylaxis for each surgical subset. The team will develop division specific VTE prophylaxis order sets that meet the requirements of these guidelines, Accreditation Canada’s ROP, and best-informed practice. A regional working group will be established to develop order sets stakeholders (e.g., clinical pharmacists, acute care nurse practitioners, clinical educators, physicians, and anaesthesiologists). With the assistance of the quality and safety leader, the team will develop PDSA cycles to evaluate the order sets and report all progress and measurements for feedback from the implementation working group. Once complete and approved, the protocols will be spread throughout all of Regional Surgical Services. The team will monitor compliance, as required by the implementation working group, with VTE prophylaxis, as reported by the managers or senior leaders of each site. B. Antibiotic Prophylaxis Project Description Surgical site infection is the most common healthcare associated infection among surgical patients, with 77% of patient deaths reported to be related to infection. One of the most important interventions in preventing surgical site infections is the optimization of antimicrobial prophylaxis. The Regional Surgical Services Program is part of a national patient safety initiative aimed at reducing surgical site infections. The key interventions in this initiative include: ensuring that appropriate patients receive the appropriate antibiotic prophylaxis between 0 to 60 minutes prior to the time of incision in the operating room; and that the antibiotic is stopped after the appropriate duration. To facilitate this, guidelines have been standardized to outline drug choices and dosages for prophylaxis in each of the surgical divisions. Prophylaxis guidelines have been developed based on a review of the current literature and practices across Canada. Based on these developed guidelines, the surgical antibiotic prophylaxis program will be implemented across all sites of Eastern Health. The SSSL implementation team will monitor compliance with antibiotic prophylaxis. C. Safe Surgery Checklist Project Description The EH Safe Surgery Checklist is based on the World Health Organization’s (WHO) ‘Safe Surgery Saves Lives’ campaign aimed at improving patient safety in operating rooms worldwide by reducing possible adverse events during surgical procedures. Spread and Sustainability Guide for Charter Draft 3, January 23, 2012 Page 1 This checklist does not replace existing procedures or safety checks, but builds on them to ensure the entire interdisciplinary team is involved in the safety communication at three critical points: before the induction of anaesthesia (Briefing), before skin incision (Time Out), and before the patient leaves the OR (Debriefing). The team will develop a checklist prior to implementation that meets the requirements of Accreditation Canada Required Organizational Practice, AHS Safe Surgery Checklist manual, and the WHO 10 essential objectives for safe surgery. This checklist will be adapted to suit the needs and responsibilities of current surgical services at each of the sites. The adapted checklist will have input from key stakeholders. With the assistance of the clinical quality and safety leader, the team will develop PDSA cycles to evaluate the adapted checklist. Full implementation of the safe surgery checklist (developed and approved) will be instituted by June 2012. Compliance rates and process and outcome measures will be monitored. Statement of the problem: AIM for improvement: What are we trying to accomplish? Goal #1: To decrease the number of surgical site infections. Goal #2: To decrease the number of preventable VTE events within Regional Surgical Services. Goal #3: The operating room will reduce the number of preventable surgical complications and further improve surgical outcomes for patients. Scope A. VTE Prophylaxis In-Scope 1. Communicate and educate all Regional Surgical Services staff regarding VTE prophylaxis. 2. Support and endorse the use of VTE prophylaxis order sets. 3. Provide role modeling and positive peer influence to colleagues. 4. Report concerns and problems associated with the initiative to the Quality and Safety Leader and/or Eastern Health Safe Surgery Saves Lives Implementation Team. Out-of-Scope 1. Obstetrics and pediatrics. Dependencies on Other Projects and/or Initiatives 1. The Eastern Health VTE Steering Committee is currently working on a global policy and implementation plan for Eastern Health. 2. Will require resources (e.g. identification of staff) to collect and analyze outcome and process measures. 3. EH SSSL implementation team will develop a plan and distribute to all sites 4. Evidence of VTE events will be obtained through review of CSRS electronic Spread and Sustainability Guide for Charter Draft 3, January 23, 2012 Page 2 reporting system reports. 5. Support the use of posters and other promotional material. B. Antibiotic Prophylaxis In-Scope 1. Communication and education of all Regional Surgical Services and Children and Women’s Health staff and physicians regarding Antibiotic Prophylaxis. 2. Support and endorse the use of antibiotic prophylaxis guidelines. 3. Provide role modeling and positive peer influence to colleagues. 4. Report concerns and problems associated with the initiative to the Quality and Safety Leader and/or Eastern Health Safe Surgery Saves Lives Implementation Team. 5. Develop, approve, and implement pediatric guidelines for antibiotic prophylaxis. Out-of-Scope Dependencies on Other Projects and/or Initiatives 1. Will require resources (e.g. identification of Infection Prevention and Control practitioner) to collect and analyze surgical site infection outcome and process measures. 2. EH SSSL implementation team will develop plan and distribute to all sites. 3. Support the use of posters and other promotional material. C. Safe Surgery Check List In-Scope 1. Communication and education of all OR staff and physicians regarding Safe Surgery Checklist. 2. Support and endorse the use of an Eastern Health Safe Surgery Checklist. 3. Provide role modeling and positive peer influence to colleagues. 4. Report concerns and problems associated with the checklist to the quality and safety leader and/or Eastern Health Safe Surgery Saves Lives Implementation Team. Out-of-Scope Dependencies on Other Projects and Initiatives 1. EH SSSL implementation team will develop a plan and distribute to all sites. 2. Evidence of near miss events and occurrences will be obtained from review of reports from CSRS electronic reporting system. 3. Will require resources (e.g. identification of staff) to collect and analyze audit process and outcome measures. 4. Support the use of posters and other promotional material. Spread and Sustainability Guide for Charter Draft 3, January 23, 2012 Page 3 Improvement Objectives A. VTE Prophylaxis 1. By January 2013, VTE protocols will be developed for each surgical subspecialty. 2. By September 2013, VTE prophylaxis will be implemented at all sites. B. Antibiotic Prophylaxis 1. By September 2013, all sites of Eastern Health will be providing all appropriate surgical patients with the right antibiotic prophylaxis, at the right time, and for the right duration. Improvement Measures: How will we know the change is an improvement? C. Safe Surgery Checklist 1. The team will develop a standardized surgery checklist and adapt for all sites within Eastern Health by April 2012. 2. By September 2013, Regional Surgical Services will be consistently using surgical safety checklists throughout all sites of Eastern Health. Outcome Measure: A. VTE Prophylaxis 1. Number of surgical patients who develop PE/DVT/VTE. B. Antibiotic Prophylaxis 1. Percentage of surgical patients who develop surgical site infections in targeted populations. C. Safe Surgery Checklist 1. Percentage of surgical patients who experience a preventable operative complication. 2. Percentage of near misses identified. Process Measures: A. 1. 2. 3. VTE Prophylaxis Percentage of protocols developed. Percentage of appropriate patients who received appropriate VTE prophylaxis. Percentage of patients who were not appropriate for VTE B. 1. 2. Antibiotic Prophylaxis Percentage of antibiotics given within 0 – 60 minutes of incision. Percentage of antibiotics stopped as per protocol. C. 1. 2. Safe Surgery Checklist Percentage of adapted checklists approved and implemented. Percentage of compliance with three components of the checklist. Balancing Measure: A. VTE Prophylaxis Spread and Sustainability Guide for Charter Draft 3, January 23, 2012 Page 4 B. Antibiotic Prophylaxis 1. Percentage of surgical patients who receive appropriate antibiotic prophylaxis who develop antibiotic related occurrences (e.g. c. difficile). C. Safe Surgery Checklist Change Ideas: What Changes can we try/test to see if they will lead to an improvement? Manage Variation Resources: People Executive Sponsor: Ms. Pat Coish Snow, Vice President, Adult Acute Care Project Team Leads: Ms. Elaine Warren, Regional Director, Surgical Services (Surgery) Ms. Maria Tracey, Regional Director, Surgical Services (Perioperative) Project Steering Committee Team: Ms. Elaine Warren, Regional Director, Surgical Services (Surgery) Ms. Maria Tracey, Regional Director, Surgical Services (Perioperative) Dr. Rod Martin, Chief of Surgery Dr. Jim Flynn, Chief of Anaesthesia Dr. Darryl Boone, Dr. Jeremy Pridham, Ms. Dale Nixon, Quality and Safety Leader Ms. Donna Ronayne, Regional Manager, Infection Prevention and Control Project Team Names Roles and Responsibilities Elaine Warren and Maria Tracey Process Owner (Manager) Dale Nixon and Lynnette Woodrow Quality Improvement Support Glenda Tapp and Joanne Peddle Clinical Champion TBD Physician Champion Michelle Cantu and Gail Wells Clarenville Members Linda Drover/ Leslie Ann Rowsell Burin Members Spread and Sustainability Guide for Charter Draft 3, January 23, 2012 Page 5 Tonya Somerton/ Karen Hanley Carbonear Members Diane Parsons Women’s Health Michelle Cooper and Darlene Osmond Children’s Health Members Infection Prevention and Control Members Aims must be fully implemented across the Regional Surgical Services Program by September 2014. Existing Financial Resources: In-kind resources (e.g. personnel, library services, conference calling capabilities). Roles and Responsibilities: Sharing context knowledge, skill and experience. Communicating and developing a shared understanding within the team of the processes to be improved or changed. Testing change ideas within the team and in the real work context. Leading and supporting coworkers to adapt the new process. Completing tasks or assignments within and between meetings. Establishing two-way communication with their colleagues and the team. Facilitating the use of improvement tools and techniques. Monitoring and facilitating healthy team behaviours. Providing technical expertise and guidance focusing on team process. Supporting the team leader to plan effective team meetings. Assisting with measurement for improvement, e.g. data collection, analyzers and display. Learning and sharing new skills from and with each other. Donna Ronayne/ Lorilee Kelly Resources: Time Resources: Financial Team Commitments and Principles for working together Constraints Executive Sponsor (ES) Commitments Principles for working together Consult with Atlantic Node proactively and as needed (before team gets overwhelmed). Demonstrate mutual respect, seek out and listen to other team member’s perspectives. Hold regular meetings with minutes prepared. Have a communication plan to reflect issues, discussion points, action steps and responsibilities. Share the workload. Include other interested partners that we identify. Share successes with each other, the site, and the organization. Start small with our PDSA cycles and bite off manageable pieces, unit by unit if necessary. Connect and consult with FFLS Faculty through scheduled team calls. Identification of resources for collection and analyzing data is an immense challenge. Roles and Responsibilities: Clarifying the improvement mandate and aligning it within the organization’s strategic and operational objectives. Connecting and communicating with appropriate stakeholders. Spread and Sustainability Guide for Charter Draft 3, January 23, 2012 Page 6 Role of ES is to remove barriers and free up resources for team to succeed. Team Lead (Process Owner) Measurement Lead Team Members Commitments Allowing time and other resources. Establishing an accountability mechanism. Facilitating the work of the team within the larger organization. Engaging a team leader and a coach. Roles and Responsibilities: Completing and clarifying the team charter in a manner that ensures the support of team members and team sponsor. Organizing and running effective meetings and maintaining team records, i.e. minutes, correspondence, improvement data. Facilitating work within the team and ensuring participation at and between meetings. Communicate about the improvement work with the sponsor, team members, stakeholders, and the larger organization. Roles and Responsibilities: Ensure that data is collected and submitted consistently to Safer Healthcare Now! Team meetings will be held using teleconferencing or webinar technology. Team meetings will be scheduled monthly and decisions will be made by consensus. A communication plan will be developed to facilitate communication within the team and to stakeholders. Draft Terms of Reference Purpose The project team will develop, implement, and evaluate this project. Functions of the Committee Identify existing resources Complete environmental scans as needed Identify best practice Plan, develop, implement, and evaluate the project Act as champions during project Meetings The team will meet monthly. The team will participate in the collaborative learning series every 2 months. Special meetings, if required, will be called by the co-leads. Agenda The agenda will be prepared and distributed to all members prior to the meeting. Records Minutes will be taken and circulated to the group within 1 week of meeting. Spread and Sustainability Guide for Charter Draft 3, January 23, 2012 Page 7 Deliverables and Key Milestones A. VTE Prophylaxis Deliverables/Key Milestones Date Start Date End Date Start Date End Date Start Date End Implementation plan (including communication and evaluation plans) developed and approved Establishment of regional working group Development of surgical subspecialty specific VTE prophylaxis protocols and order sets Approval from appropriate committee structures, including Regional Surgical Services Committees Implementation Evaluation B. Antibiotic Prophylaxis Deliverables/Key Milestones Implementation plan (including communication and evaluation plans) developed and approved Development and approval of pediatric antibiotic prophylaxis guidelines Development and approval of regional policy Implementation Evaluation C. Safe Surgery Checklist Deliverables/Key Milestones Implementation plan (including communication and evaluation plans) developed and approved Establishment of regional working group Development of standardized, adapted SSCL for all sites Approval from appropriate committee structures, including Regional Surgical Services Committees Spread and Sustainability Guide for Charter Draft 3, January 23, 2012 Page 8 Implementation Evaluation Communication Plan Communication Strategy Stakeholders Internal Stakeholders VP of Acute Care Program Leadership Division Managers Employees: Clinical, Support Physicians Professional Networks External Stakeholders Patients/Families Public/Community-at-large Key Community Groups (e.g. family physicians) Department of Health and Community Services Tactics Target Audience Vice President of Acute Care Program Leadership Division Managers Topic Communication Tool / Tactic Employees Spread and Sustainability Guide for Charter Draft 3, January 23, 2012 Timeline Department Reports Email Leadership Meetings Department Reports Email Leadership Meetings Department Reports Meetings Email Departmental Newsletters (Loop) Intranet / Internet Shared Quarterly Reports Cognos Letter Flyer/Brochure Question and Answer Forum Poster Intranet Email Paystub Inserts Page 9 Meeting Schedule: Departmental Newsletters (Loop) Bulletin Boards Orientations Meetings Break Rooms Education Days Physicians Letter Flyer/Brochure FAQs Physician Lounges Departmental Newsletters (Loop) Tabletops Media Email Internet/Intranet EH Physician Listserv EH Physician Portal Patients Flyer/Brochure Tent Cards Posters Connect issues they have access to Bulletin Boards Display Kiosks Patient Rooms Media Gift Shop Public/Community PSA at-large Media Emails Internet Key Community Letters Groups Email Media Internet Department of Letters Health and Email Community Services Media Internet Collaborative Learning Series Meetings have been scheduled for every 2 months. Learning Series 2: January 18, 2012 Learning Series 3: March 06, 2011 Learning Series 4: May 16, 2012 Learning Series 5: July 11, 2012 Learning Series 6: September 12, 2012 Spread and Sustainability Guide for Charter Draft 3, January 23, 2012 Page 10 Team Meetings will be scheduled monthly. Spread and Sustainability Guide for Charter Draft 3, January 23, 2012 Page 11