AAO Symposia 2007 - Co-Sponsor - The Ocular Microbiology and
advertisement

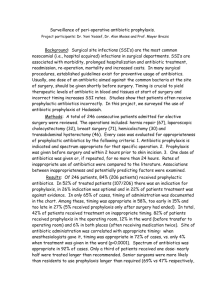
1 Figure 1. Questions of Prophylaxis Usage in Ophthalmic Practice Question 0 –What area of surgery is your primary expertise? A) Comprehensive, B) Cataract, C) Refractive, D) Retina, E) Cornea, F) Glaucoma Question #1 – What is your personal opinion of using antibiotics for surgical prophylaxis? (Don’t consider Povidone Iodine as an antibiotic) A) Antibiotics are unnecessary for surgical prophylaxis. B) Antibiotics are unnecessary but I’m not taking any CHANCES! C) It is malpractice not to use antibiotics. D) Antibiotics should only be used for select cases. Question #2 – What measure do you believe is best to avoid post-operative infection? A) Povidone Iodine, B) Topical Antibiotics, C) Consistent Surgical Preparation (lid cleansing, draping, etc), D) A dedicated ocular operating area Question #3 – What is your current regimen for antibiotic prophylaxis during surgery? A) I don’t use antibiotics for prophylaxis., B) Before surgery only, C) After surgery only D) Before and After Surgery Question #4 – What statement describes your opinion regarding the literature and its support of surgical antibiotic prophylaxis? A) The literature supports surgical antibiotic prophylaxis. B) The literature does not support surgical antibiotic prophylaxis. C) The literature is pharmaceutical driven to support antibiotic prophylaxis. D) I base my use of antibiotics for prophylaxis on my residency training. Question #5 – Besides topical application, what other method of antibiotic application do you use for prophylaxis? A) Topical ONLY, B) Antibiotics in the Infusion Fluid, C) Intracameral Injection after surgery (ESCRS study), D) Subconjunctival Injection, E) I don’t use antibiotics for prophylaxis Question #6 – What is your opinion on the use of Vancomycin for surgical prophylaxis? A) Never use Vancomycin. It will increase the chance of vanomycin-resistant bacteria! B) My patients deserve the best so I use Vancomycin. C) Only for patients that have or are a risk for MRSA. D) There are better antibiotic alternatives than Vancomycin. Question #7 – What Fluoroquinolone do you use for surgical prophylaxis? A) I don’t use antibiotics for surgical prophylaxis!, B) Vigamox (moxifloxacin) or Zymar (gatifloxacin), C) Levofloxacin, D) Ofloxacin or Ciprofloxacin, E) I use other antibiotics. Question #8 – What convinced you to switch to Vigamox (Moxifloxacin) or Zymar (gatifloxacin) for surgical prophylaxis? A) I didn’t switch, B) Literature, C) Drug Rep, D) A National Meeting Symposium (AAO, RHE, etc), E) Residency Training 2 Question #9 – What is your opinion on the future of effective antibiotics in Ophthalmology? A) There will always be something new. B) We are in trouble because there is nothing in the pipeline! C) We can use older antibiotics (i.e. gentamicin, cefazolin) to meet our needs. D) Wise use of current antibiotics will circumvent any future problems. Question #10 – What is your favorite antibiotic for surgical prophylaxis? A) I don’t use antibiotics for surgical prophylaxis!, B) Aminoglycoside (gentamicin or tobramycin), C) Polytrim, D) Fluoroquinolone, E) Other Question #11 – What was the main reason that you switched from an older antibiotic to a fluoroquinolone? A) Broad-spectrum coverage, B) Better tissue penetration, C) Less toxicity, D) Convincing drug rep (dinner, golf, etc), E) Better potency (lower MICs), F) I didn’t switch! Question #12 – What would convince you to start using an older antibiotic (gentamicin, polytrim, etc) for surgical prophylaxis? A) Same coverage, lower cost, B) I would not use older antibiotics because newer is better. C) The less chance of antibiotic resistance, D) Literature endorsement – Evidence based practice Question #13 – What is your first-line antibiotic for refractive surgical prophylaxis? A) I don’t use antibiotics B) Zymar (gatifloxacin) or Vigamox (moxifloxacin) C) Levofloxacin D) Ciprofloxacin or Ofloxacin E) Other Question #14 – What do you consider the most likely source for post-surgical refractive infection? A) Eyelids, B) Contaminated instruments, C) Patient Non-Compliance (eye rubbing, etc) D) Poor Surgical Technique Question #15 – What infectious agent do you fear most for post-operative refractive infection? A) Mycobacteria, B) Gram-negatives (Pseudomonas aeruginosa), C) Streptococci/Enterococcus D) Staphylococcus aureus, E) Fungus Question #16 – I treat suspected adenovirus conjunctivitis with antibiotics because: A) I am not sure it is an adenovirus infection, it may be bacterial. B) I have to give the patient something! C) I am worried of corneal superinfection. D) I don’t treat suspected adenovirus infections with antibiotics. Question #17 - If I had a laboratory confirmed adenovirus conjunctivitis, the treatment would be: A) No treatment, B) Antibiotics to prevent super infection, C) Steroids, D) Treat Symptoms (dilators, artificial tears, astringents, etc), E) Antiviral (if ever available) 3 Question # 18 – My first-line antibiotic for treating infectious conjunctivitis is: A) sulfacetamide, B) polytrim (polymyxin B/trimethoprim), C) aminoglycosides D) fluoroquinolones, E) other (erythromycin, bacitracin, chloramphenicol, etc) Question #19 – A patient has a large central ulcer that is not responding to antibiotics and all laboratory tests including confocal microscopy are negative. Fungal infection is still part of the differential. What would your first clinical initiative be? A) More laboratory testing to rule out fungal infection. B) Put the patient on a course of antifungal therapy, C) Steroids and keratoplasty, D) A and B, E) Refer patient Question # 20 – What would your first-line antifungal agent be to treat fungal keratitis? A) topical amphotericin B, B) topical Natamycin ,C) topical voriconazole, D) oral ketaconazole E) other Question #21 – If a contact lens wearer presented with a corneal infiltrate and used contact lens solutions that were implicated in the recent fungal keratitis epidemic, your first clinical initiative would be: A) Laboratory work-up (including contact case and solution), empiric antibiotics B) Empiric antibacterial therapy only C) Empiric antibacterial and antifungal therapy D) Remove and discard contacts, no anti-infective therapy, watch patient