Objectives 35 - U

Pathology
Lecture 35 Diffuse Interstitial (Infiltrative, Restrictive) Diseases
1) Contrast idiopathic pulmonary fibrosis (IPF) with emphysema in terms of clinical presentation, gross and microscopic morphology, etiology, and prognosis.
Clinical
Presentation
Idiopathic Pulmonary Fibrosis (IPF)
Insidious onset with increasing dyspnea on exertion and dry cough. Most patients are 40-70 years old. Hypoxemia, cyanosis, and clubbing occur later in the course.
Emphysema
Sometimes cough or wheezing is chief complaint, weight loss and common.
Classically, patient is barrel chested and dyspneic with prolonged expiration, sits foreword breathing through pursed lips.
Voluminous, pale lungs that overlap the heart.
Large alveoli can be seen on the cut surface.
Gross
Microscopic Patchy interstitial fibrosis with fibroblastic foci that become more collagenous and less cellular overtime causing collapse of alveolar walls and formation of cystic spaces (honeycomb fibrosis)
Etiology
Smaller lung, cobblestoned pleura, fibrosis of the parenchyma mostly in the lower lobe subpleural regions and along interlobular septa
Prognosis
Unknown cause, immune mechanisms suspected.
Starts out as an alveolitis (accumulation of inflammatory cells), mediators are released the cause fibroblasts multiply and lay down collagen.
Mean survival is 3 years or less. Lung transplantation is the only cure.
Abnormally large alveoli separated by thin septa was only focal centriacinar fibrosis.
Blebs or bullae appear with advanced disease.
Bronchioles and vasculature are deformed.
Smoking produces reactive oxygen species causing tissue damage and resulting in inactivation of anti-proteases with an increase in neutrophil elastase (more tissue damage)
Development of cor pulmonale and CHF is associated with poor prognosis.
2) Define desquamative interstitial pneumonitis.
Desquamative Interstitial Pneumonitis - a smoking-related interstitial disease characterized by the accumulation of large number of macrophages with abundant cytoplasm containing dusty brown pigment (smokers’ macrophages) in the airspaces.
3) Define hypersensitivity pneumonitis; give some examples.
Hypersensitivity Pneumonitis - an acute to chronic interstitial lung disease caused by inhalation organic dust (protein antigens). Examples include: 1) spores of thermophilic bacteria ( Farmer's lung ), 2) proteins from serum, droppings, or bird feathers ( pigeon breeders lung ), and 3) thermophilic bacteria in heated water reservoirs ( humidifier lung ).
4) Describe the microscopic histology of hypersensitivity pneumonitis.
Histologic changes in subacute and chronic forms are characteristically centered on bronchioles.
They include 1) interstitial pneumonitis consisting primarily of lymphocytes, plasma cells, and macrophages, 2) noncaseating granulomas in 2/3 of patients, and 3) interstitial fibrosis and obliterative bronchiolitis (late stages). >50% of patients have intra-alveolar infiltrate.
5) Define pulmonary infiltration with eosinophilia; list some common causes.
Pulmonary infiltration with eosinophilia - a collection of entities characterized by eosinophilic infiltrates in blood, lung, or both.
There are many causes, including idiopathic but including microfilaria, drugs, association with asthma, and other infectious agents.
6) Explain the immunologic mechanism at work in Goodpasture’s syndrome.
Goodpasture’s syndrome is an autoimmune disease were antibodies attack the glomerular and pulmonary basement membranes giving rise to proliferative, rapidly progressive glomerulonephritis and a necrotizing hemorrhagic interstitial pneumonitis
7) List some types of pulmonary hemorrhage syndromes.
Pulmonary hemorrhage syndromes include: 1) Goodpasture 's syndrome, 2) idiopathic pulmonary hemosiderosis, and 3) vasculitis-associated hemorrhage, which is found in conditions such as hypersensitivity angiitis, Wegener granulomatosis, and lupus erythematosus.
8)
Contrast Goodpasture’s syndrome with idiopathic pulmonary hemosiderosis.
Goodpasture 's Syndrome
Clinical Presentation Respiratory symptoms, principally hemoptysis and radiographic evidence of focal pulmonary consolidations.
Next glomerulonephritis, renal failure, common cause of death is uremia.
Etiology Autoimmune disease were antibodies attack basement membrane in kidney glomeruli and lung alveoli.
Idiopathic Pulmonary Hemosiderosis
Intermittent, diffuse alveolar hemorrhage presenting with the insidious onset of productive cough, hemoptysis, anemia, and weight loss.
Unknown, no detectable antibodies to basement membranes however, response to immunosuppression is good.
9) Recall the characteristic histologic feature of pulmonary alveolar proteinosis.
The characteristic histologic feature is accumulation of acellular surfactant in intraalveolar and bronchiolar spaces.
10) List some collagen vascular diseases that may be associated with IPF/VIP.
Systemic lupus erythematosus, rheumatoid arthritis, progressive systemic sclerosis
(scleroderma), dermatomyositis-polymyositis, and makes connective tissue disease, can involve long to a lesser or greater degree at some time in their course.
11) List some other pulmonary conditions that are associated with rheumatoid arthritis.
In rheumatoid arthritis, pulmonary involvement is common and may occur in one of four forms: 1) chronic pleuritis, with or without fusion; 2) diffuse interstitial pneumonitis and fibrosis; 3) intrapulmonary rheumatoid nodules; and 4) pulmonary hypertension.
12) Explain why it is important to recognize that a patient has developed druginduced lung disease.
Drugs can cause a variety of both acute and chronic alterations in respiratory structure and function, including bronchospasm, pulmonary edema, diffuse alveolar damage, organizing pneumonia, interstitial fibrosis, bronchiolitis obliterans, and eosinophilic pneumonia.
Bleomycin (cytotoxic drug) amiodarone (antiarrhythmic) = pneumonitis and fibrosis
13) Define ARDS and DAD and explain the difference in the two terms.
Acute Respiratory Distress Syndrome (ARDS) – a clinical syndrome characterized by the rapid onset of severe life-threatening respiratory insufficiency, cyanosis, severe arterial hypoxemia, decreased lung compliance, and diffuse pulmonary infiltrates on radiographs.
Diffuse Alveolar Damage (DAD) - the histologic manifestation of ARDS is a morphologic (pathologic) diagnosis.
14) Summarize the pathogenesis of ARDS.
ARDS can result from either epithelial or endothelial cell injury, or both. Most common causes are: 1) sepsis; 2) diffuse pulmonary infections; 3) aspiration; and 4) trauma. Important features in pathogenesis include release of endotoxin in sepsis, release of TNF-α, and injury from microthrombi.
15) List the characteristic gross and microscopic findings of DAD.
Gross: very heavy, diffusely firm, red-tan to tan lung.
Microscopic: alveolar, endothelial, and epithelial injury. Alveolar walls become lined with waxy hyaline membranes, type II epithelial cells undergo proliferation in an attempt to regenerate the alveolar lining, and host responds with lymphocytes, macrophages, and sometimes fibrosis (organization).
16) Characterize the prognosis of ARDS.
40% of patients recover, with normal lung function. Mortality is about 60%. A few patients develop diffuse fibrosis and die in weeks to months.
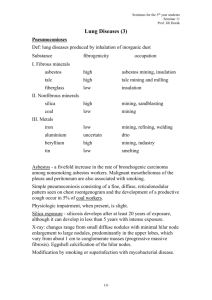
17) List the four common pneumoconiosis, their clinical presentation, histology and associated diseases.
Disease
Coal Workers
Pneumoconiosis
(CWP)
Silicosis
Clinical Associations
Little or no functional impairment
Microscopic
Dense collagen and pigment with necrotic center
Disease Associations
Anthracosis (any black dust accumulation) Tuberculosis
Berylliosis
Asbestos
Exposure –
Two forms serpentine and
Most prevalent chronic occupational disease. Silica produces free radicals, damaging macrophages to release cytokines
(inflammation)
Type IV cellular immune response (hypersensitivity) forms granulomas
Dyspnea and cough.
Fibrogenic, asbestos fibers are phagocytized causing the release of chemical
Nodular lesions of concentric layers of hyalinized collagen with a dense capsule
Granulomatous disease virtually identical to sarcoidosis
Asbestos bodies, golden brown, fusiform or beaded rods consisting of asbestos fibers coated with iron and proteins
PMF - right heart failure, tuberculosis, Caplan's
Increased risk of lung cancer,
HLA-DPβ-Glu 69 allele confers greater risk to those exposed.
Lung cancers, potentiates the effects of smoking, 50-80% of all diffuse mesotheliomas. amphibole
(↑pathogenic) mediators resulting in fibrosis.
18) List and define the various diseases caused by asbestos.
Localized fibrous plaques or, rarely, diffuse pleural fibrosis - macrophages attempt to phagocytize asbestos fibers resulting in asbestos bodies, indistinguishable from DIF.
Pleural effusions - fluid collections in the space surrounding the lungs.
Parenchymal interstitial fibrosis (asbestosis) - the fibrous scarring of the lungs from inhalation of asbestos fibers.
Lung carcinoma - malignant tumor of the lung.
Mesotheliomas - a benign or malignant tumor affecting the lining of the chest or abdomen.
Laryngeal and perhaps other extrapulmonary neoplasms, including colon carcinomas
- tumors of the larynx and other areas outside the lung.