Prospective multicenter evaluation of the pulmonary
advertisement
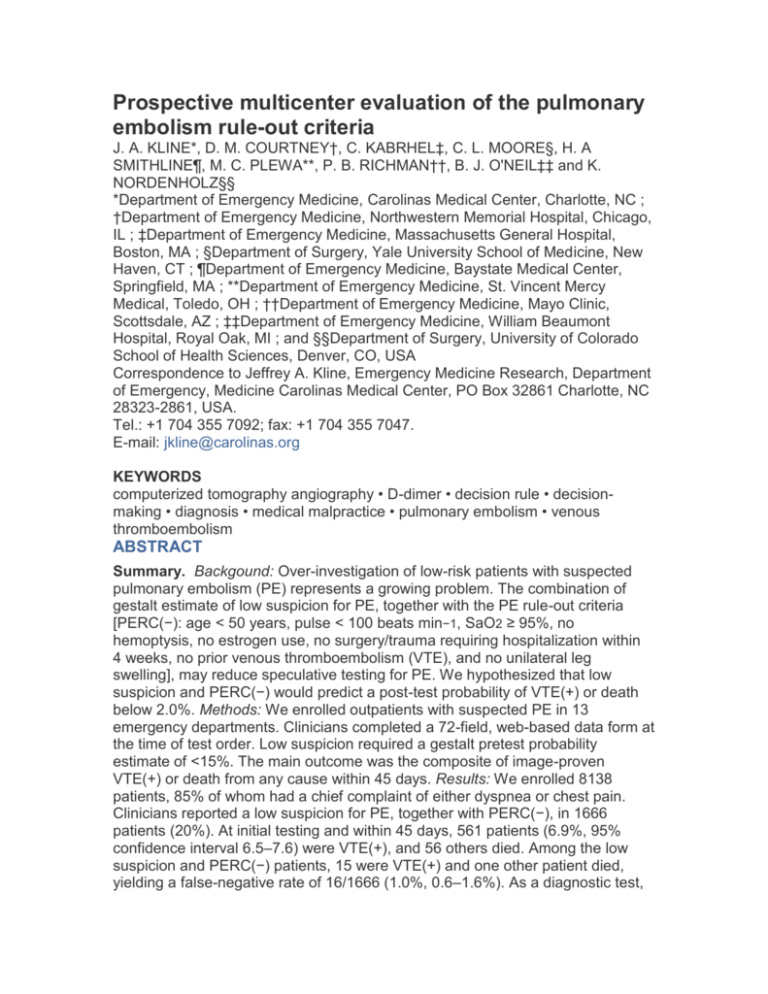
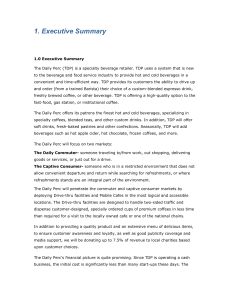
Prospective multicenter evaluation of the pulmonary embolism rule-out criteria J. A. KLINE*, D. M. COURTNEY†, C. KABRHEL‡, C. L. MOORE§, H. A SMITHLINE¶, M. C. PLEWA**, P. B. RICHMAN††, B. J. O'NEIL‡‡ and K. NORDENHOLZ§§ *Department of Emergency Medicine, Carolinas Medical Center, Charlotte, NC ; †Department of Emergency Medicine, Northwestern Memorial Hospital, Chicago, IL ; ‡Department of Emergency Medicine, Massachusetts General Hospital, Boston, MA ; §Department of Surgery, Yale University School of Medicine, New Haven, CT ; ¶Department of Emergency Medicine, Baystate Medical Center, Springfield, MA ; **Department of Emergency Medicine, St. Vincent Mercy Medical, Toledo, OH ; ††Department of Emergency Medicine, Mayo Clinic, Scottsdale, AZ ; ‡‡Department of Emergency Medicine, William Beaumont Hospital, Royal Oak, MI ; and §§Department of Surgery, University of Colorado School of Health Sciences, Denver, CO, USA Correspondence to Jeffrey A. Kline, Emergency Medicine Research, Department of Emergency, Medicine Carolinas Medical Center, PO Box 32861 Charlotte, NC 28323-2861, USA. Tel.: +1 704 355 7092; fax: +1 704 355 7047. E-mail: jkline@carolinas.org KEYWORDS computerized tomography angiography • D-dimer • decision rule • decisionmaking • diagnosis • medical malpractice • pulmonary embolism • venous thromboembolism ABSTRACT Summary. Backgound: Over-investigation of low-risk patients with suspected pulmonary embolism (PE) represents a growing problem. The combination of gestalt estimate of low suspicion for PE, together with the PE rule-out criteria [PERC(−): age < 50 years, pulse < 100 beats min−1, SaO2 ≥ 95%, no hemoptysis, no estrogen use, no surgery/trauma requiring hospitalization within 4 weeks, no prior venous thromboembolism (VTE), and no unilateral leg swelling], may reduce speculative testing for PE. We hypothesized that low suspicion and PERC(−) would predict a post-test probability of VTE(+) or death below 2.0%. Methods: We enrolled outpatients with suspected PE in 13 emergency departments. Clinicians completed a 72-field, web-based data form at the time of test order. Low suspicion required a gestalt pretest probability estimate of <15%. The main outcome was the composite of image-proven VTE(+) or death from any cause within 45 days. Results: We enrolled 8138 patients, 85% of whom had a chief complaint of either dyspnea or chest pain. Clinicians reported a low suspicion for PE, together with PERC(−), in 1666 patients (20%). At initial testing and within 45 days, 561 patients (6.9%, 95% confidence interval 6.5–7.6) were VTE(+), and 56 others died. Among the low suspicion and PERC(−) patients, 15 were VTE(+) and one other patient died, yielding a false-negative rate of 16/1666 (1.0%, 0.6–1.6%). As a diagnostic test, low suspicion and PERC(−) had a sensitivity of 97.4% (95.8–98.5%) and a specificity of 21.9% (21.0–22.9%). Conclusions: The combination of gestalt estimate of low suspicion for PE and PERC(−) reduces the probability of VTE to below 2% in about 20% of outpatients with suspected PE.