Treatment Centre TYA referral procedure SOP
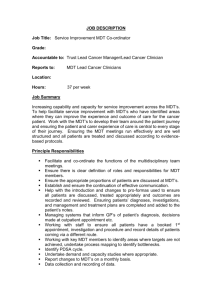
advertisement

Children and Young People’s Cancer Service (CYPCS) UCLH Primary Treatment Centre (PTC) Teenage and Young Adult (TYA) Multidisciplinary Team Meeting (MDT) Document Type Procedure(SOP) √ Policy Guideline Document Control Summary TYA Cancer Measures: 11-7D-203 Version No: 2 Author(s) (name, job title, department ) Rachael Hough, Clinical Lead CYPCS CYPCS Senior Staff Meeting Approved at: Date: 19.9.12 Director or Designee Signature: Review interval: 2 years UCL Hospitals is an NHS Foundation Trust incorporating the Eastman Dental Hospital, Elizabeth Garrett Anderson & Obstetric Hospital, The Heart Hospital, Hospital for Tropical Diseases, National Hospital for Neurology & Neurosurgery, The Royal London Homoeopathic Hospital and University CollegePage: 1 of 10 Document Title/Identifier: 106746028 Approval Date: Populated by QM Hospital. Approved By: Populated by QM Children and Young People’s Cancer Service (CYPCS) Version Change Control Log Please note that this document is subject to the document control of the UCLH CYPCS Service The following is strictly prohibited: Modifying or photocopying this controlled document Storing a local electronic or hardcopy without appropriate approval Removing this copy from its location without prior permission If you feel that this document is no longer fit for purpose please make management aware and the document will be reviewed. Version No: 1 Approval Date Populated by QM Comments/Changes Populated by Author, QMG, QM Table of Contents 1.0 Introduction ……….. .................................................................................................... 3 2.0 Abbreviations & Definitions .. ..................................................................................... 3 3.0 Scope ............................................................................................................................ 3 4.0 Stakeholders/Responsibilities .................................................................................... 4 5.0 Related Documents...................................................................................................... 4 6.0 Procedure ..................................................................................................................... 5 7.0 Limitations/ Planned Deviations ................................................................................. 8 Document Title/Identifier: 106746028 Approval Date: Populated by QM Page 2 of 10 Approved By: Populated by QM Children and Young People’s Cancer Service (CYPCS) 1.0 Introduction The UCLH TYA MDT has been established in accordance with the Improving Outcomes for Children and Young People with Cancer Guidance, NICE 2005. The purpose of the MDT is to ensure that teenage and young adult patients with cancer; 1.1. 1.2 1.3 1.4 1.5 Receive expert medical treatment for their cancer, which is appropriate for age. Have access to appropriate clinical trials where available. Have an allocated key worker. Are assured of consistency of therapeutic approach between adult and paediatric physicians. Have consideration of their individualised psychosocial needs, based on their social and emotional maturity. 1.6 1.7 1.8 1.9 The MDT also provides a forum for Discussion of those cancers in TYA patients for which there is no site specific MDT. Facilitation of transition from paediatric, through teenage to adult cancer services. Registration on the national TYA cancer database. Co-ordination between site specific and TYA MDTs. 2.0 Abbreviations & Definitions MDT TYA IOG PTC 3.0 Multidisciplinary Team Teenage and young adult Implementing Outcomes Guidance Primary Treatment Centre Scope This policy applies to all UCLH TYA MDT members. Document Title/Identifier: 106746028 Approval Date: Populated by QM Page 3 of 10 Approved By: Populated by QM Children and Young People’s Cancer Service (CYPCS) 4.0 Stakeholders/Responsibilities 4.1 The MDT Coordinator will be responsible for Receiving MDT referrals Sending acknowledgment of receipt of referral within 1 working day Sending invitation to referring clinician to attend or videoconference on date and time their patient will be reviewed Arranging for histopathologist/radiologists etc to be present if necessary Preparing MDT lists for both TYA and TYA psychosocial meetings Keeping a record of core and extended members present at each meeting Sending written record of outcome to referring clinician and GP Ensuring written record uploaded into UCLH CDR files Send UCLH TYA information pack to patient Maintaining patient list for each meeting and specific patient forms, which will be stored in the TYA MDT folder on the shared server (Cancer_services on ‘sharefs5’ drive). 4.2 Core members or their nominated deputy (defined in the terms of reference) Core members must be present at 2/3 of meetings 4.3 CYPCS Data Manager Will send the TYA registration forms to the national registry after each MDT 4.4 Referring Clinicians or Keyworkers Must send referral form to MDT coordinator at least 24 hours prior to the meeting (2pm Tuesdays). May attend the MDT in person or via videoconferencing 5.0 Related Documents Improving Outcomes for Children and Young People with Cancer Guidance, NICE 2005 Document Title/Identifier: 106746028 Approval Date: Populated by QM Page 4 of 10 Approved By: Populated by QM Children and Young People’s Cancer Service (CYPCS) 6.0 Procedure (Flow Diagram in Appendix 1) 6.1 Venue MDT Conference Room, 4th Floor Macmillan Cancer Centre, Huntley Street, London WC1E 6AG 6.2 Time Wednesday 3.00-5.00pm 6.3 TYA Pathways Any patient aged 13-18 years with a confirmed or strongly suspected cancer, must be referred to the CYPCS at UCLH. Any patient aged 19-24 with a confirmed or strongly suspected cancer, should be referred to the TYA MDT, but may be investigated and treated either at the referring centre or at the PTC, according to patient choice and if the referring centre is designated to deliver network care. Irrespective of treating centre, all patients should be re-referred to the TYA MDT in the event of disease progression or relapse or when transition is indicated. 6.4 MDT Referral The MDT coordinator will send an invitation to submit TYA MDT referral forms by email to all cancer clinicians and keyworkers on Fridays and Mondays each week (a blank referral form will be attached to the e-mail). The TYA MDT referral should be made in parallel with referral to the relevant site specific MDT. A TYA MDT Referral Form should be completed by the referring team and faxed or emailed to the TYA MDT Coordinator (E-mail address: ucl-tr.TYAMDT@nhs.net; Fax no. 020 3447 1841; Mobile number: 078 9214 7785) by 2pm on the Tuesday preceding the next MDT. The MDT coordinator will send acknowledgment of receiving the referral within 1 working day. Document Title/Identifier: 106746028 Approval Date: Populated by QM Page 5 of 10 Approved By: Populated by QM Children and Young People’s Cancer Service (CYPCS) 6.5 Preparation for the TYA MDT The MDT Coordinator saves the referral forms into appropriately initialled folders on the UCLH cancer services shared server (:\\Shared\MDT\TYA MDT\PTC TYA MDT) The MDT coordinator will prepare an electronic list of patients to be discussed at each meeting and hyperlink patient names to the forms saved to the shared server. The MDT coordinator will circulate the list for discussion to all MDT members via e-mail by 5pm on the day before the meeting. Each patient will be allocated a time slot to enable video-conferencing if required. 6.6 Process of the MDT Each attendee will sign a register which will be stored by the MDT coordinator. The meeting will be chaired by the PTC TYA MDT Lead Clinician or nominated deputy, according to the meeting’s terms of reference. Each patient will be reviewed with specific focus on; Diagnosis and which site specific MDT has reviewed it Whether further investigations or diagnostic review are necessary Treatment plan and place of delivery of each treatment modality Named consultant in charge of each treatment modality Availability of clinical trials Identification of the patient’s keyworker (either at PTC or referring centre) Psychosocial needs and how these are to be met Results of fertility discussion Registration details The outcome of the discussion will be typed into the allocated space on the referral form, during the meeting. This will be projected for MDT members to review. Document Title/Identifier: 106746028 Approval Date: Populated by QM Page 6 of 10 Approved By: Populated by QM Children and Young People’s Cancer Service (CYPCS) 6.7 Communication of Outcome of the MDT For UCLH patients, the MDT coordinator will upload the form for each patient, stored on the shared server, into the patients CDR file. For patients choosing treatment at external designated hospitals, the MDT coordinator will e-mail the referral form including outcome to the referring clinician (if an NHS.net account is available). Otherwise the MDT coordinator will send the completed form via conventional mail or fax. Irrespective of treating centre, a copy of the completed form will be sent to the patient’s GP. The MDT coordinator will send out a UCLH TYA cancer care information pack to the patient. The patient will be informed of the outcome of the MDT by their keyworker or physician who are primarily responsible for their care (either at their local hospital or the PTC). The CYPCS Data Manager will send the TYA Patient Notification document to the national registry, unless this has already been undertaken by the primary physician (19-24 year olds). 6.8 Management of Differences in Clinical Opinion There may be occasions when the TYA MDT and a site-specific MDT do not agree on the optimal management plan. Different MDTs often express differing views and offer different recommendations for treatment. When such differences exist, the following step may prove useful: All views should be heard and respected Any decision, including differences of opinion, need to be recorded as part of both MDT records The treatment choice should take account of the following options if available: An open National/international study or trial open in one or other place of care for the condition that includes the TYA patient’s age range. An open national/international study or trial for the condition that has been subject to Quality Assurance review (e.g. approval by an NCRI group) Established treatment guidelines that include the whole TYA age range Established treatment guidelines that are based upon consensus between the MDT members with expertise in that condition and that include the entire TYA age range from 16-24 inclusive In the absence of the above there should be an open recorded discussion of differing views at an MDT meeting involving both cancer site and age-appropriate considerations. The management plan taking priority will be that where the patient is to receive their medical care. Document Title/Identifier: 106746028 Approval Date: Populated by QM Page 7 of 10 Approved By: Populated by QM Children and Young People’s Cancer Service (CYPCS) Then, as part of the routine work of the team, but after a 2-month interval each would summarize the current data supporting their case, and then together the team write guidelines for future cases where the disagreements are explicit to all, leading over time to constructive suggestions and research ideas. 6.9 Governance/Operational Policy Meetings In addition to the weekly meetings, the TYA MDT will meet once yearly to review, agree and record operational policies. 7.0 Limitations/ Planned Deviations On occasions the recommendation of either TYA or site specific MDT may not be followed. This may be for a range of reasons: If the patient fails to attend the clinic, the consultant will record that the patient has failed to attend in the case notes. The patient’s GP will be informed. The referring clinician and appropriate CNS should be informed of the non-attendance and will be responsible for liaising with the patient locally. A further appointment should be offered where appropriate. In some instances the MDT recommendations developed with limited information will not be appropriate due to the patient’s condition when assessed in person. A record of these occurrences will be recorded. In some instances the MDT recommendations may not be acceptable to the patient. A record will be documented. 8.0 Appendices. Document Title/Identifier: 106746028 Approval Date: Populated by QM Page 8 of 10 Approved By: Populated by QM Children and Young People’s Cancer Service (CYPCS) Appendix A: TYA Referral and Communication of Outcomes New patient aged 19-24 at hospital other than PTC New patient aged 13-24 at UCLH Complete referral form and fax/e-mail to MDT coordinator MDT list generated and circulated to members Receipt of referral and invitation to MDT sent within 1 working day TYA MDT Review Outcome phone call within 1 working day Document Title/Identifier: 106746028 Approval Date: Populated by QM Outcome letter sent to referring clinician, keyworker and GP Information pack sent to patient Page 9 of 10 Approved By: Populated by QM Children and Young People’s Cancer Service (CYPCS) Document Title/Identifier: 106746028 Approval Date: Populated by QM Page 10 of 10 Approved By: Populated by QM