High Gleevec Price Offset by Expected Survival Benefit
High Gleevec Price Offset by Expected Survival Benefit
date : 12/13/2004
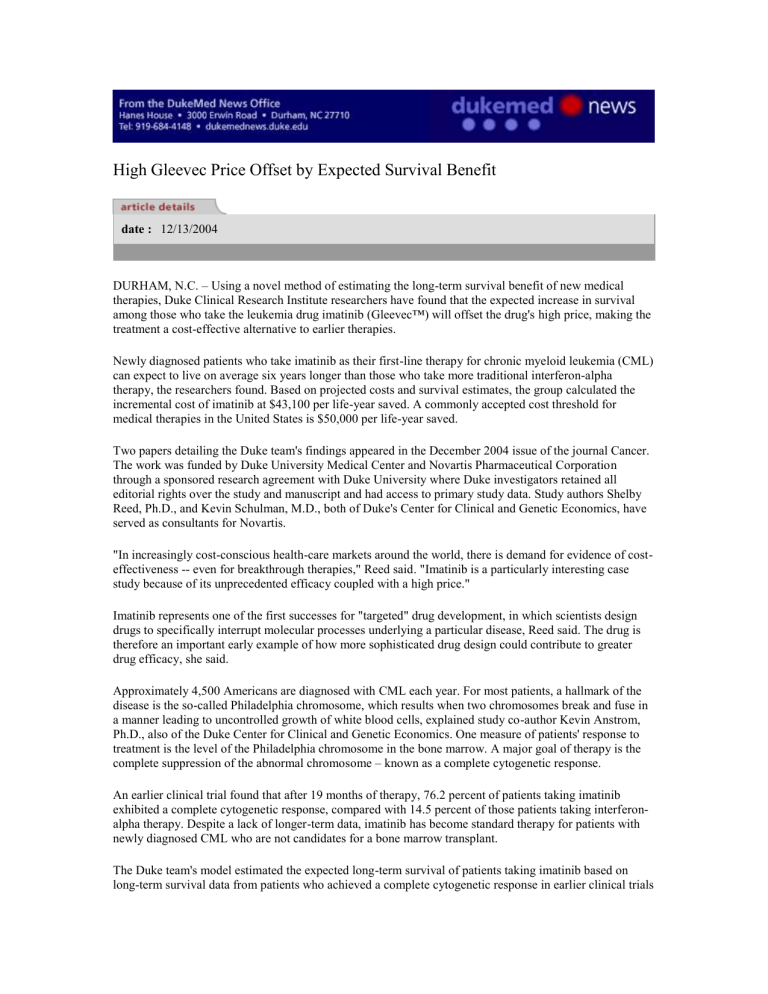
DURHAM, N.C. – Using a novel method of estimating the long-term survival benefit of new medical therapies, Duke Clinical Research Institute researchers have found that the expected increase in survival among those who take the leukemia drug imatinib (Gleevec™) will offset the drug's high price, making the treatment a cost-effective alternative to earlier therapies.
Newly diagnosed patients who take imatinib as their first-line therapy for chronic myeloid leukemia (CML) can expect to live on average six years longer than those who take more traditional interferon-alpha therapy, the researchers found. Based on projected costs and survival estimates, the group calculated the incremental cost of imatinib at $43,100 per life-year saved. A commonly accepted cost threshold for medical therapies in the United States is $50,000 per life-year saved.
Two papers detailing the Duke team's findings appeared in the December 2004 issue of the journal Cancer.
The work was funded by Duke University Medical Center and Novartis Pharmaceutical Corporation through a sponsored research agreement with Duke University where Duke investigators retained all editorial rights over the study and manuscript and had access to primary study data. Study authors Shelby
Reed, Ph.D., and Kevin Schulman, M.D., both of Duke's Center for Clinical and Genetic Economics, have served as consultants for Novartis.
"In increasingly cost-conscious health-care markets around the world, there is demand for evidence of costeffectiveness -- even for breakthrough therapies," Reed said. "Imatinib is a particularly interesting case study because of its unprecedented efficacy coupled with a high price."
Imatinib represents one of the first successes for "targeted" drug development, in which scientists design drugs to specifically interrupt molecular processes underlying a particular disease, Reed said. The drug is therefore an important early example of how more sophisticated drug design could contribute to greater drug efficacy, she said.
Approximately 4,500 Americans are diagnosed with CML each year. For most patients, a hallmark of the disease is the so-called Philadelphia chromosome, which results when two chromosomes break and fuse in a manner leading to uncontrolled growth of white blood cells, explained study co-author Kevin Anstrom,
Ph.D., also of the Duke Center for Clinical and Genetic Economics. One measure of patients' response to treatment is the level of the Philadelphia chromosome in the bone marrow. A major goal of therapy is the complete suppression of the abnormal chromosome – known as a complete cytogenetic response.
An earlier clinical trial found that after 19 months of therapy, 76.2 percent of patients taking imatinib exhibited a complete cytogenetic response, compared with 14.5 percent of those patients taking interferonalpha therapy. Despite a lack of longer-term data, imatinib has become standard therapy for patients with newly diagnosed CML who are not candidates for a bone marrow transplant.
The Duke team's model estimated the expected long-term survival of patients taking imatinib based on long-term survival data from patients who achieved a complete cytogenetic response in earlier clinical trials
of interferon-alpha. The analysis found that leukemia patients taking imatinib as a first-line therapy would survive for an estimated 15.3 years, compared with 9.1 years for those taking interferon-alpha -- an increase of 6.2 years, on average.
After adjusting for quality of life, the patients taking imatinib gained an estimated 5.85 quality-adjusted life years, with an increase in lifetime cost of approximately $241,800, the researchers reported. The researchers estimated the undiscounted lifetime costs of imatinib at $424,600 compared to $182,800 for interferon.
After discounting costs and survival benefits that occur in the future, incremental lifetime costs were found to be $168,100 higher with imatinib, resulting in incremental cost-effectiveness ratios of $43,100 per lifeyear saved and $43,300 per quality-adjusted life year saved.
"Our method is unique in relying on the available scientific evidence to more precisely quantify the survival expectations for patients taking new therapies when long-term data are unavailable," Anstrom said.
"Such survival estimates for imatinib, as well as other drugs, might allow the government to more realistically budget for the long-term costs of therapy."
In many countries, an economic evaluation of new treatments is routinely done, Reed said. While costs are not explicitly incorporated into the current U.S. health care system, the new Medicare prescription drug benefit may one day require data demonstrating the value of outpatient pharmaceuticals to ensure that patients have access to valuable treatments, she said.
Collaborators on the study include Jennifer Ludmer and Andrew Allen, Ph. D., of Duke, and G. Alastair
Glendenning, of Novartis.