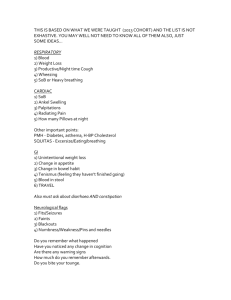
History & Physical Exam
advertisement
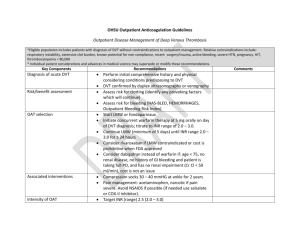
Emily Koch ACNP program Medicine History and Physical Examination Chief Complaint: SOB, DOE, cough, chest/back pain HPI: Mr. M. is a 57 y.o. male with PMH significant for obesity, HTN, and DVT in 2007 who presents to clinic with worsening SOB and DOE over the past 2 months and recently developed cough, hemoptysis, and chest/back pain with deep inspiration. He is not able to walk short distances without becoming dyspneic, and patient reports that he was able to walk 3 miles without SOB 2 months ago. He also reports 1 episode of palpitations and diaphoresis that occurred 1 week ago and resolved spontaneously when he laid down. Within the last 3-4 days, the SOB is not always relieved by rest and when he presented to clinic, he reports that his RA oxygen saturation was 85%. He denies recent air travel, leg injuries, surgeries, and confirms his usual level of physical activity on most days. His current employment involves finishing dry wall, which he confirms exposes him to significant volumes of dust regularly. PMH: HTN, obesity, perirectal abscess requiring sgy in 2007. DVT, 2007 Code Status: Full Vaccines: does not have current Pneumococcal or Influenza vaccines Social History: lives alone, mother recently died, supportive brothers, 70 pack year smoking history and quit smoking tobacco 2000; denies ETOH abuse current or past Family History: Father died at 79 of CAD, COPD; Mother died at 79 of esophageal CA, asthma Allergies: NKDA Medications: aspirin 81 mg daily, HCTZ 25 mg daily, lisinopril 20 mg daily ROS: Constitutional: Denies fever, chills, night sweats HEENT: non-contributory Cardiovascular: Per HPI; difficulty sleeping supine, chronic LLE swelling since DVT 2007 Respiratory: Per HPI; snores GI: indigestion GU: non-contributory Musculoskeletal: weakness over past 2 months Skin: non-contributory Neurological: Denies numbness, tingling Endocrine: non-contributory Hematologic/Lymphatic: Denies that he bruises easily or bleeds excessively Psychiatric: non-contributory Physical Exam: This is a pleasant, obese, well-developed male in mild distress r/t SOB and pain with deep inspiration. VS: 36.1, 98. 22. 120/72. 93% O2 sat on 2 L; 6’1” 150.9 kg, BMI 45 HEENT: normal (Head: normocephalic, atraumatic; Neck: supple, FROM, trachea midline, no carotid bruits, no JVD; Nose: septum midline, moist mucus membranes, no cough/sputum production during exam) CV: S1/S2 distant, no murmurs/rubs/gallops/clicks, +2 pulses Bilaterally and symmetrical throughout, trace LE edema Lungs: diminished breath sounds with faint upper airway wheeze, shallow but symmetrical chest expansion, tachypneic, no stridor, no egophony, no fremitus Abd: normal (soft, nontender, obese, normoactive bowel sounds, no masses/organomegaly) MS: exam deferred due to SOB/DOE, no joint tenderness Lymph: no lymphadenopathy Neuro: normal (A&O x 4, no focal neuro deficits) Skin: pink, warm, moist Psyc: mood is calm, pleasant. Laboratory & Radiology Review: Na 137 K 4.1 Cl 98 CO2 26 BUN 22 Creat 1.6, eGFR 49 Glucose 122 WBC 10.25 Hgb 12.6 Hct 38.9 Platelets 160 Ca 8.6 Mg 1.9 Phos 3.9 D-dimer 2510 CTPA: large burden diffuse pulmonary thromboemboli, Right heart strain likely based on septal bowing, Bilateral lower lobe atelectasis, RV enlarged, 2 mm nodule RML, coronary artery calcifications are seen. Echocardiogram: trace mitral regurgitation, EF 60-65%, normal LV function and size, pulmonary valve and RV not well visualized. Assessment: This is a 57 y. o. male with PMH DVT treated with 6 months of anticoagulation, obesity, HTN presenting with SOB, DOE, hemoptysis, and pleuritic pain. (Before laboratory and radiology review differential diagnoses include pulmonary embolism, MI, dysrhythmia, new HF, PNA, COPD, flu. I would rule out PE by CTPA, MI by ECG and troponins, dysrhythmia by continuous telemetry during hospitalization and CMP, HF by echocardiogram and BNP, PNA/flu by CXR and CBC with differential and blood cultures, and COPD by PFTs.) Plan: 1. Massive PE a. Respiratory support – oxygen to maintain O2 sat >92%, ABGs to evaluate adequacy of oxygenation and ventilation. Severe hypoxemia or respiratory distress should prompt intubation and mechanical ventilation. (Patients with coexistent RV failure may be prone to hypotension after intubation) b. Monitor hemodynamic status – if hypotensive consider normal saline IV bolus carefully, start with 500ml if systolic BP drops below 90. IV fluids can increase RV wall stress and decrease ratio of RV oxygen supply to demand and result in worsening RV function. If small fluid bolus is not sufficient for BP support, patient may require vasopressors. c. Anticoagulation – Heparin continuous infusion 18 units/kg/hour after initial bolus of 80 units/kg. Check PTT every 6 hours until therapeutic and then every 24 hours. Adjust Heparin gtt based on hospital nomogram. Outpatient anticoagulation – enoxaparin 1 mg/kg q 12 hours. Indefinite Warfarin therapy is indicated for 2 or more episodes of DVT/PE. Start Warfarin 5 mg daily, check INR in two days, adjust and check 3 days after each adjustment and then every 2-4 weeks when therapeutic. INR goal is 2-3. d. Work-up etiology – evaluate for clotting disorders. i. Get Hematology/Oncology consult. Send labs for Factor V, II Leiden PCR; dRVVT (lupus anticoag), antiphospholipid antibody syndrome. Consider malignancy, particularly lung, prostate, pancreas, stomach, colon, leukemia, Trousseau’s syndrome. e. Consider risk/benefits of thrombolytic therapy. Hemoptysis most likely renders patient poor candidate, but discuss with Hematology or Pulmonology. Thrombolysis may improve RV function and pulmonary perfusion. (tPA 100 mg over 2 hours.) f. Consider IVC filter if patient is not a candidate for thrombolysis and/or if complications to anticoagulation develop. g. Get Cardiology consult for recommendations on managing RV strain and preventing cor pulmonale. May need cardiac catheterization. (ECG findings in PE: Twave inversions V1-V4, sinus tachycardia, S1Q3T3 pattern [the classic signs are a large S wave in lead I, a large Q wave in lead III and an inverted T wave in lead III], complete/incomplete RBBB) 2. AKI a. Hold lisinopril, HCTZ, check urine electrolytes, gentle hydration after IV contrast dye. (eGFR should be >30ml/min in patients receiving contrast dye and discretion should be used in patients with eGFR <45ml/min. Following up with extra fluids is highly recommended.) 3. Discharge follow up a. Patient needs to be seen by outpatient cardiologist for stress test and possible cardiac catheterization and/or EP study if prolonged palpitations recur. Consider cardiac event monitor if recurrent palpitations. He could be experiencing intermittent Afib. b. Patient should come back as outpatient for sleep study and PFTs to evaluate for OSA and COPD, respectively.