42a lecture notes
advertisement

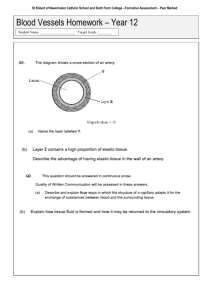
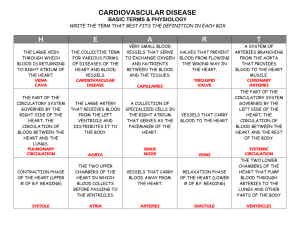
Chapter 42: Circulatory Systems Why Do Animals Need a Circulatory System? • A circulatory system is composed of a pump (heart), fluid (blood), and conduits (blood vessels). • This is also called a cardiovascular system. • The function of the circulatory system is to transport things(oxygen, nutrients, waste etc.) to different parts of the body. Some animals do not have circulatory systems • Single-celled organisms serve all their needs through direct exchange with their environment. • If an organism’s cells are in close proximity to the external environment, nutrients, gases, and wastes can diffuse between the cells, and the environment and a circulatory system is not needed. • Some aquatic animals have a flat body shape or a highly-branched gastrovascular cavity to provide maximum surface area in contact with the environment. • Larger animals and more active animals must support the metabolism of their cells by delivering nutrients to them and taking wastes away from them with circulatory systems. • The critical environment for each cell, where all nutrients are derived and wastes are excreted, is the extracellular fluid that surrounds it. • In open circulatory systems, the extracellular fluid is continuous with the fluid in the circulatory system. Like in insects • In closed circulatory systems, circulating fluid, blood, is completely contained in a continuous system of vessels. • The term extracellular fluid refers to both the fluid in the circulatory system and the fluid between the cells of the body. • Blood plasma is the fluid in the circulatory system. • Interstitial fluid occurs around the cells. • water and low-molecular-weight solutes are exchanged between blood and the intracellular fluids surrounding the cell . Circulatory systems carry materials to and from all regions of the body to maintain the optimum composition of the interstitial fluids and speed up delivery of nutrients to the most active tissues. Open circulatory systems move extracellular fluid • Simple, open circulatory systems squeeze tissue fluid through intercellular spaces. • There is no distinction between tissue fluid and blood, but usually a muscular pump helps propel the fluid, and vessels direct it. • Arthropods and mollusks utilize this system. Closed circulatory systems circulate blood through a system of blood vessels • A closed circulatory system keeps the blood and tissue fluid separate. • One or more muscular hearts and a branching network of vessels (the vascular system) move the blood. • The common earthworm demonstrates this type of circulatory system. • Closed systems have the following advantages over open systems: • Nutrient delivery and waste removal are more rapid due to increased rates of blood flow. • Resistance control by the vessels can selectively direct the blood. • Cellular elements and large molecules that aid in transport of hormones and nutrients can be kept within the vessels. • Closed systems generally support higher levels of metabolic activity than open systems do. • Insects provide an exception to this rule, but they do not rely on their circulatory systems for gas exchange. How Have Vertebrate Circulatory Systems Evolved? • Vertebrates have closed systems with two or more chambers in the heart. • Valves between the chambers, and between the chambers and the vessels, prevent blood backflow when the heart contracts. • A theme in vertebrate circulatory system evolution is progressive separation of blood to the lungs from blood to the rest of the body. • This results in a two-circuit setup: a pulmonary (lung) circuit and a systemic (body) circuit. • Vertebrate systems have arteries to carry blood away from the heart and veins to bring blood back to the heart. • These vessels are connected by thin-walled capillaries through which materials are exchanged between the blood and the tissue fluid. Fish have two-chambered hearts • In fish, there are two chambers: an atrium to receive blood and a ventricle to pump blood. • Blood is first pumped to the gills for gas exchange, then through the aorta to the rest of the body. • Blood collects in the veins after passing the capillary beds and eventually returns to the atrium. • Blood pressure is low in the aorta as the narrow gill spaces dissipate flow force. This limitation does not seem to hamper the fish. Amphibians have three-chambered hearts • Pulmonary and systemic circulation are partly separated in adult amphibians. • As in lungfish, two atria receive blood returning to the heart. • One atrium receives deoxygenated blood from the body; the other receives oxygenated blood from the lungs. • Both atria feed into one ventricle, but anatomical features keep the blood from the two sources mostly separate. • Deoxygenated blood is sent to the lungs; oxygenated blood is sent to the body. • This partial separation of pulmonary and systemic circulation permits delivery of blood through the aorta to the body tissues at a higher pressure than in the fish. Reptiles have exquisite control of pulmonary and systemic circulation • Reptilian hearts have two separate atria and a ventricle that is divided, so mixing of oxygenated and deoxygenated blood is minimized. • Reptiles have a life cycle involving active, high metabolic stages and inactive, low metabolic stages. • This range of demands means that they do not have to breathe continuously. • Some may spend long periods underwater without breathing. • These challenges are met by a bypass of the lung circuit when they are not breathing and the lungs are not needed. • Reptiles have two aortas—a left and a right—and a ventricle that is incompletely divided by a septum. Blood from both sides of the ventricle flows through both aortas to the systemic circuit. • When a reptile is breathing, the resistance in the pulmonary circuit is lower than the resistance in the systemic circuit, so blood from the right side of the ventricle tends to flow into the pulmonary artery then the right aorta. • When a reptile is not breathing, pulmonary vessels constrict, resistance in the pulmonary circuit rises, and blood from the right side of the ventricle tends to flow into the right aorta. • Crocodiles have a true four-chambered heart, but also have two aortas: one aorta originating at the left ventricle and one at the right with a connection between them. • When a crocodile is breathing, backpressure from the stronger left ventricle prevents blood from the right ventricle from entering the right aorta and it flows into the pulmonary circuit instead. • When the animal is not breathing, pulmonary vessels constrict, resistance in the pulmonary circuit rises, and blood from the right ventricle flows into the right aorta. Birds and mammals have fully separated pulmonary and systemic circuits • The four-chambered hearts of birds and mammals completely separate oxygenated and deoxygenated blood. • The advantages of separate circuits are: • Oxygenated and deoxygenated blood cannot mix. • Gas exchange is maximized because the lungs receive only blood with low oxygen content and high CO2 content. • The separate circuits can operate at different pressures. • High pressure is required in the systemic circuit because there are many capillary beds to feed, and these present resistance to blood flow. • The pulmonary circuit has lower resistance and operates at lower pressures. How Does the Mammalian Heart Function? • The left and right sides of the human heart may be thought of as separate pumps. • The left pump delivers blood to the systemic circuit. • The right pump delivers blood to the pulmonary circuit. • Valves (atrioventricular) between the atria and ventricles prevent backflow into the atria when the ventricles contract. • Valves (pulmonary and aortic) positioned between the ventricles and arteries prevent backflow into the ventricles. Blood flows from right heart to lungs to left heart to body • The cycle of blood through the heart begins at the right atrium, which receives blood from two large upper and lower body veins. • From the right atrium, blood goes to the right ventricle. • The right ventricle contracts, sending blood through the pulmonary artery to the lung. • Pulmonary veins return oxygenated blood to the left atrium. • From the left atrium, blood goes to the left ventricle. • The left ventricle contracts, sending blood through the aorta to the body and the capillary beds. • Blood, relieved of its O2 and laden with CO2, returns to the right atrium via veins. • The left ventricle is more muscular because the resistance of the systemic circuit is much greater than that of the pulmonary circuit. • The pumping action of the heart generates the cardiac cycle. • Ventricle contraction is called systole. • Ventricle relaxation is called diastole. • The cardiac cycle can be monitored by the “lub-dup” sound through a stethoscope, noting the closure of heart valves. • Defective valves produce heart murmurs, whooshing sounds following the “lub.” •The cardiac cycle can also be felt in artery pulsation, the surge of blood during systole.The heart rate, also called the pulse is the number of beats per minute • The cardiac output is the volume of blood pumped into the systemic circulation per minute • Blood pressure is the hydrostatic pressure that blood exerts against the wall of a vessel • Systolic pressure is the pressure in the arteries during ventricular systole and is the highest pressure in the arteries • Diastolic pressure is the pressure in the arteries during diastole is lower than systolic pressure Blood pressure may be measured by a stethoscope and a sphygmomanometer, which compares the systolic with diastolic pressure. • A normal young adult might show a systolic pressure of 120 mm of Hg and a diastolic pressure of 70 mm of Hg, or 120/70. Blood pressure is influenced by blood volume and resistance to flow The heartbeat originates in the cardiac muscle • Cardiac muscle cells are in electrical continuity with one another. • This condition permits coordinated contraction for effective blood pumping. • Some cardiac muscle cells initiate action potentials without nervous stimulation, acting as pacemakers. • The primary pacemaker of the heart is the sinoatrial node located at the juncture of the superior vena cava and the right atrium.• • The sympathetic and parasympathetic neurotransmitters control the heart rate • Acetylcholine and norepinephrine from the parasympathetic and sympathetic nerve endings slow and increase the rate, respectively. A conduction system coordinates the contraction of heart muscle • A normal heartbeat begins with an action potential in the sinoatrial node. • The action potential spreads through the atrial cells, causing them to contract in unison. • The ventricles do not contract in unison with the atria because there are no gap junctions between the cells of the atria and ventricles. • The delay in the spread of action potentials through the heart assures that the atria contract before the ventricles do. Electrical properties of ventricular muscles sustain heart contraction The ECG records the electrical activity of the heart • An electrocardiogram (ECG) is a record of electrical events in cardiac muscle during the cardiac cycle. • Electrodes placed on the body surface at different remote locations detect heart action potentials at different times and register a voltage difference. • The ECG is used to diagnose a variety of heart problems. Properties of Blood Vessels?. .Blood circulates throughout the body in a system of blood vessels • Blood leaves the heart in arteries and is distributed in arterioles, which feed capillary beds. • Capillary beds are the sites of exchange of nutrients, wastes, respiratory gases, and hormones. • Blood leaving capillary beds collects in venules, which empty into veins that conduct the blood back to the heart. Arteries-thick wall due to more musculature and Large artery walls are elastic to withstand high pressures and to squeeze blood along their lumens by elastic rebound. • Smooth muscle cells in arteries and arterioles contract and relax, varying their diameters. • This action makes them resistance vessels influenced by neural and hormonal mechanisms. Regulation of resistance influences Blood Pressure. Veins-Thin walls and have valves to prevent backflow.though there is some contraction of vascular smooth muscles, the skeletal muscles help in pushing blood through the veins when they contract. Breathing also helps by creating a negative pressure. Some Properties of Blood. • Blood is connective tissue, so it consists of living cells within an extracellular matrix. Blood is unusual in that the extracellular matrix is a fluid. • The fluid matrix is a straw-colored liquid called plasma. • The cellular components of blood are the red blood cells (erythrocytes), the white blood cells (leukocytes), and the platelets (cell fragments). . Red blood cells transport respiratory gases via hemoglobin Platelets are essential for blood clotting • The platelets contain enzymes and chemicals necessary for blood clotting. • Blood vessel damage exposes collagen fibers, which activate the platelets. • The swelling, sticky platelets activate other platelets and initiate clotting. • Blood clotting involves many chemical steps in a cascade that activates circulating substances in the blood, many of which come from the liver. • Cell damage and platelet activation lead to conversion of an inactive enzyme in the blood, prothrombin, to its active form, thrombin. • Thrombin causes a plasma protein, fibrinogen, to polymerize, forming fibrin threads. • These threads form a meshwork to seal the damaged vessel and provide a base for scar tissue. • Plasma is a complex solution and contains gases, ions, nutrients, proteins, hormones, and vitamins. • Predominant ions are Na+ and Cl–, giving blood a salty taste. • Nutrient molecules in plasma include glucose, amino acids, lipids, lactic acid, and cholesterol. • Circulating proteins include albumin, antibodies, hormones, and carrier molecules. • Plasma is similar in composition to tissue fluid but has a higher concentration of proteins. Materials are exchanged in capillary beds by filtration, osmosis, and diffusion •Capillary beds lie between arterioles and venules and exchange materials between blood and tissue fluid through their thin walls. Two mechanisms regulate the distribution of blood in capillary beds •In one mechanism §Contraction of the smooth muscle layer in the wall of an arteriole constricts the vessel •In a second mechanism §Precapillary sphincters control the flow of blood between arterioles and venules The high-pressure in the arteries is dissipated by the vast number of arterioles and still greater number of capillaries. • The total cross-sectional area of the capillary beds is much greater than that of any of the other vessels; thus pressure is reduced to a very low level. • Capillaries have a very small diameter, and blood flows through them slowly • Capillaries are leaky due to fine holes, called fenestrations, in endothelial cells. •Plasma is similar in composition to tissue fluid but has a higher concentration of proteins Circulating proteins include albumin, antibodies, hormones, and carrier molecules. • Many small molecules leak through, but larger protein molecules are held back. • This process, called filtration, creates a difference in osmotic potential between the plasma and tissue fluid. • The end result is to draw water back into the capillary. • Blood pressure on the arterial side of the capillary bed squeezes water out, but the osmotic pressure increase pulls it back at the venous end. • These two opposing forces are known as Starling’s forces, after the work of the physiologist E. H. Starling. Starling named the second force, at the venous end of the capillaries, colloidal osmotic pressure. • Actually, CO2 and bicarbonate ions (HCO3–) are major factors that pull water back into the capillaries. • As blood flows through the capillary, CO2 diffuses into the plasma and is converted into HCO3–. • The increasing bicarbonate concentration causes osmotic pressure to be higher. • Lipid-soluble substances and many small molecules can pass easily through capillary walls down their concentration gradients. . Vascular disease is a killer • Heart disease accounts for almost half the deaths in the United States and Europe in any single year. • Heart attack or stroke is often the end result of atherosclerosis (hardening of arteries). • When the smooth internal lining of arteries becomes damaged, deposits called plaque form at damaged sites. • Swelling and lipid (especially cholesterol) deposition invite fibrous connective tissue and calcium deposits. • These make the artery wall less elastic (“hardening”), and the plaque narrows the lumen of the artery. • Blood platelets stick in the plaque and form blood clots (a thrombus), further blocking the artery. • If the heart arteries (coronaries) are affected, blood supply to the heart decreases. • A thrombus here could block the artery, causing a heart attack (myocardial infarction, or MI). • If part of the thrombus breaks loose (an embolism), lodges in the brain, and blocks blood flow, a stroke may occur. • The best approach to reducing heart disease is prevention. • Genetic predisposition is a major factor in addition to environmental risk. • Risk factors include high-fat/high-cholesterol diets, smoking, a sedentary life style, and obesity. How Is the Circulatory System Controlled and Regulated? • Neural and hormonal mechanisms control the circulatory system at local and systemic levels. • Each tissue, however, regulates its own blood flow by autoregulatory mechanisms that constrict or dilate arterioles supplying blood. Autoregulation matches local blood flow to local need • When arteriole blood flows into a capillary bed, smooth muscle in the arteriole may constrict or relax by means of precapillary sphincters. • Low O2 and high CO2 levels cause the smooth muscle to relax and flood the capillary bed. • Any activities that increase metabolism of the tissue also increase blood flow to the tissue. Arterial pressure is controlled and regulated by hormonal and neuronal mechanisms Blood pressure (BP) is determined partly by cardiac output and partly by peripheral resistance due to variable constriction of the arterioles Arteriole smooth muscle also responds to endocrine and neural signals. • The sympathetic division of the autonomic nervous system (ANS) innervates most arteries and arterioles.releasing epinephrine that can cause arterioles to constrict or in skeletal muscles arterioles acytylcholine is released which causes relaxation like the parasympathetic division of the ANS. • Stretch receptors (also called baroreceptors) in the aorta and carotid artery provide information about blood pressure. • ADH is an antidiuretic hormone secreted by the posterior pituitary in response to a fall in baroreceptor activity. • ADH helps to stabilize blood pressure by causing the kidneys to absorb more water and thereby maintain blood volume. • Baroreceptors inhibits release of ADH ahich is also called vasopressin as it constricts blood vessels and increases BP Also when arterial pressure falls kidney releases renin which in turn converts angiotensinogen into angiotensin which constricts the arteries increasing BP When atria are receiving too much venous return they release a hormone called atrial natriuretic factor, which stimulates the kidney to excrete sodium and water, resulting in a reduced blood volume Cardiovascular control in diving mammals conserves oxygen • Several adaptations permit the air-breathing seal to remain under water for long periods. • The O2 storage capacity of seals is double that of humans because of greater blood volume. • Seals have a greater blood O2 carrying capacity and more myoglobin in their muscles. • The diving reflex is the most important adaptation. • This reflex slows the heart and constricts all major blood vessels except those critical to survival under water (heart, nervous system, eyes). • Central blood pressure remains high but blood flow to tissues decreases. • This triggers a switch to glycolytic (anaerobic) metabolism and overall tissue metabolism suppression. • The “oxygen debt” built up is paid back after the dive is over, but the hypometabolism during the dive has kept the debt small.