Flanagan_Supplementary Information_R1
advertisement

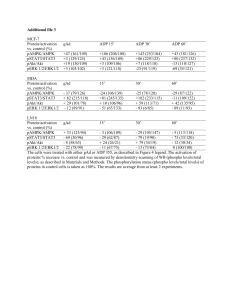
Supplementary Information Early-onset Multi-Organ Autoimmunity Caused by Activating Germline Mutations in STAT3 Sarah E. Flanagan,1, 13 Emma Haapaniemi,2,13 Mark A. Russell,1,13 Richard Caswell,1 Hana Lango Allen,1 Elisa De Franco,1 Timothy J. McDonald,1 Hanna Rajala,3 Anita Ramelius,4 John Barton,5 Kaarina Heiskanen,6 Tarja Heiskanen-Kosma,7Merja Kajosaari,8 Nuala P. Murphy,9 Tatjana Milenkovic,10 Mikko Seppänen,11 Åke Lernmark,4 Timo Otonkoski,6 Satu Mustjoki,3 Juha Kere,2,12 Noel G. Morgan,1 Sian Ellard1 and Andrew T. Hattersley1 1 Institute of Biomedical and Clinical Science, University of Exeter Medical School, Exeter, EX2 5DW, UK Folkhälsan Institute of Genetics, and Research Programs Unit, Molecular Neurology, University of Helsinki, Helsinki, Finland 3 Hematology Research Unit Helsinki, Department of Hematology, University of Helsinki and Helsinki University Central Hospital Cancer Center, Helsinki, Finland 4 Department of Clinical Sciences, Lund University/CRC, Skåne University Hospital SUS, Malmö, Sweden 5 Bristol Royal Hospital for Children, Upper Maudlin Street, Bristol, BS2 8BJ, UK 6 Children’s Hospital, Helsinki University Central Hospital and Research Programs Unit, Molecular Neurology, University of Helsinki, Helsinki, Finland 7 Department of Pediatrics, Kuopio University Hospital, Helsinki, Finland 8 Children’s Hospital, Helsinki University Central Hospital, Helsinki, Finland 9 Department of Diabetes and Endocrinology, Children's University Hospital, Temple St., Dublin 1, Ireland 10 Department of Endocrinology, Institute for Mother and Child Health Care of Serbia ‘Dr Vukan Cupic’, Belgrade, Serbia 11 Immunodeficiency Unit, Division of Infectious Diseases, Helsinki University Central Hospital, Helsinki, Finland 12 Department of Biosciences and Nutrition, and Center for Innovative Medicine, Karolinska Institutet, Hälsovägen 7, 14183 Huddinge, Sweden 13 These authors contributed equally to this work 2 Table of Contents Supplementary Methods ……………. Supplementary Table 1 ………………. Supplementary Table 2 …………….. Supplementary Table 3 …………….. Supplementary Table 4 …………….. Supplementary Table 5 …………….. Supplementary Table 6 …………….. References …………… Supplementary Methods Cohort selection and sample preparation Twenty-five individuals with early-onset polyautoimmune disease (diagnosed before 5 years of age) and 39 subjects with isolated permanent diabetes diagnosed before 6 months were recruited by their clinicians for molecular genetic analysis in the Exeter Molecular Genetics Laboratory (n=63) or the Folkhälsan Institute of Genetics, University of Helsinki (n=1). Genomic DNA was extracted from peripheral leukocytes using standard procedures. All subjects and/or their parents gave informed consent for genetic testing and institutional review board approval was received for this study. Exome sequencing and variant calling Genomic regions corresponding to NCBI Consensus Coding Sequence (CCDS) database were captured and amplified using Agilent’s SureSelect Human All Exon Kit (v1). Paired-end sequencing was performed on an Illumina GAII, one lane per sample, 101 or 76bp read length. The resulting reads were aligned to the hg19 reference genome with BWA providing mean target coverage of 66.3 reads per base. At least 72% of the targeted bases were covered by at least 20 reads. Variants were called with GATK UnifiedGenotyper and annotated using Annovar and SeattleSeq Annotation server, as previously described.1 Variant filtering steps are shown in Supplementary table 1. STAT3 sequencing and microsatellite analysis Sanger sequencing was undertaken in patient 1 and her unaffected parents to confirm that the p.T716M STAT3 variant had arisen de novo. Exons 2-24 and intron/exon boundaries of STAT3 (NM_139276.2) were Sanger sequenced in a further 24 individuals with at least 2 early-onset autoimmune features of unknown cause (Supplementary table 2). Primers for STAT3 exons 2-24 are provided in Supplementary table 3. Targeted next-generation sequencing of STAT3 was undertaken on a further 39 individuals with isolated permanent diabetes diagnosed before the age of 6 months of unknown cause without additional autoimmune features. All patients were less than 5 years of age at the time of genetic testing. We adapted our custom Agilent SureSelect exon-capture assay (Agilent Technologies, Santa Clara, CA, USA) to include baits for exons 2-24 and intron/exon boundaries of STAT3 (sequences available on request to authors.2 Samples were fragmented using a Bioruptor (Diagenode, Liège, Belgium), indexed for multiplexing and hybridised (in pools of 12 samples) according to the manufacturer’s instructions. Sequencing was performed with an Illumina HiSeq 2000 (Illumina, San Diego, CA, USA) (48 samples per lane) and 100 bp paired end reads. Data were processed to identify potential pathogenic mutations located within 50 bp upstream and 10bp downstream of each exon. We identified STAT3 mutations in a further 3 individuals with early onset autoimmune disease (4 of 25, 16% of cohort) and 1 individual with permanent neonatal diabetes (1 of 39, 2.6% of cohort). This brought the total number of STAT3 positive subjects to 5. Sanger sequencing of parental samples confirmed all mutations had arisen de novo. Biological relationships were confirmed by microsatellite analysis using the PowerPlex kit (PowerPlex 16 System, Promega, Southampton, UK). In total four different mutations were identified in 5 unrelated individuals. All mutations affected residues in the highly conserved DNA binding domain (x1), SH2 domain (x2) and transactivation domain (x1) (conserved to Zebrafish). None of the mutations were present in dbSNP132, 1000 Genomes Project database (based on 1094 individuals) or the Exome Sequencing Project (based on 6500 individuals). Functional studies of STAT3 mutations Mutations within human STAT3 (Source Bioscience) were generated using the QuikChange sitedirected mutagenesis kit following the manufacturer’s guidelines (Agilent Technology). The primer pairs used to generate each mutant are provided in Supplementary table 4. The success of all mutatagenesis reactions was confirmed by direct sequencing of the entire STAT3 insert (Eurofins). Following mutagenesis, STAT3 inserts were subcloned into the multiple cloning site of a pcDNA5/FRT/TO expression vector between AflII and EcoRV restriction sites. The transcriptional activity of STAT3 was assessed via a STAT3 responsive dual firefly/Renilla luciferase Cignal reporter system (Qiagen). HEK293 cells were seeded at a density of 1 x 10 5 cells/well, and were transfected after 24h with a combination of 200ng Cignal reporter assay constructs and 400ng WT or mutant STAT3 pcDNA5/FRT/TO using the Attractene transfection reagent according to the manufacturer’s instructions (Qiagen). Cells were incubated in the transfection mix for 24h and, where appropriate, 20ng/ml IL-6 was also included for the final 18h. STAT3 reporter activity was assessed using a dual luciferase reporter assay system (Promega). To confirm that equivalent amounts of STAT3 protein were expressed following transfection of each construct, cells were lysed and protein extracted prior to Western blotting with anti-STAT3 antibody (Cell Signalling) as described previously5. FACS analysis of patient cells For the assessment of T-cell activation and degranulation, fresh mononuclear cells from patients 2 and 5 (supplementary table 5) were stimulated for 6 h with anti-CD3, anti-CD28 and anti-CD49d (BD Biosciences). The cells were analyzed using 4- or 6 colour flow cytometry panel with mAbs against the antigens CD3, CD4, CD8, IFN-γ and TNF-α. Supplementary Table 1. Breakdown of variants identified by exome sequencing of individual 1 Individual 1 Total passing quality filters After dbSNP131 filtering After 1000Genomes filtering After excluding those in parents (de novo) After excluding those outside of the coding regions and conserved splice sites (+/- 2bp) After excluding non-synonymous and intronic variants After manual inspection and exclusion of putative de novo variants present in a parent substitutions indels 18220 570 466 489 95 16 18 1 15 0 7 0 1 0 1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 18 19 20 21 22 23 24 25 STAT3 mutation identified Dental anomalies Autoimmune joint disease Autoimmune thyroid dysfunction Autoimmune pulmonary disease Autoimmune Enteropathy Early-onset diabetes Patient Supplementary Table 2: Features of 25 individuals with multiple early onset-autoimmune disease sequenced for STAT3 mutations p.T716M p.K392R p.N646K p.K658N No No No No No No No No No No No No No No No No No No No No No Supplementary Table 3: STAT3 primers for Sanger sequencing Exon 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 18F 18R 19 20 21 22 23 24 Forward Primer Sequences (M13 tailed) Reverse Primer Sequences (M13 tailed) All primers start 5’ TGTAAAACGACGGCCAGT All primers start 5’ CAGGAAACAGCTATGACC CCCCAGAGCATCTTTATCCC GGGTTATAGCATCAGGTTTGC TAGTAACGACCTCCCCTTCG TTCCCTTCCTCTTGTGATGG AACAGGGAGCCTTCTCTTGG GGAGGTACGGGTCCTCAAAG ATTTCAGCGTCTTGTGGCAG TTTTCAGCATCCACCCAAC GGTAATTTAGCATCCTTGTCCC GACAGCTTGGCCTATTTACCTG TGCGCTGATCAACTGTAACTG ATTCCCACATCTCTGCTCCC ATGGAAGAATCCAACAACGG TGCTGCTTAGACTGGTCTCG CACTCCTCGCCTAGAGTTGG AACATGCTGACCAACAATCC AAATCCTCAGGCCCGTCTAC CCTTCAAAGATGTGAAAGCTG CTGAACTCTTGGTCCAGCG GCTGGCAAGGGCTTCTC CACTACAATTCTTTCCCATAAGGAG TAAATGAGGGCAGACAACCC AGCCCCTGGGCTATGTTTAG TCCAGGGAGGAGGGTAAATC CTCATTTTCCCCATCACCTG AAGTATACAGAGCTTTGAGAAAGGG TCTGTTGGATTCTTTTGGTGG CAAGAGAAGGCTCCCTGTTG ATGACCAGGCTCCTTTGAGG CAACTCCAGAGCAGGAACTTCT GCTAAATTTGAATATGGAAAAGTCC GGAAAGAGAAGATGGGCTCAC ATGGCAACAAATTTCAACCC TGTCCACAAAATGAAGATCTCTG ATTCCCACATCTCTGCTCCC TGCGCTGATCAACTGTAACTG GTTCATGTCACTTTGGCCTG CCCCTGTACGTAGCCTCTCA GTCCTCGCTTGGTGGTG GCCTTGCTCAGGAAAGAAAC CCTTCAAAGATGTGAAAGCTG AAATCCTCAGGCCCGTCTAC AAAGCCCATGATGTACCTGG AAGCAAACCAATCCTTCAGC AACAGGGTGTTCAGGGTCTC TCAAACTCTGGTCTCCAACAG TCTCTTTTGGAAAGCAAAGCTC AGCAGATCACCCACATTCAC Supplementary Table 4: Primer sequences for site-directed mutagenesis Mutation Forward Primer Reverse Primer Polyautoimmune mutations: p.K392R ATTCTGGGCACAAACACAAGAGTGATGAACATGGAAG TCTTCCATGTTCATCACTCTTGTGTTTGTGCCCAGAATG p.N646K ACACAAAGCAGCAGCTGAAGAACATGTCATTTGCTG AGCAAATGACATGTTCTTCAGCTGCTGCTTTGTG p.K658N TCATCATGGGCTATAACATCATGGATGCTACC TGGTAGCATCCATGATGTTATAGCCCATGATG p.T716M ATCTGTGTGACACCAATGACCTGCAGCAATACC TGGTATTGCTGCAGGTCATTGGTGTCACACAG Hyper IgE mutations: p.R382W AGCTCTCAGAGGATCCTGGAAATTTAACATTCTGGGC TGCCCAGAATGTTAAATTTCCAGGATCCTCTGAGAGC p.V637M AGACCCAGATCCAGTCCATGGAACCATACACAAAG TGCTTTGTGTATGGTTCCATGGACTGGATCTGGGTC Supplementary Table 5: Clinical characteristics of individuals with a de novo STAT3 mutation PATIENT 1 PATIENT 2* PATIENT 3 PATIENT 4 PATIENT 5 Table of clinical features Mutation Sex Current Age (yrs) Birth weight (SDS) p.Thr716Met (c.2147C>T) Female 6 -1.59 p.Lys392Arg (c.1175A>G) Female 15 -5.81 -6.63 Delayed puberty p.Asn646Lys (c.1938C>G) Male 6 -2.70 p.Asn646Lys (c.1938C>G) Male 3 -1.59 -1.47 -2.05 0 40.3 RU (<5.36) 0.08 (<0.43) Not tested 3224 RU(<1.56) 3 5 (<34) 0(<5) 11(<60) Not tested insulin treated Negative 43 31.9 U/mL (<1.0) 9.5 U/mL (<5) Not tested Not tested insulin treated Not tested Not diabetic Negative Negative Not tested Negative Fecal elastase 166mg/ g faeces (>200) On enzyme replacement therapyLow Fecal elastase NO NO NO High Risk DRB1*03 -DQB1*02/ DRB1*03 -DQB1*02 High Risk DRB1*04 DQB1*0302 Low Risk DQA1*01DQB1*05/ DQA1*01DQB1*0602 Low Risk DQA1*03B1*03:02/A1*01B1*06:02 Low risk 1.8 1.5 0.76 0.8 N/A 61 70 68 69 Not tested Coeliac disease Coeliac-disease NO NO Autoimmune enteropathy 17 months <12 months N/A N/A <12 months High Risk DR52-DR3-DQ2 High risk DQ8 Not tested Not tested Low risk TtG IgA 20.47 U/mL (<10) TtG IgG > 200 U/mL (<10) Not tested <1.0 (<10) 2.8 (<7) Not tested Not tested Positive Endomysial & gliadin autoantibodies Not tested Not tested Positive for gliadin autoantibodies YES YES N/A N/A NO NO Mild atopic YES YES Non-specific dematitis None Desquamative interstitial pneumonitis None None Asthma Recurrent URTI Growth (Height SDS) -2.33 DIABETES insulin doses HbA1c Age at Diagnosis (Wks) 2 GAD65 autoantibodies 35 RU (<34) I-A2 autoantibodies 0 (<5) ZnTn8 autoantibodies 7 (<60) Not tested insulin IAA autoantibodies treated ICA Negative Pancreatic Exocrine Insufficiency T1D HLA Type† Current Insulin dose (U/Kg/day) Current HbA1c (mmols/mol) ENTEROPATHY Type Onset of symptoms (months) Coeliac HLA type Anti TtG autoantibodies Endomysial/gliadin autoantibodies Responsive to gluten free diet OTHER AUTOIMMUNE FEATURES Eczema Pulmonary manifestations Primary hypothyroidism (TPO Other features antibodies 224 U/mL (<20). Lipoatrophy at sites of insulin injection HEMATOLOGICAL FEATURES NO 28 JDFU(<2.5) p.Lys658Asn (c.1974G>C) Female 17 -1 -4.00 Delayed puberty Negative None None Juvenile arthritis, severe dry eyes Progressive macular edema & vision loss. Kawasaki diseaselike episodes T-cell LGL leukemia. Hb 10.0g/dl nd NO Lymphadenopathy Autoimmune cytopenias. MCV 64.7fl (73-89) MCH 20.4pg (2430) & splenomegaly. Autoimmune cytopenias NO Dentures NO NO <2.0 (<100kU/L) - 1.3% (<6%) - <2.0 (<100kU/L) 0.30 x109 /L (<0.7x109/L) <2.0 (<100kU/L) 0.28 x109 /L (0.08-1.1x109/L) DENTAL ANOMALIES Delayed eruption of primary teeth IMMUNODEFICIENCY Ig E Eaosinophils Infection susceptibility 0.7 (3.9-10) - Recurrent bacterial Recurrent LRTI, IVIG from 12 NO NO bacterial URTI, y/o IVIG from 12 y/o Table: TPO = Thyroid Peroxidase, TtG = Anti-Tissue trans glutaminase antibody, URTI=Upper Respiratory Tract Infections, LRTI=Lower Respiratory Tract Infections, IVIG = Intravenous Immunoglobulin Replacement Therapy. N/A = not applicable. Normal ranges are provided in parenthesis when appropriate. * Patient previously reported in 3. †HLA typing was undertaken on patients 1-4 using previously described methods4. NO Supplementary Table 6: Adapted from Gambineri and Torgerson (2012)6 using additional published literature. Approximate % of patients affected with a condition are shown in brackets. Abbreviations APS1 (autoimmune polyendocrinopathy syndrome type I) IPEX (X-linked immunodysregulation, polyendocrinopathy, and enteropathy) Disorder Gene Inheritance Number of patients reported References STAT3 polyautoimmunity STAT3 Dominant 5 patients (5 families) This paper Common clinical features (present in >50% of patients Type 1 diabetes (80%) Enteropathy (60%) Short stature (100%) Additional clinical features Autoimmunoe thyroid (40%) Juvenile Chromic Arthritis (20%) Fibrotic lung disease (20%) Other laboratory or diagnostic features Normal eosinophil count Low-normal IgE APS1 IPEX CD25 deficiency ITCH deficiency AIRE Recessive >150 FOXP3 Recessive >70 IL2RA Recessive 4 patients (4 families) ITCH Recessive 10 patients (1 family) Peterson, & Peltonen (2005)7 d'Hennezel, et al (2012) 8 Wildin et al(2002)9 Enteropathy (100%) Eczematous Dermatitis (70%) Type 1 diabetes (67%) Bezrodnik, et al (2013)10 Lohr et al. (2010)11 Enteropathy (100%) Recurrent persistent viral infection(100%) Eczema (75%) Developmental delay (100%) Macrocephaly(90%) Dysmorphic facies (90%) Chronic lung disease (90%) Hepatosplenomegaly (90%) Hypothyroidism (50%) Type 1 diabetes (25%) Alopecia Universalis (50%) Lympthadenoptathy (50%) Hypothyroidism (40%) Autoimmune Hepatitis (30%) Enteropathy (20%) Type 1 diabetes (10%) Hypoparathyroidism (80%) Adrenal insufficiency (88%) Mucocutaneous candidiasis (86%) Gonadal insufficiency (45%) Type 1 Diabetes (13%) Pernicious anaemia (13%) Alopecia areata (45%) Vitiligo (15%) Autoimmune hepatitis (15%) Keratitis (28%) Antibodies to type I interferons (IFN-α or ω) Autoimmune thyroid(35%) Autoimmune haemolytic anaemia (32%), Thrombocytopenia (15%), Lympthadenopathy (8%) Eosinophilia Very elevated IgE FOXP3 expression in CD4+ T Cells low IgE typically normal CD25 expression on T cells absent or low (flow cytometry) Supplementary Figure 1 Western blot showing the expression of STAT3 protein in HEK-293 cells transfected with STAT3 contructs. HEK293 cells were lysed and protein extracts probed with anti-STAT3 antibody. β-actin was used as a loading control. The experiment was repeated twice with similar results. Supplementary Figure 2 Genotype-phenotype relationship in STAT3 mutations. The predicted effects of STAT3 mutations were modelled in PDB structure 1bg1 (mouse STAT3/DNA complex) using SWISS-MODEL, and visualized in SwissPdbViewer. a) Overview of STAT3 dimer bound to DNA; STAT3 chains are shown in ribbon form, with residues N646 (red) and N647 (green) shown as space-filling on the left chain only; DNA strands are shown as blue and turquoise ribbons. b) as a), but expanded to show the proximity of residues N646 and N647 to both the DNAbinding and dimerization surfaces. c) Predicted molecular surfaces of wild-type STAT3 (wt), and mutants N646K, N647D and N647I; surfaces are coloured for positive charge (blue; top row), negative charge (red; middle row) and hydrophobicity (brown, most polar to blue, most hydrophobic; bottom row); structures have been rotated compared to a) and b) to show relevant groups more clearly. The N646K mutation reported here results in increased positive charge (circled, N646K column, upper row) at the DNA binding surface; this is likely to result in higher DNA binding affinity due to electrostatic interaction with the DNA backbone, and hence increased STAT3 activity. Conversely, the N647D mutation, previously reported as a loss-of function mutation in HIES, leads to increased negative surface charge in this region (circled, N647D column, middle row) and is likely to inhibit DNA binding and/or dimerization. By comparison, a different mutation at this position, N647I, has been previously reported as an activating mutation in LGLL; it has been postulated that STAT3 mutations in LGLL promote STAT3 dimerization, and hence biological activity, as a result of increased hydrophobicity at the dimerization surface. This is consistent with protein modelling in silico which predicts increased hydrophobicity in this region (circled, N646I column, bottom row) compared to wild-type STAT3 or other variants. References 1 2 3 4 5 6 7 8 9 10 11 Lango Allen, H. et al. Nature genetics 44, 20-22, (2012). Ellard, S. et al. Diabetologia 56, 1958-1963,(2013). Otonkoski, T. et al. Diabetologia 43, 1235-1238,(2000). Sjoroos, M. et al BioTechniques 18, 870-877 (1995). Russell MA et al. Islets 5, 95-105 (2013) Gambineri, E. & Torgerson, T. R. et al CMLS 69, 49-58, (2012). Peterson, P. & Peltonen, L.. Journal of autoimmunity 25 Suppl, 49-55,(2005). d'Hennezel, E. et al Journal of medical genetics 49, 291-302, (2012). Wildin, R. S. et al Journal of medical genetics 39, 537-545 (2002). Bezrodnik, L. et al Clinical and experimental immunology (2013). Lohr, N. J. et al. American journal of human genetics 86, 447-453 (2010).