Professional Ethics, Health Care and Ethics
advertisement
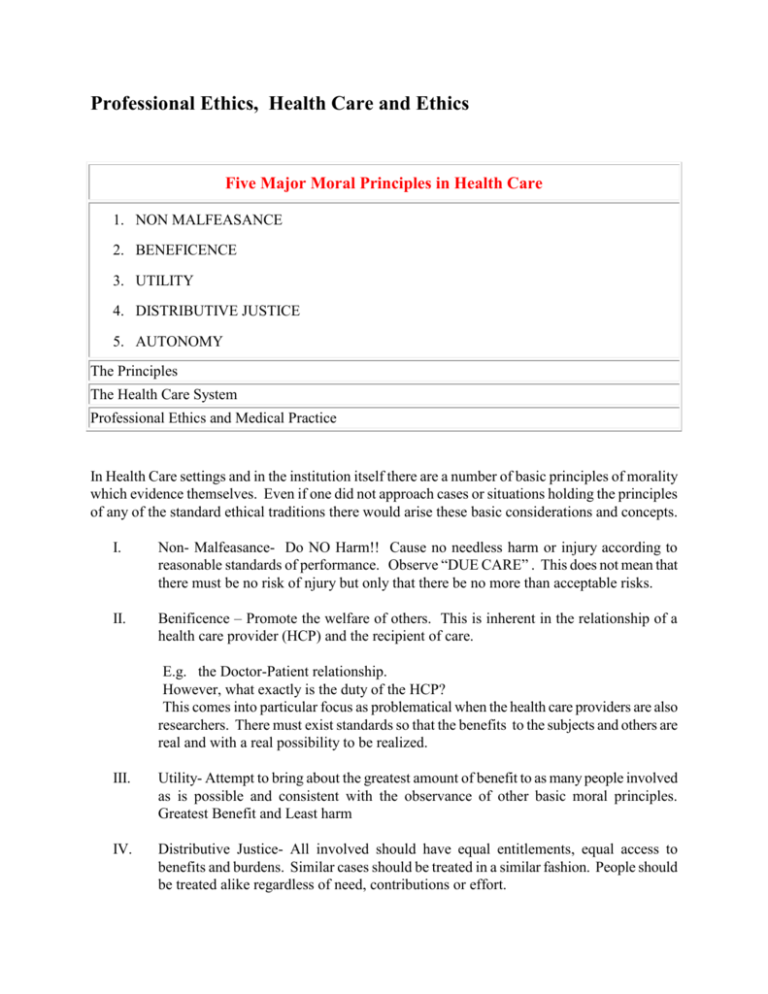
Professional Ethics, Health Care and Ethics Five Major Moral Principles in Health Care 1. NON MALFEASANCE 2. BENEFICENCE 3. UTILITY 4. DISTRIBUTIVE JUSTICE 5. AUTONOMY The Principles The Health Care System Professional Ethics and Medical Practice In Health Care settings and in the institution itself there are a number of basic principles of morality which evidence themselves. Even if one did not approach cases or situations holding the principles of any of the standard ethical traditions there would arise these basic considerations and concepts. I. Non- Malfeasance- Do NO Harm!! Cause no needless harm or injury according to reasonable standards of performance. Observe “DUE CARE” . This does not mean that there must be no risk of njury but only that there be no more than acceptable risks. II. Benificence – Promote the welfare of others. This is inherent in the relationship of a health care provider (HCP) and the recipient of care. E.g. the Doctor-Patient relationship. However, what exactly is the duty of the HCP? This comes into particular focus as problematical when the health care providers are also researchers. There must exist standards so that the benefits to the subjects and others are real and with a real possibility to be realized. III. Utility- Attempt to bring about the greatest amount of benefit to as many people involved as is possible and consistent with the observance of other basic moral principles. Greatest Benefit and Least harm IV. Distributive Justice- All involved should have equal entitlements, equal access to benefits and burdens. Similar cases should be treated in a similar fashion. People should be treated alike regardless of need, contributions or effort. The formal principle of Justice as Fairness (Rawls’ Theory) similar cases are to receive the same treatment. However, in what ways are the cases similar? In what relevant ways? V. Autonomy- People are rational, self determining beings who are capable of making judgments and decisions and should be respected as such and permitted to do so and supported with truthful and accurate information and no coercion. They should have their actions: free of duress, options explained that are genuine possibilities and given the information for decision making. RESTRICTIONS on AUTONOMY: 1. HARM- stop an individual from causing harm 2. PATERNALISM- weak – stop a person from self harm Strong – to benefit a person 3. LEGAL MORALISM- legislated morality 4. WELFARE PRINCIPLE- for the benefit of all Health Care System COMPONENTS: Providers: primary and secondary(medical schools, professional associations, drug suppliers,etc..) Consumers Mechanisms for financing/supporting the institution VALUES A. HUMANITARIAN Freedom, Dignity, Privacy, Autonomy B. FREE ENTERPRISE Market System Technology C. INSTITUTIONAL a. Efficiency b. Economy Free Enterprise Self Interest Technology Institutional Clash of Values Individual Welfare Benefit of Others Dignity and Comfort Human Social Function of Health Care: a. Health Care b. Employment c. Knowledge Bureaucratic Model versus the Human Hierarchy of Control and Authority Division of Labor with identifiable goals Values of: Industry, efficiency, predictability and speed>>>Impersonal Operational Problems: i. Non-routine tasks ii. Internal dynamics iii. Conflicting values iv. Separation of patients from social context into institutional context (persons become patients) v. Information Control- elitism, paternalism vi. Communications Breakdown vii. Dilution of Authority viii. Displacement of Authority ix. Development of sub groups Professional Model Based on : Education- professional organizations Code- licensing, association, peer control VALUES: Autonomy, Collegiality, Service to Others, Skill Professional Model clashes with the Bureaucratic Model Tensions develop Medical versus Administrative Line of Authority Service versus Economic Good Specialized labor versus Flexibility Authority based on expertise versus Authority based upon Position Role Conflicts Incompatible Role Expectations RN < a. b. c. d. e. > MD Relationship educational status career patterns semantic differences class differences authority differences f. sex differences g. different orientations: care versus cure h. different amounts of time with recipients of care Three Cases 1. Whistle Blowing 2. Truth Telling 3. Letting Die Ethics in the Context of Professional Activities Definition of a Profession Definition of Ethics Medical Practice and Models 2 sets of Basic Relations (A) Physician >Patient (B) Physician > Physician 1. 2. 3. 4. 5. Paternalistic (Authoritarian) Employer (less Authoritarian) Collegial (non-authoritarian) Contractual (non-authoritarian) Possible return to COVENENTIAL Models based upon Governing Ideals, Conceptual Frameworks, Perspectives I. Code II. Contract III. Covenant CODE 1. Unwritten, traditional guides, rules: technical proficiency 2. Written, official pronouncements: etiquette, philanthropy 3. Special language, initiation rites, secrecy, DUTIES, professional Guild a. Anti-competition monopoly –price fixing, sliding scale b. Group solidarity Aesthetic code- life style, image, decorum- beautiful life Concern for colleagues is greater than that for those served Five (5) factors militate against self-criticism and self regulation 1. Sense of community 2. 3. 4. 5. Power of the priestly caste Power of the modern physician unstable- based on power over death Suspicion of officiousness, injustice, hypocrisy Basic conflict- 2 sets of obligations: to guild and to patient Obligations to colleagues Responsive, obligation and a debt Obligations to patients are: self-incurred and duties Physician > guild, colleagues, teachers, progeny Hippocratic Oath 1. codal duties to patients 2. Conventional obligations to colleagues 3. context of oath –gods a. no reference to gift b. no promises Initiatory Oath- Code- Covenant as chosen, profession and a transformation CONTRACT Pro : 1. Symmetry 2. Legal enforcement 3. Self-interest and not philanthropy, e.g., informed consent Against: 1. Minimalism 2. Unpredictability 3. Maximalism- Defense Mechanism 4. Inequality 5. No freedom of choice 6. Denies transcendent rights and duties COVENANT Key elements are promise and fidelity to the promise 1. 2. 3. 4. 5. Responsive Debt Obligation Canon of Loyalty, Fidelity (truth, promises, care) not proficiency Change in Being- ontological nature, e.g., temporal aspect of being Problems with this model: Needs a transcendent reference for the proper context: Transcendent norm for rights and duties of physicians and patients Transcendent source of limits for expectations and duties Pro: 1. Not so personal- applies to the whole profession, a covenant with society broadens accountability 2. Permits setting Professional responsibility for one human good (health) within social limits Physicians’ indebtedness established by five (50 factors: 1. 2. 3. 4. 5. Education Privileges Social Largess- payments for services Experimental Subjects Continual Support of profession and individuals Covenant includes and extends beyond code and contract a. Includes code: fidelity to duty, responsibilities to patients and colleagues b. Includes contract- terms of contract- fidelity Covenant requires more- a surplus of obligations to society are is final advantage Obligations (debts) to society are greater than debts to colleagues Permits possibility of self-discipline Patient Role relates to the Physician’s image Physician- as parent, priest Technician Contractual partner Covenantor patient as dependant Passive host of disease Equal participant Active participant Mutual reciprocal rights and duties, gifts and debts, promises and obligations Application of the models and images to the three cases