File - Wk 1-2
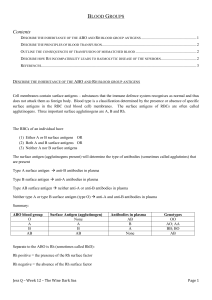
1. Describe the inheritance of the ABO and Rh blood group antigens
The antigens expressed on the red blood cell determine an individual's blood group.
The main two blood groups are called ABO (with blood types A, B, AB, and O) and
Rh (with Rh D-positive or Rh D-negative blood types).
The functions of many of the blood group antigens are not known, and if they are missing from the red blood cell membrane, there is no ill effect. But the presence or absence of red blood cell antigens becomes extremely important when blood from different individuals mix, ie. when a patient receives a blood transfusion. This also happens when a pregnant mother experiences a small amount of fetal blood entering her circulation. In these circumstances, exposure to the foreign antigens on the red blood cells can trigger immune reactions which can have adverse health effects
ABO Inheritance
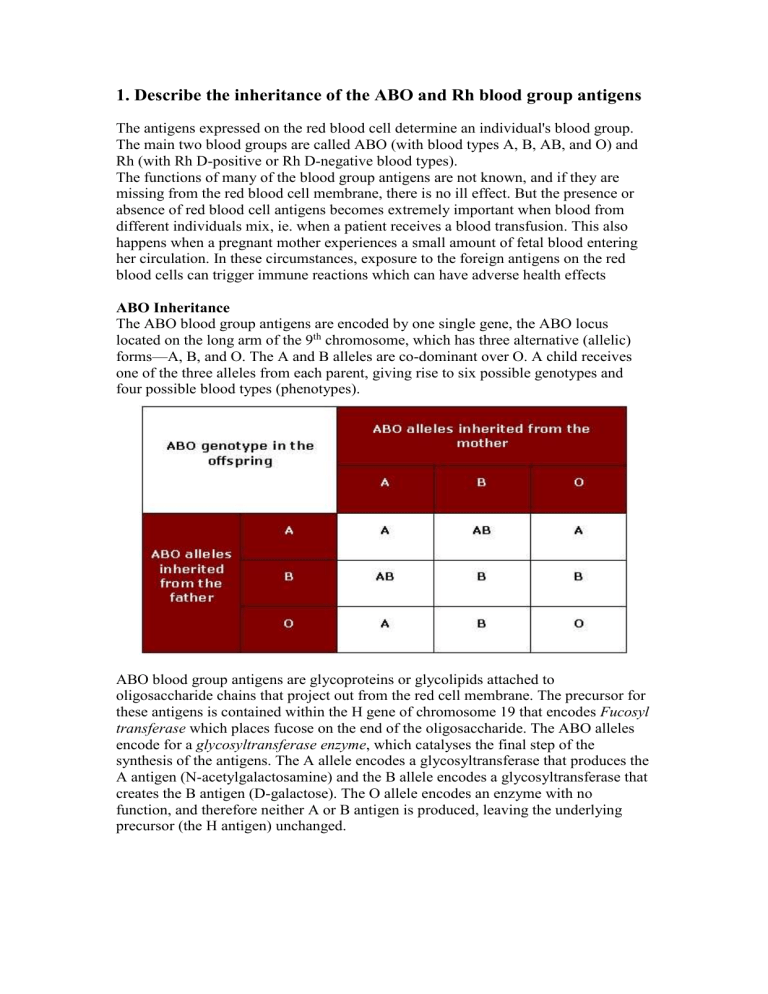
The ABO blood group antigens are encoded by one single gene, the ABO locus located on the long arm of the 9 th
chromosome, which has three alternative (allelic) forms—A, B, and O. The A and B alleles are co-dominant over O. A child receives one of the three alleles from each parent, giving rise to six possible genotypes and four possible blood types (phenotypes).
ABO blood group antigens are glycoproteins or glycolipids attached to oligosaccharide chains that project out from the red cell membrane. The precursor for these antigens is contained within the H gene of chromosome 19 that encodes Fucosyl transferase which places fucose on the end of the oligosaccharide. The ABO alleles encode for a glycosyltransferase enzyme , which catalyses the final step of the synthesis of the antigens. The A allele encodes a glycosyltransferase that produces the
A antigen (N-acetylgalactosamine) and the B allele encodes a glycosyltransferase that creates the B antigen (D-galactose). The O allele encodes an enzyme with no function, and therefore neither A or B antigen is produced, leaving the underlying precursor (the H antigen) unchanged.
Rh Inheritance
The Rh blood group system is in most cases attributable to two genes, RhD and
RhCE, which are located on chromosome 1. However the most immunogenic and hence clinically relevant is the RhD antigen. The RhD gene is dominant and so whenever present a person is considered to be RhD positive even though they may have only inherited the gene from one parent. If no RhD gene has been inherited a person will be RhD negative.
2. Explain briefly the principles of the agglutination reaction
The immune system forms antibodies against whichever blood group antigens are not found on the individual's RBCs. Thus, with ABO blood groups, a group A individual will have anti-B antibodies and a group B individual will have anti-A antibodies.
Blood group O is common, and individuals with this blood type will have both anti-A and anti-B in their serum. Blood group AB is the least common, and these individuals will have neither anti-A nor anti-B in their serum. ABO antibodies in the serum are formed naturally. Their production is stimulated when the immune system encounters the "missing" ABO blood group antigens in foods or in micro-organisms. This happens at an early age because sugars that are identical to, or very similar to, the
ABO blood group antigens are found throughout nature.
An antigen is any substance to which the immune system can respond. If the immune system encounters an antigen that is not found on the body's own cells, it will launch an attack against that antigen. If this is the first time the antigen has been encountered, a primary immune response is mounted. Usually there is a delay of several days, and then IgM antibody is produced, followed by a switch to IgG antibody production later on. The initial IgM molecules bind the antigen weakly, but the subsequent IgG molecules are much better targeted. IgG continues to be produced long after the encounter with the antigen, providing long-lasting immunity.
If the immune system has encountered the antigen before, it will already be armed with primed B cells (memory cells) that accelerate the production of larger amounts of IgG (rather than IgM). This is called the secondary immune response. It is faster, more specific, and the production of the specific antibody may remain high for years.
B cells may also undergo changes to further improve how the antibodies they produce bind to the antigen.
There are two main arms of immune response - humoral (using antibodies) and cellular (using immune cells). In the case of a foreign red blood cell antigen, the patient's pre-existing antibodies bind to the antigen, coating the donor RBCs.
Some types of antibody may activate the complement cascade, a series of enzymedriven reactions involving protein fragments. The cascade ends with the formation of a "membrane attack complex", a large molecule that punches a hole in the cell membrane. Other antibodies simply bind to the donor RBCs and cause them to stick clump together (agglutinate) with potentially fatal results. This consequently has major implications for the application of blood transfusions. The threat in blood transfusion is that the donor's RBCs may be rapidly agglutinated by the recipient's antibodies as the RBCs enter the recipient's bloodstream.
To avoid these adverse reactions, “cross-matching” of a patient’s blood type is done prior to transfusion. In serological cross-matching, red blood cells from the donor unit are tested against the plasma of the patient in need of the blood transfusion. If the patient’s serum contains antibodies against the antigens present on the donor red blood cells, agglutination will occur. Agglutination is considered a positive reaction indicating that the donor unit is incompatible for that specific patient. If no agglutination occurs the unit is deemed compatible and is safe to transfuse.
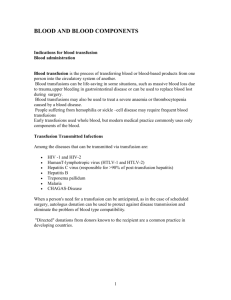
3 & 4. Describe the principles of blood transfusion and the consequences of transfusion of mismatched blood
A blood transfusion is transfer of blood from one person to another or from one animal to another of the same species. Transfusions are performed to replace a substantial loss of blood and/or as supportive treatment in certain diseases and blood disorders. When whole blood is not needed, or when it is not available, plasma (the fluid of the blood without the blood cells) can be given. Alternately, such components of the blood as red cells, white cells, or platelets may be given for particular deficiencies
In whole-blood transfusions, the blood of the donor must be compatible with that of the recipient. Blood is incompatible when certain factors in red blood cells and plasma differ in donor and recipient. When this occurs, agglutinins (antibodies) in the recipient's blood will clump with the red blood cells of the donor's blood. The most
frequent blood transfusion reactions are caused by substances of the ABO blood group system and the Rh factor system. In the ABO system, group AB individuals are known as universal recipients, because they can accept A, B, AB, or O donor blood.
Persons with O blood are sometimes called universal donors, since their red cells are unlikely to be agglutinated by the blood of any other group. In the Rh factor system, agglutinins are not produced spontaneously in an individual but only in response to previous exposure to Rh antigens, as in some earlier transfusion. Transfusion reactions involving incompatibility eventually cause hemolysis, or disruption of donor cells. The resulting liberation of haemoglobin into the circulatory system, causing jaundice and kidney damage, can be lethal.
In addition to providing for the compatibility of blood groups in transfusion, it is necessary to determine that the donor's blood is free of organisms that might cause syphilis, malaria, hepatitis, or HIV.
Blood can only be administered intravenously, and a unit (up to 500 ml) is typically administered over 4 hours. It therefore requires the insertion of a cannula of suitable calibre (size!!). Before the blood is administered, the personal details of the patient are matched with the blood to be transfused, to minimize risk of transfusion reactions.
Clerical error is a significant source of transfusion reactions and attempts have been made to build redundancy into the matching process that takes place at the bedside.
The consequences of transfusions of mismatched blood result in a haemolytic transfusion reaction, which may occur immediately (acute) or after a period of days
(delayed). The symptoms produced by these transfusion reactions are often similar, beginning with chills, fever, shaking, and aching. Some transfusion reactions are mild and resolve by themselves whereas others can develop into a life-threatening reaction.
Complications include;
Embolism related events
Jaundice due to excess destruction of RBCs
Circulatory overload – hypervolemia, excessive bleeding, pulmonary oedema
Hives
Anaphylaxis
Renal failure
Vessel occlusion (due to agglutination reactions)
Infection with various blood-borne diseases
5. Describe how Rh incompatibility leads to haemolytic disease of the newborn (HDN)
The Rh factor or Rhesus system got its name from the fact that it was first reported in erythrocytes of the Rhesus monkey by Landsteiner and Wiener (1940). About 85 per cent of white people are Rh positive (Rh
+
), i.e., have the Rh antigen in their erythrocytes, and 15 percent are Rh negative (Rh
-
), with no Rh antigen. If a woman is
Rh negative and her husband Rh positive, the fetus may be Rh positive, having inherited the factor from its father.
Sensitization to an antigen occurs when the immune system encounters an antigen for the first time and mounts an immune response. In the case of HDN caused by Rh
incompatibility, an RhD-negative mother may first encounter the D antigen while being pregnant with an RhD-positive child, or by receiving a blood transfusion of
RhD-positive blood. Once a mother has been sensitized to the D antigen, her serum will contain anti-RhD antibodies. Only a small amount of fetal blood need enter the mother's circulation for sensitization to occur. Typically, this occurs during the delivery of the first-born RhD-positive child. Sensitization can also occur earlier in the pregnancy, for example during a prenatal bleed or a miscarriage. It may also occur during medical procedures, such as a termination of pregnancy or chorionic villus sampling.
Initially, the maternal anti-D that is formed at the time of sensitization is of the IgM type, which can not cross the placenta. In subsequent pregnancies however, a repeat encounter with the RhD antigen stimulates the rapid production of type IgG anti-D, which can be transported across the placenta and enter the fetal circulation. Once in the fetal circulation, anti-D attaches to the RhD antigens found on the fetal RBCs, marking them to be destroyed.