usf department of cardiology
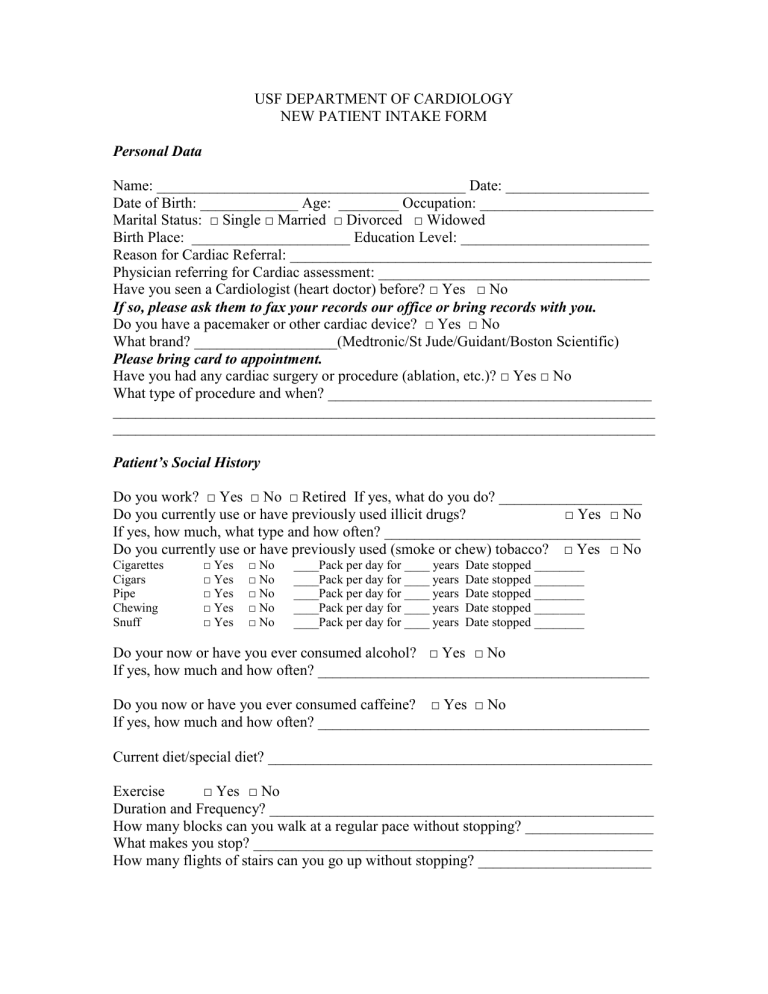
USF DEPARTMENT OF CARDIOLOGY
NEW PATIENT INTAKE FORM
Personal Data
Name: _________________________________________ Date: ___________________
Date of Birth: _____________ Age: ________ Occupation: _______________________
Marital Status: □ Single □ Married □ Divorced □ Widowed
Birth Place: _____________________ Education Level: _________________________
Reason for Cardiac Referral: ________________________________________________
Physician referring for Cardiac assessment: ____________________________________
Have you seen a Cardiologist (heart doctor) before? □ Yes □ No
If so, please ask them to fax your records our office or bring records with you.
Do you have a pacemaker or other cardiac device? □ Yes □ No
What brand? ___________________(Medtronic/St Jude/Guidant/Boston Scientific)
Please bring card to appointment.
Have you had any cardiac surgery or procedure (ablation, etc.)? □ Yes □ No
What type of procedure and when? ___________________________________________
________________________________________________________________________
________________________________________________________________________
Patient’s Social History
Do you work? □ Yes □ No □ Retired If yes, what do you do? ___________________
Do you currently use or have previously used illicit drugs?
□ Yes □ No
If yes, how much, what type and how often? __________________________________
Do you currently use or have previously used (smoke or chew) tobacco? □ Yes □ No
Cigarettes
Cigars
Pipe
Chewing
Snuff
□ Yes □ No ____Pack per day for ____ years Date stopped ________
□ Yes □ No
____Pack per day for ____ years Date stopped ________
□ Yes □ No ____Pack per day for ____ years Date stopped ________
□ Yes □ No ____Pack per day for ____ years Date stopped ________
□ Yes □ No ____Pack per day for ____ years Date stopped ________
Do your now or have you ever consumed alcohol? □ Yes □ No
If yes, how much and how often? ____________________________________________
Do you now or have you ever consumed caffeine? □ Yes □ No
If yes, how much and how often? ____________________________________________
Current diet/special diet? ___________________________________________________
Exercise
□ Yes □ No
Duration and Frequency? ___________________________________________________
How many blocks can you walk at a regular pace without stopping? _________________
What makes you stop? _____________________________________________________
How many flights of stairs can you go up without stopping? _______________________
REVIEW OF SYMPTOMS
Are you currently having or have you had the following problems?
Anemia
Anxiety
Arthritis
Attempted Suicide
Black and Tarry Stools
Blood in Stool
Blood clots in legs/lungs
Blood in Urine
Blood Transfusions
Chronic Bronchitis
Runny or Stuffed Nose
Depression
Change in Bowel Habits
Difficulty Hearing
Exposure to Asbestos
Corrective lenses?
Eye Pain, Vision Problems/Spots, Blurriness?
Esophageal Reflux
Excessive Bleeding
Gallbladder Disease
Headache
Dizziness (Syncope or fainting)
Indigestion or Heartburn
Frequent and/or productive cough
Weight change
Nervousness
Chest pain, discomfort or pressure
Back pain that radiates around to chest
Palpitations
Fatigue / Feeling tired
Difficulty in breathing/Shortness of breath
Leg pain w/excertion (leg claudication)
Awakening at night with shortness of breath
Excessive sweating
Abdominal pain
Fever(s)
Chills
Vomiting
Neck pain
Jaw pain
Excessive urination
Sleep w/ extra pillows or sleeping upright
Numbness or tingling in extremities
Fast heart rate
Slow heart rate
Irregular heart rate
Wheezing
Rapid breathing
Swelling in legs, hands and/or feet
Coldness in hands and/or feet
□ Yes □ No When? _________________
□ Yes □ No When? _________________
□ Yes □ No When? _________________
□ Yes □ No When? _________________
□ Yes □ No When? _________________
□ Yes □ No When? _________________
□ Yes □ No When? _________________
□ Yes □ No When? _________________
□ Yes □ No When? _________________
□ Yes □ No When? _________________
□ Yes □ No When? _________________
□ Yes □ No When? _________________
□ Yes □ No When? _________________
□ Yes □ No When? _________________
□ Yes □ No When? _________________
□ Yes □ No When? _________________
□ Yes □ No When? _________________
□ Yes □ No When? _________________
□ Yes □ No When? _________________
□ Yes □ No When? _________________
□ Yes □ No When? _________________
□ Yes □ No When? _________________
□ Yes □ No When? _________________
□ Yes □ No When? _________________
□ Yes □ No When? _________________
□ Yes □ No When? _________________
□ Yes □ No When? _________________
□ Yes □ No When? _________________
□ Yes □ No When? _________________
□ Yes □ No When? _________________
□ Yes □ No When? _________________
□ Yes □ No When? _________________
□ Yes □ No When? _________________
□ Yes □ No When? _________________
□ Yes □ No When? _________________
□ Yes □ No When? _________________
□ Yes □ No When? _________________
□ Yes □ No When? _________________
□ Yes □ No When? _________________
□ Yes □ No When? _________________
□ Yes □ No When? _________________
□ Yes □ No When? _________________
□ Yes □ No When? _________________
□ Yes □ No When? _________________
□ Yes □ No When? _________________
□ Yes □ No When? _________________
□ Yes □ No When? _________________
□ Yes □ No When? _________________
□ Yes □ No When? _________________
□ Yes □ No When? _________________
REVIEW OF SYMPTOMS (CONTINUED)
Hemorrhoids
High Triglycerides
HIV
Hoarseness or Voice Change
Indigestion/ Heartburn
Joint stiffness, Pain or Swelling
Kidney Stones
Loss of Appetite
Nausea or Vomiting
Nervousness
Night Sweats
Need to Get Out of Bed to Urinate?
Pain in Legs While Walking
Painful Urination
Pneumonia
Previous Mental Illness
Renal Failure/Iodine Allergies
Rheumatic Fever
Ringing in Ears
Seizures
Severe Nose Bleeds
Shortness of Breath W/Exertion
Shortness of Breath Laying Flat in bed
Sinus Problems
Spells of Unconsciousness
Stomach Ulcers
Stroke
Swelling of the Legs/Ankles
Syncope (fainting spells)
Thirst or Frequent Urination
Thyroid Disease
Tuberculosis
Urinary Tract Infections
Weight Change
Wheezing
Yellow Jaundice or Liver Disease
Migraine headaches
□ Yes □ No When? _________________
□ Yes □ No When? _________________
□ Yes □ No When? _________________
□ Yes □ No When? _________________
□ Yes □ No When? _________________
□ Yes □ No When? _________________
□ Yes □ No When? _________________
□ Yes □ No When? _________________
□ Yes □ No When? _________________
□ Yes □ No When? _________________
□ Yes □ No When? _________________
□ Yes □ No How often? _____________
□ Yes □ No When? _________________
□ Yes □ No When? _________________
□ Yes □ No When? _________________
□ Yes □ No When? _________________
□ Yes □ No When? _________________
□ Yes □ No When? _________________
□ Yes □ No When? _________________
□ Yes □ No When? _________________
□ Yes □ No When? _________________
□ Yes □ No When? _________________
□ Yes □ No When? _________________
□ Yes □ No When? _________________
□ Yes □ No When? _________________
□ Yes □ No When? _________________
□ Yes □ No When? _________________
□ Yes □ No When? _________________
□ Yes □ No When? _________________
□ Yes □ No When? _________________
□ Yes □ No When? _________________
□ Yes □ No When? _________________
□ Yes □ No When? _________________
□ Yes □ No When? _________________
□ Yes □ No When? _________________
□ Yes □ No When? _________________
□ Yes □ No When? _________________
Family History
Has anyone in your family (mother, father or sibling) had a heart attack? □ Yes □ No
If yes, how old were they when it occurred? __________________________________
Has anyone in your family (mother, father or sibling) had “sudden cardiac death” or died at a young age inexplicably?
□ Yes □ No
Mother:
If living, current age ______
History of heart disease: □ Yes □ No
If yes, what age diagnosed? ______
□
Diabetes
□
□
□
□
□
□
High Cholesterol
Hypertension
Coronary Artery Disease
Cardiomyopathy
Arrhythmias
Heart Failure
If deceased, age at death: ______
Cause of death: _______________________
Overall health of mother: ___________________________________________________
Father:
If living, current age ______
History of heart disease: □ Yes □ No
□
□
□
□
If yes, what age diagnosed? ______
□
Diabetes
□
□
High Cholesterol
Hypertension
Coronary Artery Disease
Cardiomyopathy
Arrhythmias
Heart Failure
If deceased, age at death: ______
Cause of death: _______________________
Overall health of father: ____________________________________________________
Siblings:
Age: _______ Sex: _______ Health: __________________________________________
Age: _______ Sex: _______ Health: __________________________________________
Age: _______ Sex: _______ Health: __________________________________________
Age: _______ Sex: _______ Health: __________________________________________
PAST MEDICAL HISTORY – Cardiac
Do you currently have or have ever had any of the following diseases?
Rheumatic Fever When diagnosed? _______________
Heart Murmur
Heart Attack (MI)
High Cholesterol
High Blood Pressure
□ Yes □ No
□ Yes □ No
□ Yes □ No
□ Yes □ No
□ Yes □ No
How treated? __________________
When diagnosed? _______________
How treated? __________________
When diagnosed? _______________
How treated? __________________
When diagnosed? _______________
How treated? __________________
When diagnosed? _______________
Diabetes
Irregular Heart Beat
How treated? __________________
When diagnosed? _______________
How treated? __________________
When diagnosed? _______________
Palpitations
Congenital Heart Disease
Valvular Heart Disease
Enlarged Heart
Cardiomyopathy
Congestive Heart Failure
□ Yes □ No
□ Yes □ No
□ Yes □ No
□ Yes □ No
□ Yes □ No
□ Yes □ No
□ Yes □ No
□ Yes □ No
How treated? __________________
When diagnosed? _______________
How treated? __________________
When diagnosed? _______________
How treated? __________________
When diagnosed? _______________
How treated? __________________
When diagnosed? _______________
How treated? __________________
When diagnosed? _______________
How treated? __________________
When diagnosed? _______________
How treated? __________________
When diagnosed? _______________
How treated? __________________
When diagnosed? _______________
Coronary Artery Disease
Peripheral Vascular Disease
□ Yes □ No
□ Yes □ No
PAST MEDICAL HISTORY - OTHER
COPD
Asthma
Emphysema
Kidney Disease
Liver Disease
Cancer
What type? ______________
Bleeding Disorders
□ Yes □ No
□ Yes □ No
□ Yes □ No
□ Yes □ No
□ Yes □ No
□ Yes □ No
□ Yes □ No
How treated? __________________
When diagnosed? _______________
How treated? __________________
When diagnosed? _______________
How treated? __________________
When diagnosed? _______________
How treated? __________________
When diagnosed? _______________
How treated? __________________
When diagnosed? _______________
How treated? __________________
When diagnosed? _______________
How treated? __________________
When diagnosed? _______________
Stroke (CVA or ICH) □ Yes □ No
Thyroid disorders (hyper, hypo) □ Yes □ No
How treated? __________________
When diagnosed? _______________
How treated? ___________________
When diagnosed? _______________
How treated? ___________________
Other major medical problems?
______________________________________________________________________________________
______________________________________________________________________________________
______________________________________________________________________________________
Have you ever had the following tests performed?
If you have, please bring a copy of the results with you.
Heart Catheterization
12 Lead EKG
Holter Monitor
Event Monitor
Nuclear Stress Test
Treadmill Stress Test
Echocardiogram
Dobutamine Stress Test
Adenosine Stress Test
CT/MRI
Vascular Ultrasound
Cardiac Device Adjustment
□ Yes □ No When/Where? _______________________
□ Yes □ No When/Where? _______________________
□ Yes □ No When/Where? _______________________
□ Yes □ No When/Where? _______________________
□ Yes □ No When/Where? _______________________
□ Yes □ No When/Where? _______________________
□ Yes □ No When/Where? _______________________
□ Yes □ No When/Where? _______________________
□ Yes □ No When/Where? _______________________
□ Yes □ No When/Where? _______________________
□ Yes □ No When/Where? _______________________
□ Yes □ No When/Where? _______________________
Surgical History
Previous surgeries:
Type Place When
______________________________________________________________________________________
______________________________________________________________________________________
______________________________________________________________________________________
______________________________________________________________________________________
______________________________________________________________________________________
______________________________________________________________________________________
Medications (taken regularly, including over the counter medications, vitamins, herbal supplements)
Please bring all of your medications with you.
Name Dosage Frequency (How often)
______________________________________________________________________________________
______________________________________________________________________________________
______________________________________________________________________________________
______________________________________________________________________________________
______________________________________________________________________________________
______________________________________________________________________________________
______________________________________________________________________________________
______________________________________________________________________________________
______________________________________________________________________________________
______________________________________________________________________________________
______________________________________________________________________________________
______________________________________________________________________________________
______________________________________________________________________________________
______________________________________________________________________________________
______________________________________________________________________________________
______________________________________________________________________________________
Allergies
Medication or other Reaction? When diagnosed?
________________________________________________________________________
________________________________________________________________________
________________________________________________________________________
________________________________________________________________________
________________________________________________________________________
________________________________________________________________________
Major Hospitalizations
Reason for Admission Where? When?
________________________________________________________________________
________________________________________________________________________
________________________________________________________________________
________________________________________________________________________
________________________________________________________________________
________________________________________________________________________
________________________________________________________________________
Patient Signature__________________________________________Date____________
Physician Signature________________________________________Date____________