Full methodology of the pediatric pilot randomized trial on
advertisement

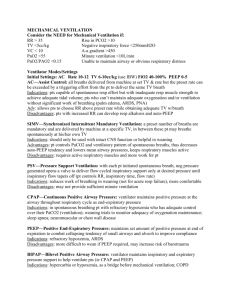
Full materials and methods of the pediatric pilot randomized trial on mechanical ventilation weaning with a computerized protocol versus usual care Patients Eligible patients were children between 2 and 18 years with body weight (BW) ≥ 15 kg admitted to the pediatric intensive care unit (PICU) of Sainte-Justine Hospital for any reason, except cardiac surgery, between September 2007 and June 2009, for whom mechanical ventilation for at least 12 hours was expected. Children were included if the Evita XL respirator with SmartCare/PS™ was available and if they fulfilled the following weaning criteria during the screening periods (Monday to Friday mornings): patient able to breath spontaneously, no vasopressor or inotrope medication (other than digoxin or low dose dopamine (< 5 µg/kg/min)), FiO2 ≤ 60% with oxygen saturation ≥ 95%, positive end expiratory pressure (PEEP) ≤ 8 cmH2O, plateau pressure ≤ 25 cmH2O, PaCO2 < 70 mmHg on most recent blood gas, endotracheal tube leak ≤ 20%. Patients were excluded if: they had severe chronic respiratory insufficiency due to neurological, neuromuscular or lung diseases prior to PICU admission, primary pulmonary hypertension or cyanotic congenital heart disease. Children expected to be extubated on the day of inclusion, not expected to survive, with a decision to withdraw care or with no parental consent were also excluded. The study protocol was approved by the institutional review board of Sainte-Justine Hospital. Pilot trial design This was a single centre, pilot randomized study. After inclusion, a pressure support (PS) test was performed (ventilation in PS mode at a level of ± 5 cmH2O of the pre-inclusion plateau pressure). The test was considered positive when, after 30 minutes, the patient remained with a respiratory rate (RR) between 10 and 40 breaths per minute (bpm), an expiratory tidal volume (Vt) ≥ 6 ml/kg and a SpO2 ≥ 95% with FiO2 ≤ 60%. The test was stopped before 30 minutes if the patient showed evidence of respiratory distress (RR > 40 bpm or FiO2 > 60% with SpO2 ≥ 95%). The test was repeated daily until positive. When the PS test was positive, the patient was ventilated with an Evita XL respirator in PS mode and was allocated randomly to wean via SmartCare/PS™ (SmartCare group) or usual methods through a sequential opaque envelope technique. In the usual care group, physicians were instructed to wean according to their practice, in the absence of formal guidelines in the PICU, including modification of ventilation mode if required. In the SmartCare group, the SmartCare/PS™ option of the Evita XL was switched on after adjusting for BW. SmartCare/PS™ is an explicit computerized protocol that manages the weaning phase with modification of pressure support level in closed loop. Its functioning for children has already been described in a previous study (17). In addition, PEEP was adjusted using a written protocol including the following two guidelines: (1) decrease of PEEP level by 1 cmH2O per 8 hours to a minimum of 5 cmH2O, if FiO2 ≤ 50% with SpO2 ≥ 95%; (2) if FiO2 ≥ 60% to maintain a SpO2 ≥ 95% during 1 hour, the attending physician could decide if an increase in PEEP was necessary. If the patient required heavy sedation, or if his clinical status deteriorated, with a RR ≥ 40 bpm, clinical discomfort, and/or hypoxemia (need for FiO2 ≥ 60% and need for PEEP ≥ 8 cmH2O with SpO2 ≥ 95%), or PS level reached the upper limit of 27 cmH2O, ventilation was switched back to assist control ventilation. The patient was then retested with PS test daily and SmartCare/PS™ was restarted when the test was positive. The decision to extubate was made by the attending clinicians in both groups. In the SmartCare group, if the extubation was performed later than 30min after a ‘‘separation recommendation’’ from SmartCare/PS™, this was considered to be a delayed extubation. The reason for this delay was collected prospectively. In accordance with current mechanical ventilation practice in this pediatric intensive care unit, no recommendation of separation from the respirator was provided by the SmartCare/PS™ between 8:00 pm and 6:00 am. The primary endpoint studied was the time from randomization to the first extubation. Secondary endpoints included: (1) weaning failure: resuming mechanical ventilation (non invasive or invasive) within 48 hours after extubation or failure to wean within 28 days of randomization. Non-invasive ventilation was considered as weaning failure if used more than 12 hours a day. Causes of failure were documented (lower respiratory tract problems, upper airway obstruction, apnea, cardiovascular insufficiency, others); (2) total duration of mechanical ventilation: duration of ventilatory support from first intubation until extubation. If a patient was reintubated within 48 hours after extubation, both mechanical ventilation episodes were considered as the same episode; (3) length of PICU stay; (4) length of hospital stay; (5) Ventilator free days at 28 days: number of days between successful weaning from invasive mechanical ventilation and day 28 after study enrollment. Power & sample size calculations This pilot study included 30 patients (15 in each group), which corresponded to 10% of the sample size that we expect to include in a multicentrer randomized clinical trial that we plan to conduct after this pilot study. Our preliminary study had suggested a 20% difference in length of weaning between usual care vs SmartCare/PS™ (17). A study led by A. Randolph et al. (13) reported that the duration of weaning was 3.22.5 days in a similar population. A 20% reduction of this period would have resulted in a difference of 0.70.5 days. Therefore, to detect a statistically significant difference in the length of weaning at 90% power and at a 2-sided alpha=0.05 using the “Paired t-test for sample size calculations” and considering 5 PICUs with 3 stratification levels (ie acute lung injury, surgical procedure, others) and an attrition rate of 10%, the calculated sample size for the multicenter randomized clinical trial was 296 patients. Data analysis Analysis was done using the intention to treat principle. As the primary outcome did not have a normal distribution, a non-parametric statistical test was used (Mann-Whitney U test) to assess for statistical significance. Levels of statistical significance were set at P<0.05. Statistical analysis was performed with SPSS software, version 13.0. The probability of remaining on mechanical ventilation was analyzed by the Kaplan-Meier method, and a log-rank test was used to assess differences. Cox proportional hazards modelling was performed to estimate the adjusted effect of selected variables (close to statistical significance at baseline between the two groups) on the primary end point.