ю ° T Р яяяяяяяя Й) 8. . . " 8. 8. 8. PА а=Р/ Р Р
advertisement

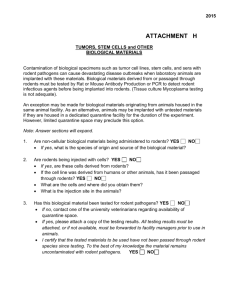
COMMUNICABLE DISEASE MANUAL POLICIES / PROCEDURES HANTAVIRUS PULMONARY SYNDROME (HPS) OBJECTIVE: Control and management of Hantavirus Pulmonary Syndrome. DESCRIPTION: An acute zoonotic viral disease characterized by fever, myalgias and GI complaints followed by the abrupt onset of respiratory distress and hypotension. The illness progresses rapidly to severe respiratory failure and shock. An elevated hematocrit, hypoalbuminemia and thrombocytopenia are found in most cases. The crude mortality rate is approximately 40%-50%; it was 43% of the first 217 cases identified. In survivors, the recovery from acute illness is rapid, but full convalescence may require weeks to months. Restoration of normal lung function generally occurs, but pulmonary function abnormalities may persist in some individuals. Renal and hemorrhagic manifestations are usually absent except in some severe cases. Multiple hantaviruses have been identified in the Americas: Sin Nombre virus is the agent responsible for the 1993 epidemic in southwest USA and most of the other cases identified in North America. Other strains associated with human disease include Black Creek Canal and Bayou viruses (southeastern USA), New York-1 and Monongahela viruses (eastern USA), Andes virus (Argentina, Chile), Laguna Negra virus (Paraguay, Bolivia) and Juquitiba virus (Brazil). Rodents, the natural hosts for the hantaviruses, acquire a lifelong, asymptomatic, chronic infection with prolonged viruria and virus in saliva. Humans acquire infection through direct contact with infected rodents, rodent droppings, nests, inhalation of aerosolized virus particles from rodent urine, droppings, or saliva. Rarely, infection may be acquired from rodent bites or contamination of broken skin with excreta. Person-to-person transmission of the viruses in the United States has not been demonstrated, but a few cases of person-to-person spread of Andes virus have been reported from Patagonia, South America. At-risk activities include handling or trapping rodents, cleaning or entering closed, rarely used rodent-infested structures, cleaning feed storage or animal shelter areas, hand plowing, and living in a home with an increased density of mice in or around the home. For backpackers or campers, sleeping in a structure also inhabited by rodents has been associated with HPS. Weather conditions resulting in exceptionally heavy rainfall and improved rodent food supplies can result in a large increase in the rodent population. The increased rodent population results in more frequent contact between humans and infected mice and may account for recently recognized outbreaks. Most cases occur during spring and summer, and the geographic location is determined by the habitat of the rodent carrier. Protection and immunity conferred by previous infection in unknown. Sin Nombre virus is transmitted by the deer mouse, Peromyscus maniculatus; Black Creek Canal virus is transmitted by the cotton rat, Sigmodon hispidus; Bayou virus is transmitted by the rice rat, Oryzomys palustris; and New York virus is transmitted by the whitefooted mouse, Peromyscus leucopus. The incubation period may be 1 to 6 weeks after exposure to infected rodents, their saliva, or excreta but has not been established definitely. D:\106739853.docPage 1 of 4 EQUIPMENT: MDSS User Manual and the MDSS Communicable Disease Case Form. MDCH website at www.michigan.gov/cdinfo and CDC website at www.cdc.gov/diseasesconditions/az/a.html. POLICY: Legal Responsibility: Michigan's communicable disease rules of Act No. 368 of the Public Acts of 1978, as amended, being 333.5111 of the Michigan Compiled Laws. Follow-up time within 24 hours post referral AND ENTER INTO MDSS WITHIN 24 HOURS OF RECEIPT OF REFERRAL. PROCEDURE: A. B. Case Investigation 1. Referral received per phone call, laboratory results, or automatically through MDSS. 2. Document all case investigation proceedings. 3. Contact MD and/or client to start process of completing disease specific form in MDSS. Case Definition 1. Clinical Case Definition: An illness characterized by one or more of the following clinical features: A febrile illness (i.e., temperature > 101.0º F [>38.3º C]) characterized by bilateral diffuse interstitial edema that may radiographically resemble ARDS, with respiratory compromise requiring supplemental oxygen, developing within 72 hours of hospitalization, and occurring in a previously healthy person. 2. Case Classification: C. D:\106739853.docPage 2 of 4 An unexplained respiratory illness resulting in death, with an autopsy examination demonstrating noncardiogenic pulmonary edema without an identifiable cause. Confirmed: confirmed. A clinically compatible case that is laboratory Lab Criteria for Diagnosis 1. Detection of hantavirus-specific IgM antibodies by using Elisa, Western blot or strip immunoblot techniques or rising titers of hantavirus-specific IgG antibodies, or 2. Detection of hantavirus-specific ribonucleic acid sequence by polymerase chain reaction in clinical specimens, or 3. Detection of hantavirus antigen by immunohistochemistry. 4. Laboratory testing should be performed or confirmed at a reference laboratory. Because the clinical illness is nonspecific and Acute Respiratory Distress Syndrome (ARDS) is common, a screening case definition can be used to determine which patients to test. In general, a predisposing medical condition (e.g., chronic pulmonary disease, malignancy, trauma, burn, and surgery) is a more like cause of ARDS than HPS, and patients who have these underlying conditions and ARDS need not be tested for hantavirus. D. E. D:\106739853.docPage 3 of 4 Control Measures 1. Hantavirus infections of humans occur primarily in adults and are associated with domestic, occupational, or leisure activities bringing humans into contact with infected rodents, usually in a rural setting. Eradicating the host reservoir is not feasible. The best currently available approach for disease control and prevention is risk reduction through environmental hygiene practices that discourage rodents from colonizing the home and work environment and that minimize aerosolization and contact with virus in saliva and excreta. Hantaviruses, because of their lipid envelope, are susceptible to most disinfectants, including diluted bleach solutions, detergents, and most general household disinfectants. 2. Measures to decrease exposure in the home and workplace include eliminating food sources available to rodents in structures used by humans, limiting possible nesting sites, sealing holes and other possible entrances for rodents, and using "snap traps" and rodenticides. Other methods include using a 10% bleach solution to disinfect dead rodents and wearing rubber gloves before handling trapped or dead rodents. Gloves and traps should be disinfected after use. Before entering areas with potential rodent infestations, doors and windows should be opened to ventilate the enclosure. People entering these areas should avoid stirring up or breathing potentially contaminated dust. Dusty or dirty areas or articles should be moistened with a 10% bleach or other disinfectant solution before being cleaned. Brooms and vacuum cleaners should not be used to clean rodent-infested areas. 3. Efficacious chemoprophylaxis measures or vaccines are not available. HPS has not been associated with nosocomial or person-to-person transmission in the USA and does not need isolation or quarantine measures for patient or contacts. MDSS Case Report 1. Complete case investigation using disease specific form in MDSS. 2. Notify CD Supervisor that the case report is ready for review. PHN will be notified if corrections are needed prior to closing case in MDSS. 3. CD Supervisor reviews case for completeness and closes MDSS case report. RESOURCES: D:\106739853.docPage 4 of 4 Current Red Book Current Control of Communicable Diseases Manual Current disease specific “Fact Sheet” Websites: www.cdc.gov/diseasesconditions/az/a.html www.michigan.gov/cdinfo MMWR, Volume 46, 1997