ML228 - SharePoint - Erie Community College
advertisement
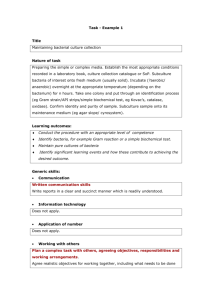
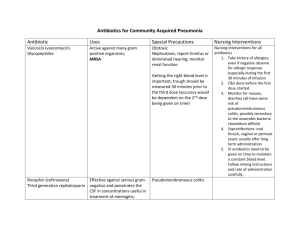
ERIE COMMUNITY COLLEGE NORTH CAMPUS COURSE OUTLINE A. Unit Code and Suggested Course Title: 2188 ML 228-Clinical Microbiology II B. Curriculum/Program: Clinical Laboratory Technician C. Catalog Description: Continuation of ML 218 with the discussion of the pathogenesis and identification of specific microorganisms isolated from clinical specimens according to the ASCP Board of Certification Guidelines for CLT (MLT) curriculum. A taxonomic approach will be used in presenting the groups of microorganisms. Prerequisites: ML 218 and ML 219. Co-requisites: ML 229. S (N) D. Duration of Instructional Period: 50 minutes, 2 class meetings per week, 15 weeks E. Academic Credit Hours: Contact Hours: 2.0 2.0 (2-0-2) F. Suggested Text/ Course Materials: Diagnostic Microbiology: A Study Guide, by Margaret A. Bartelt A Photographic Atlas for the Microbiology Laboratory, by Michael J. Leboffe and Burton E. Pierce Microbiology: Principles and Explorations, by Jacquelyn Black G. Course Outcomes: Upon completion of this course, the student will be able to: 1. 3/08 Collection and Handling of Specimens for Microbiological Examination: a. Describe procedures for appropriate body site sampling and proper time for collection of microbiological specimens. b. State the appropriate collection/transport device for various patient specimens; e.g. throat culture. c. Outline the proper procedures for handling microbiological specimens which may be a possible cause of laboratory acquired infections such as respiratory tract specimens or suspected systemic fungal infections. 1 2. Cultivation and Isolation of Microbes from Patient Specimens: a. State the necessary growth conditions for cultivation of pathogenic microbes. b. List the components of primary plating media and the appropriate use of each type of media. c. State the necessary growth conditions for cultivation of pathogenic microbes from patient specimens. d. Identify the possible bacteria which may be isolated from various types of body specimens. e. Outline the approach to the identification of pathogens including the Gram Stain reaction, biochemical, enzyme, and agglutination tests. 3. Bacterial Pathogens: The following groups of microorganisms will be examined and described according to the characteristics listed below in items a-c: Gram positive cocci, Gram negative aerobic cocci, Gram positive bacilli, Gram positive spore forming bacilli, enteric Gram negative bacilli, Gram negative coccobacilli, spirochetes and other spiral-shaped organisms and non-fermenting Gram negative bacilli. a. Compare and contrast the characteristics of the group of pathogenic microbes listed above in relation to cell and colony morphology, staining, and biochemical reactions. b. Describe symptoms, mode of transmission and virulence characteristics of each organism. c. Outline methods of identification of member genera utilizing specific media, biochemical tests, and culture techniques, including both presumptive and confirmatory tests. The preceding is applied to the following topics – Groups 1 to 9: 1. Gram Negative Enteric Bacteria (Enterobacteriaceae): a. Differentiate between normal intestinal flora, a primary pathogen, and an opportunistic pathogen. b. Define the family Enterobacteriaceae on a morphological and biochemical basis and list the pathogenic members of the family using genus and species designation. c. Identify the reactive component for the individual biochemical media. d. For each genus discussed, the student will complete the following: 1. State the organism’s microscopic morphology. 2. Describe the colony morphology on selective and differential media. 3. Identify the key biochemical reactions of the specific genera belonging to the Enterobacteriaceae family. 4. State the key biochemical reactions to differentiate the species within a genus. 3/08 2 5. Review the pathogenesis of significant enteric microorganisms. e. Describe the antigenic structure of: E. coli, Salmonella, Shigella. f. Define the concept of serologic identification of the enteric bacilli, include antigen and location on the bacterial cell. 2. Non-Fermentative Gram Negative Bacilli: a. State the principle of the oxidative-fermentative test. b. Describe the procedures for the identification of a member of this group such as the oxidase reaction, motility, growth on MacConkey agar and flagella stain. c. Explain how OF Medium may be used to differentiate fermentative, oxidative, and non-saccharolytic organisms. d. Identify significant species of Alcaligenes, Pseudomonas, Burkholderia, Chryseobacterium, Stenotrophomonas, Acinetobacter, and Moraxella 3. Vibrionaceae, Curved Gram Negative Bacilli, and Oxidase Positive Fermenters: Vibrio, Campylobacter, Helicobacter pylori, Aeromonas, and Plesiomonas a. State the significant characteristics of Vibrio cholerae including selective media (TCBS) for isolation, cell morphology, flagellar arrangement, and RBC agglutination. b. Describe the pathogenesis of cholera and how it is effectively treated. c. List the important features of Vibrio parahaemolyticus including disease production and differentiation from V. cholerae. d. State the isolation procedures and identifying traits of Campylobacter jejuni including complex atmospheric conditions, selective media, biochemical tests, and appearance on a direct smear. e. Describe the disease produced by C. jejuni pylori. f. Review the significant features of Helicobacter pylori including laboratory identification, pathogenesis, and treatment of peptic ulcer disease. g. Be able to differentiate Aeromonas hydrophilia and Plesiomonas shigelloides according to growth on selective media, DNase, V-P test, flagellar arrangement, and hemolysis on blood agar h. State how A. hydrophilia and P. shigelloides infections are acquired. 4. Gram Negative Coccobacillary Facultative Bacteria Pasteurella, Francisella, Bordetella, Haemophilus, and Legionella a. Describe the major diseases produced by the genera in this group. b. List the identifying features of the major pathogens including P. multocida, F. tularensis, Bordetella pertussis, and Legionella pneumophila. c. Characterize the significant Haemophilus species according to biochemical testing and “X” and “V” factor requirements. d. State the diseases produced by pathogenic Haemophilus species 5. Aerobic Gram Negative Cocci a. Define the Neisseria on a morphological and biochemical basis. 3/08 3 b. List the pathogenic members of the family Neisseriaceae. c. Differentiate Neisseria gonorrhoeae from Neisseria meningitides and Moraxella (Branhamella) catarrhalis. d. For each member genus and species, the student will complete the following: 1. Characterize specimen collection techniques. 2. Describe culture media procedures for isolation. 3. Outline preliminary identification features (screening). 4. Describe colony morphology variation. 5. List steps for serologic classification 6. Identify key biochemical reactions of the specific species. e. List nonbiochemical identification tests. 3/08 6. Staphylococci and Micrococci: a. Differentiate the Staphylococcus aureus from other staphylococci and micrococci. b. Describe morphology and general characteristics of staphylococci and micrococci. c. Differentiate coagulase negative staphylococci. d. Discuss Staphylococcus aureus regarding its structure and extracellular products. e. List and outline: identification techniques for Staph aureus, Staph epidermidis, and Staph saprophyticus. f. Discuss antibiotic susceptibility of Staph aureus. g, Compare hemolytic differences among these organisms. h. Describe the coagulase test reactions of species listed. i. List the significant ingredients and the results obtainable from the blood agar plate, coagulase test, Mannitol salt agar and DNase test. j. List pathological conditions caused by Staphylococcus aureus. k. State the primary pathological condition caused by: (1) Staphylococcus epidermidis and (2) Staph saprophyticus. List the areas of the human body to which staphylococcus is indigenous. 7. Streptococci, Including Enterococci and Pneumococci: a. Describe the procedure for distinguishing between the genus Staphylococcus and the genus Streptococcus. b. List several species of the genus Streptococcus. c. Classify Streptococci according to their hemolytic reactions on blood agar. d. Outline presumptive identification procedures used for streptococci. e. Discuss epidemiology and pathogenic mechanisms of the genus Streptococcus. f. Describe beta-hemolytic streptococci susceptibility differences to the antibiotic bacitracin or “A” disk test. g. List diseases caused by beta hemolytic Group A Streptococcus. 4 h. Outline and describe the tests or procedures for the identification of Streptococcus pyogenes, Streptococcus agalactiae, Enterococcus faecalis, Streptococcus pneumoniae, and Streptococcus viridans. i. Characterize Lancefield’s serological identification using specific organisms as examples. j. List specific culture media and reagents for the identification of Group A Beta Hemolytic Streptococci (Streptococcus pyogenes). Indicate why identification of a specific streptococcus group necessary for proper antimicrobial therapy and control of some infections. l. Discuss the pathological significance of the capsule. m. Describe differences in optochin susceptibility or “P” disk test in alpha-hemolytic streptococci. n. Differentiate pneumococci from other alpha-hemolytic streptococci. 3/08 8. Gram Positive Bacilli: aerobic spore forming Bacillus, aerobic nonspore forming Corynebacterium, Listeria, and others. a. Characterize the genus Bacillus. b. List the forms of anthrax which can occur in humans. c. Outline identification methods for B. anthracis B.cereus. d. List common genera of the aerobic, non-spore forming group of Gram positive bacilli. e. Discuss epidemiology and pathogenesis of Listerosis. f. Outline laboratory identification of Listeria monocytogenes. g. Characterize the genus Corynebacterium. h. Discuss the term diphtheroid and how it relates to the Corynebacteria. i. Outline isolation procedures of C. diphtheriae from suspected clinical material. j. List type of infections caused by C. diphtheriae and control measures. k. Outline the pathogenesis of Nocardia infection. l. List laboratory identification procedures of Nocardia including microscopic and cultural features. 9. Spirochetes (Treponema, Borrelia, and Leptospira) a. State the main features of the Spirochaetaceae family. b. Be able to describe Treponema, Borrelia, and Leptospira based upon cell morphology. c. State the difficulties associated with Gram staining spirochetes and cultivating in the lab. d. Describe the pathogenesis of infection caused by the various Treponema species. e. List the tests both treponemal and non-treponemal used to identify Treponema pallidum. f. State the main features of Borrelia recurrentis and pathogenesis of relapsing fever. g. Discuss Lyme disease caused by Borrelia burgdorferi including 5 diagnostic procedures. h. Briefly describe the disease and identifying characteristics the disease and identifying characteristics of Leptospira interrogans. i. List the animal reservoirs of Leptosporosis. j. State the important features of Weil’s Syndrome. 10. H. Bioterrorism a. Define the term bioweapon. b. List the significant agents (microorganisms or toxins) which may be potential biological weapons. c. Define the terms that are primary factors of bioweapons including infectivity, pathogenicity, virulence, toxicity, transmissibility, and incubation period. d. Describe the role of the smallpox virus as a potential biological weapon. e. State the mechanisms of disease production by Bacillus anthracis and how it has been used as a bioweapon in the past and present. f. Discuss the role of vaccination in the prevention of smallpox and anthrax outbreaks. g. Give the rationale behind the use of Clostridium botulinum toxin as an effective bioweapon. Program Competencies: Upon graduation with an Associate in Applied Science Degree in Clinical Laboratory Technician, the graduate will be able to: 1. 2. 3. 4. I. Following prescribed procedures, performs routine analytical tests in chemistry, hematology, hemostasis, immunology, immunohematology, and microbiology. (1-9) Recognize abnormal or unusual test results and follow institutional procedures for reporting critical values. (1-9) Perform related work as assigned. (1-10) Demonstrate behavior consistent with acceptable professional conduct standards such as appearance, quality of work, quantity of work, human relation skills, leadership skills, written and verbal communication skills. (1-10) SUNY General Education Knowledge and Skills Areas: Not applicable to course offerings in Health Science Division. J. ECC Learning Outcomes (LO): 1. 2. 3/08 Information Literacy (1-10) Scientific Reasoning (1-10) 6 K. Student Learning: K1. Evaluation of Student Learning: Achievement of the course objectives may be measured by hourly examination, quizzes, selected homework assignments and case study evaluation. The final grade will be calculated as follows: Four exams (each 25%) 100% An optional fifth (cumulative) exam may be administered at the end of the semester which would replace the lowest scored exam. K2. Assessment of Student Learning: The methods of evaluation should be consistent with the level of the course and meet criteria as set forth by the Accreditation Agencies to include cognitive levels, I, II, and III, as well as, affective and psychomotor skills appropriate to the course. L Library Resources: Students are encouraged to read current literature on related topics. Copies of selected current journals are available in the Microbiology laboratory and in the ECC Library. M. Topical Outline: Instructional Units: 3/08 Instructional Periods UNIT I: Introduction to Clinical Microbiology Specimen Collection and Handling 1.0 week UNIT II:. Use of Plating Media for Clinical Specimens 0.5 week UNIT III:. Staphylococci and Micrococci 1.5 weeks UNIT IV: Streptococci, Pneumococci, and Enterococci 1.5 weeks UNIT V: Aerobic Gram Negative Cocci Neisseria species / Moraxella catarrhalis 1.0 week UNIT VI: Enterobacteriaceae E. coli, Shigella, and Salmonella sp.; Proteus, Providencia, and Morganella sp; Serratia, Enterobacter, and Edwardsiella sp.; Yersinia sp. 1.5 weeks UNIT VII: Non Fermentative Gram Negative Bacilli Pseudomonas aeruginosa and Burkholderia sp. Stenotrophomonas maltophilia Chryseobacterium sp. and Alcaligenes faecalis; Acinetobacter and Moraxella sp. 1.0 week 7 UNIT VIII. Miscellaneous Gram Negative Bacilli Pasteurella, Bordetella, and Francisella Vibrio, Campylobacter, and Helicobacter sp. 1.5 weeks UNIT IX. Gram-Negative Coccobacilli Haemophilus species; Gardnerella vaginalis; Legionella pneumophila 1.0 week UNIT X. Gram Positive Bacilli Corynebacterium species; Listeria monocytogenes Bacillus species; Nocardia sp. 1.0 week UNIT XI. Spirochetes Borrelia sp.; Treponema pallidum; Leptospira sp. 1.0 week UNIT XII. Bioterrorism 0.5 week Examination Period N. 3/08 Proposal Prepared by: Date Prepared: Date Last Updated: 2.0 weeks CLT/MA Faculty April 2014 March 2008 8