Treprostinil use in the treatment of pulmonary arterial hypertension
advertisement
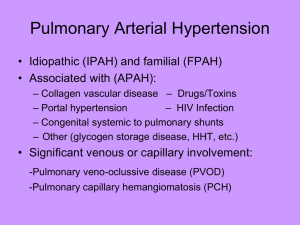
Article "Development of the European Network in Orphan Cardiovascular Diseases" „Rozszerzenie Europejskiej Sieci Współpracy ds Sierocych Chorób Kardiologicznych” Title: Treprostinil use in the treatment of pulmonary arterial hypertension. Author: Jakub Stępniewski Affiliation: Department of Cardiac and Vascular Diseases, John Paul II Hospital, Krakow, Poland Background Pulmonary arterial hypertension (PAH), defined as an elevation of mean pulmonary arterial pressure ≥ 25mmHg is a chronic diseases impeding every-day activity of affected people and inevitably leads to premature death. Therefore, management of PAH remains a great challenge for many caregivers. Discussion As a synthetic PGI2 derivative, treprostinil shows biological effects similar to epoprostenol. [1,2] However, in contrast to epoprostenol, treprostinil sodium is chemically and metabolically more stable in ambient temperature and neutral pH presenting longer duration of action with elimination half-life time of approximately 4 hours. [3] These features made treprostinil suitable for subcutaneous (s.c.) as well as i.v. use. Studies on pharmacokinetics of s.c. treprostinil confirmed its bioavailability after s.c. infusion, additionally showing that treprostinil plasma concentration linearly corresponds with dosing rates and reaches its steady state after about 10 hours. [4] Before FDA first approved treprostinil for the s.c. treatment of PAH in 2002, the efficacy of treprostinil s.c. was evaluated in a large randomized, multicenter clinical trial performed on a group of 470 patients with PAH of different etiologies. [5] 12- week double- blind, placebocontrolled study reported that s.c. treprostinil improves clinical state, exercise capacity and John Paul II Hospital in Kraków Jagiellonian University, Institute of Cardiology 80 Prądnicka Str., 31-202 Kraków; tel. +48 (12) 614 33 99; 614 34 88; fax. +48 (12) 614 34 88 e-mail: rarediseases@szpitaljp2.krakow.pl www.crcd.eu the quality of life of treated patients as well as hemodynamic parameters assessed by RHC. 6minute walk distance (6MWD) increased importantly comparing to placebo group where it remained unchanged. The extent of improvement was greater in patients in more advanced stages of PAH (higher WHO FC) at baseline and was dependent on applied dose. Patients who achieved treprostinil dosing of more than 13.8 ng/kg/min had significantly greater change in 6MWD in comparison to those receiving smaller doses. Persistence of aforementioned improvements was observed in several subsequent long-term trials. In one study 860 PAH patients were followed for up to 4 years in order to state that s.c. treprostinil therapy was related with a survival rate of 88% at 1 year and 70% at 4 years in comparison to predicted survival of 69% and 38% respectively. [6] Adverse events were the reason for interruption of the study for 23% of patients and additional 11% of them were converted for alternative treatment. Another retrosepctive study, conducted in three European university hospitals indicated efficacy of s.c. treprostinil in terms of improvement in 6MWD and clinical state in 99 PAH and 23 inoperable CTEPH patients. [7] The assessed event- free survival rates at 1 and 3 years were 83,2% and 69%, respectively, with corresponding overall survival of 88,6% and 70,6%, respectively. Recently published data from a prospective registry of 111 PAH patients treated with s.c. treprostinil confirmed the previously produced reports. [8] 1 year overall survival rate was 84%. After 5 and 9 years the survival was 53% and 33%, respectively. Discontinuation was observed in 12% of patients due to occurrence side effects mainly drug infusion site reaction or pain. Results provided by these studies suggest that the use of continuous s.c. treprostinil in treatment of PAH is a genuine alternative for i.v. epoprostenol. In order to verify the feasibility of treprostinil i.v. mode of delivery a randomized clinical trial with healthy volunteers was designed. [9] Pharmacokinetic assessment of continuous i.v. infusion was performed and compared with s.c. infusion showing that both routs are bioequivalent. Additionally, it has been shown, that transitioning from i.v. epoprostenol to i.v. treprostinil is safe and efficacious in adults and children. [10,11,12] The switching can be performed either on a rapid (24-48hours) or slow (up to 14 days) fashion. [13] Interestingly, John Paul II Hospital in Kraków Jagiellonian University, Institute of Cardiology 80 Prądnicka Str., 31-202 Kraków; tel. +48 (12) 614 33 99; 614 34 88; fax. +48 (12) 614 34 88 e-mail: rarediseases@szpitaljp2.krakow.pl www.crcd.eu while the dosing of treprostinil in s.c. infusion is about the same as in i.v. , it has to be at least two times higher than i.v epoprostenol dose, in order to maintain the clinical benefit. [10,13, 14] Following this and several consecutive studies on efficacy of i.v. treprostinil the FDA approved treprostinil to intravenous application as a therapy for PAH in 2004. One of these trials, an open-label, uncontrolled study demonstrated the positive role of i.v. treprostinil in amelioration of 6MWD, hemodynamics and dyspnea indices in 16 patients followed for 12 weeks. [15] These observations were confirmed in a randomized, placebo-controlled trial performed on a group of 44 PAH patients residing the Indian subcontinent. [16] Correspondingly, an improvement of exercise capacity and clinical status, as well as a positive trend in improvement of survival in treprostinil group was noted. However, data on long-term survival analysis of i.v. treprostinil are limited to date. Conclusion Treprostinil remain an optional therapy for PAH patients. Their efficacy have been proven in numerous clinical trials and meta-analyses and as a consequence prostacyclines are recommended by ESC and ACCF/AHA authorities for the treatment of PAH. References 1. Steffen RP, de la Meta M. The effects of 15AU81, a chemically stable prostacyclin analog, on the cardiovascular and renin–angiotensin systems of anesthetized dogs. Prostaglandins Leukot. Essent. Fatty Acids 43, 277–286 (1991). 2. McNulty MJ, Sailstad JM, Steffen RP. The pharmacokinetics and pharmacodynamics of prostacyclin analog 15AU81 in anesthetized beagle dog. Prostaglandins Leukot. Essent. Fatty Acids 48, 159–166 (1993). 3. Vachiery JL, Naeije R. Treprostinil for pulmonary hypertension. Expert Rev Cardiovasc Ther. 2004;2:183– 191. 4. Wade M, Baker FJ, Roscigno R, et al. Absolute bioavailability and pharmacokinetics of treprostinil sodium administered by acute subcutaneous infusion J. Clin. Pharmacol. 44, 83 88 (2004). 5. Simonneau G, Barst RJ, Galie N, et al. Continuous subcutaneous infusion of treprostinil, a prostacyclin analogue, in patients with pulmonary arterial hypertension. A double‑blind, randomized, placebo‑controlled trial. Am J Respir Crit Care Med 2002;165:800 –804. 6. Barst RJ, Galie N, Naeije R, et al. Long‑term outcome in pulmonary arterial hypertension patients treated with subcutaneous treprostinil. Eur Respir J. 2006;28:1195–1203. 7. Lang I, Gomez‑Sanchez M, Kneussl M, et al. Efficacy of long‑term subcutaneous treprostinil sodium therapy John Paul II Hospital in Kraków Jagiellonian University, Institute of Cardiology 80 Prądnicka Str., 31-202 Kraków; tel. +48 (12) 614 33 99; 614 34 88; fax. +48 (12) 614 34 88 e-mail: rarediseases@szpitaljp2.krakow.pl www.crcd.eu in pulmonary hypertension. Chest. 2006;129:1636–1643. 8. Roela Sadushi‑Koliçi, Nika Skoro‑Sajer, Daniel Zimmer, et al. Long‑term treatment, tolerability, and survival with sub‑cutaneous treprostinil for severe pulmonary hypertension. J Heart Lung Transplant. 2012:31:735–743. 9. Laliberte K, Arneson C, Jeffs R, Hunt T, Wade M. Pharmacokinetics and steady‑state bioequivalence of treprostinil sodium (Remodulin) administered by the intravenous and subcutaneous route to normal volunteers. J Cardiovasc Pharmacol 2004;44:209e14. 10. Gomberg‑Maitland M, Tapson VF, Benza RL, et al. Transition from intravenous epoprostenol to intravenous treprostinil in pulmonary hypertension. Am J Respir Crit Care Med 2005;172:1586–9. 11. Ivy DD, Claussen L, Doran A. Transition of stable pediatric patients with pulmonary arterial hypertension from intravenous epoprostenol to intravenous treprostinil. Am J Cardiol 2007;99:696–8. 12. Rubenfire M, McLaughlin VV, Allen RP, et al. Transition from IV epoprostenol to subcutaneous treprostinil in pulmonary arterial hypertension: a controlled trial. Chest 2007;132:757–63. 13. Sitbon O, Manes A, Jais X, et al. Rapid switch from intravenous epoprostenol to intravenous treprostinil in patients with pulmonary arterial hypertension. J Cardiovasc Pharmacol 2007;49:1–5. 14. McSwain CS, Benza R, Shapiro S, et al. Dose proportionality of treprostinil sodium administered by continuous subcutaneous and intravenous infusion. J Clin Pharmacol 2008;48:19–25. 15. Tapson VF, Gomberg‑Maitland M, McLaughlin VV, et al. Safety and efficacy of IV treprostinil for pulmonary arterial hypertension: a prospective, multicenter, open‑label, 12 week trial. Chest 2006; 129:683–8. 16. Hiremath J, Thanikachalam S, Parikh K, et al. Exercise improvement and plasma biomarker changes with intravenous treprostinil therapy for pulmonary arterial hypertension: a placebo‑controlled trial. J Heart Lung Transplant. 2010;29:137–149. ……………………………………….. Author’s signature* [* Signing the article will mean an agreement for its publication] John Paul II Hospital in Kraków Jagiellonian University, Institute of Cardiology 80 Prądnicka Str., 31-202 Kraków; tel. +48 (12) 614 33 99; 614 34 88; fax. +48 (12) 614 34 88 e-mail: rarediseases@szpitaljp2.krakow.pl www.crcd.eu