ADHESION MOLECULES from NEJM 6/6/96
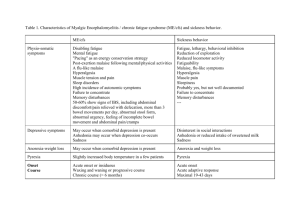
advertisement

University of Colorado Denver – School of Medicine Disease and Defense Course IDTP5004A Instructor: Francisco G. La Rosa, MD, Associate Professor February 5th, 2010 ACUTE AND CHRONIC INFLAMMATION Recommended Reading: Chapter 2 - "Acute and Chronic Inflammation", in Kumar, Robbins and Cotran: Pathologic Basis of Disease, 8th ed. WB Saunders Co. This is also available free online at: http://www.mdconsult.com/das/book/body/94286448-2/0/1249/0.html Learning Objectives: 1. List and describe the 5 clinical signs of acute inflammation and give their clinicalpathogenetic basis. 2. Describe the 3 major pathogenetic mechanisms of acute inflammation. Summarize the role of the endothelial cell. 3. List and describe the sequence of events involving a neutrophilic response in acute inflammation due to a pyogenic microorganism, e.g. Staphylococcus aureus. 4. Discuss leukocyte and endothelial cell adhesion molecules and cite an example of each. 5. Define chemotaxis and list the 3 major examples. 6. Define opsonin and list the 2 major types. 7. Describe the process by which a neutrophil engulfs and destroys a pyogenic microorganism. 8. Define and compare transudate and exudate. List and describe the different types of exudate citing etiologic agents for each type. 9. Define and compare abscess and cellulitis. 10. Define chronic inflammation and compare it to acute inflammation. Give examples of etiologic agents of chronic inflammation. 11. Indicate the features and differential diagnosis of granuloma. Discuss its pathogenesis. 12. Define and compare ulcer and erosion. 13. Define and compare fistula and sinus tract. 14. Describe the pathogenetic, pathologic and clinical features of leukocyte adhesion deficiency, type I; chronic granulomatous disease of infancy, and Chediak-Higashi disease. 15. Define and indicate the major features of the systemic inflammatory response syndrome and the acute phase reaction. 16. Describe sarcoidosis. Disease & Defense Block I. “Acute and Chronic Inflammation” Page 2 ACUTE INFLAMMATION A. CLINICAL FEATURES: Celsus, a Roman writer of the first century AD, first listed the four cardinal signs of inflammation: 1. Rubor (Redness) 2. Calor (Warmth) 3. Tumor (Swelling) 4. Dolor (Pain) 5. Functio laesa (Loss of function) (later added by Virchow). B. PATHOGENESIS: Three main processes occur at the site of inflammation, due to the release of chemical mediators: 1. Increased blood flow. Brief initial vasoconstriction (pallor) is followed by vasodilatation of arterioles and capillaries (redness and warmth). 2. Increased vascular permeability. Loss of intravascular fluid and other blood components results in stasis of blood flow and the accumulation of fluid (exudate) in the interstitial tissues and/or body cavities. These account for swelling, pain and loss of function. Note: Edema and/or effusion can be an exudate (due to an inflammatory process) or a transudate (due to a non-inflammatory process). The pathogenesis of transudate will be discussed in the sessions on hemodynamic disease processes. In the meantime, this table summarizes the differences: Etiology Specific gravity (g/mL) Total protein (g/dL) Fluid/serum protein ratio Fluid/serum LDH ratio Fluid/serum glucose ratio Cells (leukocytes) TRANSUDATE Increased hydrostatic pressure <1.015 <3.0 <0.5 <0.6 >1.0 No EXUDATE Iinflammation >1.015 >3.0 >0.5 >0.6 <1.0 Yes Types of exudate vary with etiologic agent and site and degree of injury. The various types of exudate will be discussed below. 3. Leukocytes accumulate at the site of injury in some types of inflammation. Neutrophils are the predominant cell in and are characteristic of acute inflammation. The sequence of events are as follows: a. Margination (rolling). With loss of fluid and stasis circulating neutrophils accumulate along the endothelial surface of capillaries and venules. b. Adhesion. Neutrophils adhere to the endothelial surface. This involves specific interaction between 1) adhesion molecules on the surface of the neutrophil. e.g. LFA-1 (CD11/CD18 integrins) 2) Adhesion molecules on neutrophils are enhanced by C5a 3) adhesion molecules on the surface of the endothelial cell e.g ICAM-1 (immunoglobulin family) 4) Adhesion molecules on endothelial cells are enhanced by IL-1 and TNF Disease & Defense Block “Acute and Chronic Inflammation” Page 3 The interaction between LFA-1 and ICAM-1 is frequently used as an example of adhesion molecule interaction. For a full listing of such interactions (optional) see Kumar, et al p. 38 c. Migration and chemotaxis. Adhered neutrophils next move between endothelial cells to the site of injury. This is directed emigration and occurs in response to chemotactic agents released at the site of injury. The chemotactic response is unidirectional and in response to a chemical gradient. The major chemotactic agents for neutrophils are 1) 2) 3) 4) Bacterial products Complement derivatives, e.g. C5a Arachidonic acid derivates, e.g. leukotriene B4 (LTB4) Cytokines – especially chemokines d. Phagocytosis. If the injury is due to foreign particles (e.g. bacteria) the particles are recognized by the neutrophil surface and adhere to it. Non-specific coating of such particles by opsonins facilitates their phagocytosis. Opsonins include IgG and C3b in blood. The foreign particle is enclosed by the cell membrane and ingested as a membrane-bound structure, the phagosome. The bacterium is killed and lysed by: 1) Oxygen-dependent system. The ultimate step in the elimination of infectious agents and necrotic cells is their killing and degradation within neutrophils and macrophages, which occur most efficiently after activation of the phagocytes. Microbial killing is accomplished largely by oxygen-dependent mechanisms. Phagocytosis stimulates a burst in oxygen consumption, glycogenolysis, increased glucose oxidation via the hexose-monophosphate shunt, and production of reactive oxygen intermediates (ROIs, also called reactive oxygen sepecies). The generation of reactive oxygen intermediates is due to the rapid activation of an oxidase (NADPH oxidase), which oxidizes NADPH (reduced nicotinamide-adenine dinucleotide phosphate) and, in the process, reduces oxygen to superoxide anion ( ). Superoxide is then converted into hydrogen peroxide (H2O2), mostly by spontaneous dismutation. Hydrogen peroxide can also be further reduced to the highly reactive hydroxyl radical (OH). Most of the H2O2 is eventually broken down by catalase into H2O and O2, and some is destroyed by the action of glutathione oxidase. 2) Oxygen-independent systems. These include lysozyme, lactoferrin and major basic protein. Major basic protein is especially important in eosinophilic toxicity to parasites. 3) Lysosomes. Phagosomes merge with neutrophilic lysomes to form phagolysosomes, allowing activated enzymes to biodegrade the bacteria. C. TYPES OF ACUTE INFLAMMATION. These are defined by the type of exudate which, in turn, is determined by the etiologic agent, the site of injury and the severity of injury. 1. Serous Contains low MW proteins, especially albumin. Clear yellow fluid. No cells. Examples: Blister in a second degree burn; Laryngeal edema in an acute anaphylactic reaction to penicillin. Disease & Defense Block “Acute and Chronic Inflammation” Page 4 2. Fibrinous Contains larger proteins, especially fibrin. Note: Make sure you distinguish between the terms “fibrinous” and “fibrous”. Often coats a surface. No cells. Examples: Fibrinous pneumonia (pneumonitis) in chlorine gas inhalation or viral infection, e.g. influenza. Fibrinous pericarditis in rheumatic carditis. 3. Purulent (Suppurative) In addition to albumin, fibrin and other proteins, the exudate contains neutrophils. A exudate composed of fluid, protein, and dead/dying neutrophils and other cells is pus. Pyo- is the prefix which refers to pus. Examples: Suppurative pneumonia or meningitis due to a pyogenic microorganism, e.g. Neisseria meningitidis. Pyosalpinx – purulent infection of the fallopian tube e.g. due to Neisseria gonorrhoeae. 4. Eosinophilic The eosinophil is prominent or predominant in this type of exudate. It characteristically occurs in Type I hypersensitivity (allergic) reactions and certain parasitic infections. Examples: Asthma, allergic rhinitis; Nematode infection, ascariasis of small intestine. 5. Hemorrhagic Damage to endothelial cells and vessel walls allow RBCs to leak into the surrounding tissue. Rickettsia are especially prone to damaged endothelial cells. Example: Rocky Mountain Spotted Fever. 6. Mucinous Inflammation in tissue containing abundant mucin-secreting glands is likely to stimulate secretion mucus. Example: Bronchitis. 7. Pseudomembranous The injury results in necrosis of the affected tissue lining a surface. This results in the formation of a “membrane” composed of fluid, proteins, neutrophils, RBCs and necrotic tissue. Example: Pseudomembrane obstructing the upper airway in diphtheria (Corynebacterium diphtheriae); Pseudomembranous enterocolitis in patients treated with clindomycin and develop intestinal infection due to Clostridium dificile. * Many exudates are combined, e.g. fibrinopurulent or mucopurulent. D. SPECIFIC TYPES 1. Abscess A focus of acute inflammation composed of pyogenic exudate and necrotic tissue. Certain bacteria are especially likely to result in an abscess, e.g. Staphylococcus aureus and Klebsiella pneumoniae. Although generally designated as “acute” an abscess may be present for a long time. They may occur anywhere in the body and, in some locations, may be present for a long time before diagnosis. They may eventually become “walled off” by a fibrous connective tissue. They may be large or microscopic and single or multiple. They may rupture into a hollow structure (e.g. a ventricle in the brain) or drain (e.g. into a bronchus or the surface of the skin. Furuncle (“boil”) – a subcutaneous abscess, usually arising in or near a hair follicle. S. aureus is a common cause. Carbuncle – coalesced furuncles. 2. Cellulitis A diffuse area of acute inflammation composed of edema fluid, bacteria and neutrophils spread through tissue. Clinically characterized by a diffuse area of swelling, redness, warmth and pain. Certain bacteria are especially likely to result in cellulitis, e.g. Streptococcus pyogenes. Typically occurs in skin and subcutaneous tissues. Usually necrosis is not present but, in certain instances, it may be a prominent feature, e.g. socalled flesh-eating infections. Disease & Defense Block “Acute and Chronic Inflammation” Page 5 3. Lymphangitis. Pyogenic infections may spread proximally via lymphatics; this may be recognized clinically as red lines seen in the skin. Secondary involvement of draining lymph nodes may result in acute lymphadenitis. The nodes are enlarged, soft (fluctuent) and tender. II. CHRONIC INFLAMMATION In comparison with acute inflammation, chronic inflammation tends to be: Gradual in onset Of relatively lower intensity Longer lasting The characteristic inflammatory cells are mononuclear cells, especially lymphocytes and/or macrophages. Eosinophils and/or plasma cells may be present. A. MACROPHAGES are derived mainly from monocytes in the circulating blood. They are distinguished from “fixed macrophages” such as Kuppfer cells in the liver. Macrophages are active in phagocytosis and produce a wide variety of biologically active products. Fusion of macrophages results in giant cells (Langhans cells). Tissue destruction is a hallmark of chronic inflammation. Chronic inflammation may evolve from previous acute inflammation, but most often, it occurs de novo in response to certain etiologic agents or with certain diseases. These include: Viral infections Certain bacterial infections, e.g. syphilis Autoimmune diseases, e.g. rheumatoid arthritis, chronic thyroiditis Transplant rejection B. GRANULOMA reaction is a distinct type of chronic inflammation. consisting of three types of cells. It is a focal lesion 1. Epithelioid cells. Macrophages (CD68+) which morphologically resemble epithelial cells. 2. Multinucleated (Langhans) giant cells. Result from the coalescence of macrophage/epithelioid cells. 3. Lymphocytes – Mostly CD4+ and some B cells (CD20+) and plasma cells form a rim around the granuloma. The pathogenesis of most granulomas is immune-mediated (Type IV hypersensitivity), with activated CD4+ T-lymphocytes producing factors (especially gamma-interferon) important in the transformation of CD68+ macrophages into epitheloid and giant cells. Some granulomas, mainly those arising in response to inert foreign bodies, do not appear to be immune-mediated. Differential diagnosis: 1. Tuberculosis (caseating granuloma) 2. Atypical mycobacterial infections 3. Leprosy, cat-scratch disease, brucellosis, lymphogranuloma venereum 4. Fungal infections (especially when longstanding), e.g. histoplasmosis 5. Berylliosis 6. Foreign body 7. Sarcoidosis Disease & Defense Block “Acute and Chronic Inflammation” Page 6 C. SARCOIDOSIS: A disease of unknown etiology with presence of multiple non-caseating granuloma formations (granulomata). Features include: 1. 90% of cases involve the hilar lymph nodes and lungs. Presentation may be as an unexpected finding in a “routine” chest X-ray or a patient with low grade fever and shortness of breath. Other non-specific findings include weight loss, fatigue, and night sweats. 2. Since it can affect virtually any organ or organs in the body it may also present with any of a large variety of clinical manifestations. Sarcoidosis has provided the New England Journal of medicine (NEJM) with many Clinicopathological Conferences (CPCs). It is one of those diseases which is part of almost any differential diagnosis. 3. The diagnosis depends on the demonstration of non-caseating granulomas, e.g. in a bronchial biopsy, in a clinical context compatible with sarcoidosis. In the USA the disease is endemic to the Middle Atlantic states, e.g. North Carolina, and is more common in women and African-Americans. 4. Other sites of involvement include other lymph nodes, spleen, liver, bone marrow, skin and salivary glands. 5. The granulomatous pattern suggests a persistent, poorly degradable antigen. Various immunologic abnormalities are present and CD4+ T-lymphocytes play a role. 6. In most cases the disease is indolent. In a small number of cases it is rapidly progressive and in about 10% of cases the disease is the cause of death. DEFICIENCIES IN THE INFLAMMATORY RESPONSE These inflammatory deficiencies are analogous of the immunodeficiencies and result in increased susceptibility to infection. Some are inherited and others are acquired. These include the leukopenias (e.g. secondary to radiation therapy affecting bone marrow, defects in leukocyte migration (e.g. in diabetes mellitus) and in phagocytosis (e.g. opsonin deficiency). SPECIFIC DISEASES include: 1. Chediak-Higashi disease a) Autosomal recessive b) Infants and children c) Neutropenia with recurrent infections d) Oculocutaneous albinism e) Aberrant granules in Neutrophils and other WBCs – “giant” lysosomes f) Melanocytes – “giant” melanosomes g) Basic defect is unknown – may be in microtubules 2. Chronic granulomatous disease of infancy a) X-linked recessive in most cases, therefore usually in males b) Infants and children c) Recurrent infections, especially by catalase-producing microorganisms d) A variety of histopathologic patterns is seen, especially granulomas e) Basic defect is of NADPH oxidase – resulting in a deficiency of oxygen-dependent generation of H202 and microbial killing. 3. Leukocyte Adhesion Deficiency, Type I a) Inherited b) Children c) Recurrent infections, especially of mucosal surfaces and skin d) Non-specific histopathology e) Basic defect is of leukocyte integrins – beta2 subunit. LFA-1 is a beta2 integrin. Disease & Defense Block “Acute and Chronic Inflammation” Page 7 SYSTEMIC EFFECTS OF INFLAMMATION Non-specific indicators of indicators of inflammation – laboratory tests: 1. “Left-Shift” -- A peripheral blood smear is examined and the percentage of each type of WBC is determined. Some of the neutrophils may show immature types, e.g. “bands” – the immediate precursors of mature neutrophils. The number/percentage of immature neutrophils is increased in certain infections, notably bacterial infections. When the number of immature neutrophils and, especially, if even less mature types are present in the peripheral smear – the term leukemoid reaction is used. 2. Erythrocyte sedimentation rate (ESR) -- The rate at which RBCs “settle” to the bottom of a tube is determined by the amount of protein in the blood. This, in turn, is largely determined by the amount of fibrinogen. The amount of fibrinogen in the blood, and the erythrocyte sedimentation rate (ESR), are increased non-specifically in patients who are undergoing an inflammatory response. 3. C-reactive protein -- Blood levels of this glycoprotein are non-specifically elevated in patients who are undergoing an inflammatory response. It is synthesized by the liver. OTHER TOPICS: - Erosion vs. Ulcer Erosion: A focal defect limited to the epithelial lining or covering e.g. gastric mucosa or epidermis. Ulcer: A focal defect which extends beneath the epithelial lining e.g. to involve the gastric submucosa or dermis. - Fistula vs. sinus tract Fistula: A communication between the lumina of hollow structures (e.g. an acquired communication between two loops of bowel in Crohn’s disease or a congenital malformation – tracheo-esophageal fistula. Fistulae may also communicate between a hollow internal structure and the surface of the skin. Sinus tract: Generally refers to a communication between subcutaneous tissue and the surface of the skin, e.g. pilonidal sinus. “Acute and Chronic Inflammation” Page 8 Disease & Defense Block TERMINOLOGY: Abscess Epithelioid cell Macrophage Acute phase reaction Major basic protein Adhesion molecules ESR Mast cell Monocyte Basophil Fibrin (Fibrinous) Fistula Phagosome Carbuncle Furuncle Phagolysosome C-reactive protein Pseudomembranous C3b, C5a Granuloma Purulent Cellulitis Pyogenic Chediak-Higashi disease ICAM-1 Chemotaxis Integrins Selectins Serous Langhans giant cell Sinus tract Cytokines Leukemoid reaction Suppurative Leukocyte adhesion deficiency Edema Transudate Effusion LFA-1 Erosion Lymphadenitis Ulcer Exudate Lymphangitis Eosinophil Lysosom Chronic granulomatous disease Disclaimers: 1. The primary goal of this chapter is to study the learning objectives outlined at the beginning of this handout. The material to study is provided in the lectures, the handouts and the recommended textbooks. All these sources provide the content over which you will be tested. The lectures are intended to provide broad information of the material found in the textbooks and handouts, and to give the students the opportunity to ask questions on subjects not clear in the texts. The handouts do not seek to follow up the sequence of the lectures, and most importantly, they are not a surrogate of the books. 2. The text presented in this handout has been edited by Dr. La Rosa from material found in your books, from published articles and other educational works. This handout is solely for educational purpose and not intended for commercial or pecuniary benefit (see USA Copyright Law, Section 110, “Limitations on exclusive rights: Exemption of certain performances and displays”). Reproduction and use of this handout can be done only for educational use. [Download] the USA Copyright Law version, October 2009.